Recently, some countries have shown stable trends in lung cancer death rates among women not yet described for Spain. We propose to update lung cancer mortality rates in Spain during the period of 1980–2018 by sex and region.
MethodsWe used lung cancer mortality (International Classification of Diseases code 162 for the 9th edition, and codes C33 and C34 for 10th edition) and population data from the Spanish National Statistics Institute for the period 1980–2018. Age-standardised mortality rates (ASMRs), all ages and 30–64 years, by region and sex were assessed through joinpoint regression.
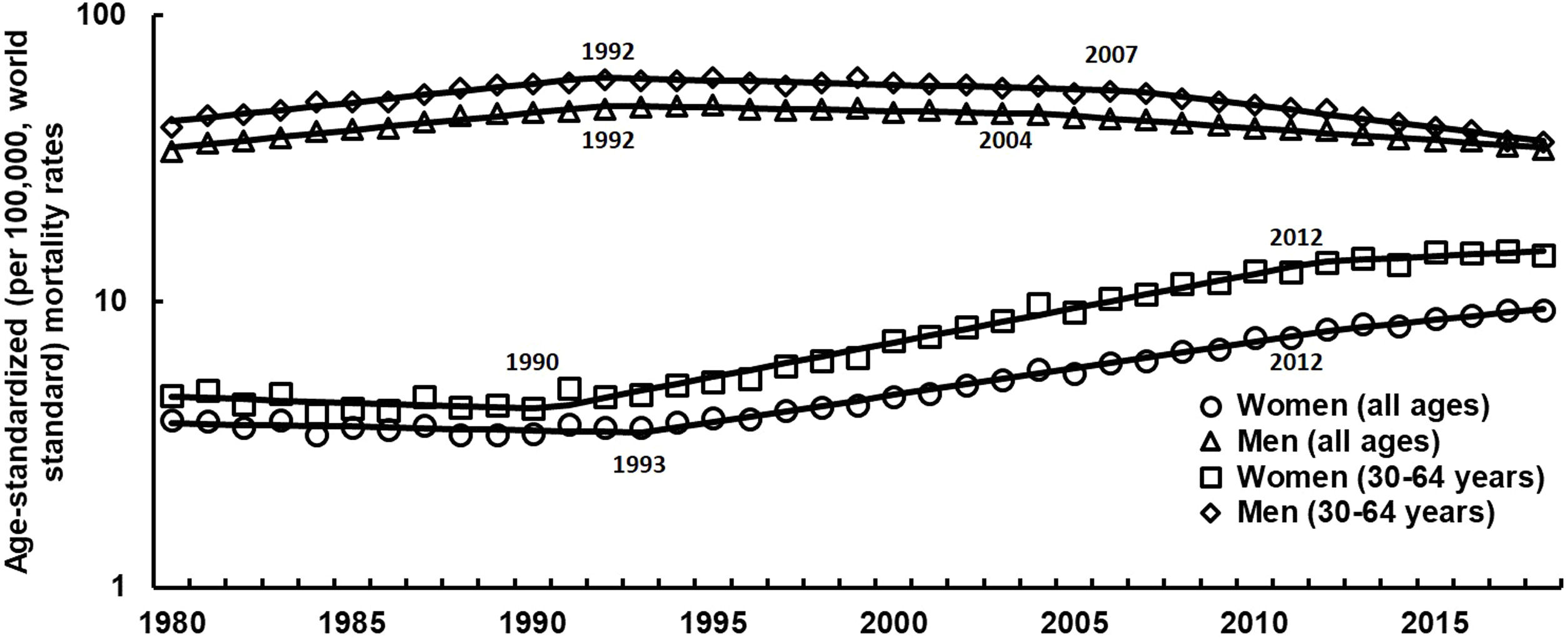
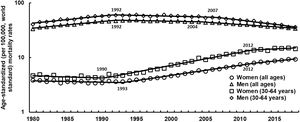
ResultsDuring the study period lung cancer ASMRs (all ages) in men decreased -0.4% per annum and increased by 3.1% in women. Recently, ASMR (30–64 years) accelerated its decrease (1992–2007; −0.7 and 2007–2018; −3.5%) in men and slowed its increase (1990–2012; 5.7% and 2012–2018; 1.4%) in women. In men, joinpoint analysis detected an initial period in all Autonomous Communities (ACs) in which the rates significantly increased, followed by a second period in which the rates decreased significantly (12 ACs) or remained stable (4 ACs) since the late 1980s or early 1990s. In women, upward trends in ASMRs (all ages) were observed for the whole period in all the ACs. In 13 ACs, an initial period was detected with joinpoint in which the rates remained stable or significantly decreased, followed by a second period in which the rates increased significantly since the late 1980s or early 1990s.
ConclusionsOur study shows gender differences in lung cancer mortality trends in Spain. These differences may be explained by the increased use of tobacco among women and the decreased use among men.
Recientemente, algunos países han mostrado tendencias estables en las tasas de mortalidad por cáncer de pulmón entre las mujeres que aún no se han descrito para España. Proponemos actualizar las tasas de mortalidad por cáncer de pulmón en España durante el período 1980-2018 por sexo y región.
MétodosUtilizamos la mortalidad por cáncer de pulmón (código 162 de la Clasificación Internacional de Enfermedades según la novena edición, y los códigos C33 y C34 según la décima edición) y los datos poblacionales del Instituto Nacional de Estadística de España para el período 1980-2018. Las tasas específicas de mortalidad por edad (TEME), para todas las edades y entre los 30 y 64 años, por región y sexo, se evaluaron mediante el análisis de regresión por segmentos.
ResultadosDurante el período de estudio, la TEME (todas las edades) de cáncer de pulmón disminuyó un −0,4% por año en hombres y aumentó un 3,1% en mujeres. Recientemente, la TEME (30-64 años) aceleró su descenso (1992-2007: −0,7% y 2007-2018: −3,5%) en los hombres y desaceleró su aumento (1990-2012: 5,7% y 2012-2018: 1,4%) en las mujeres. En los hombres, el análisis de regresión por segmentos detectó un período inicial en todas las comunidades autónomas (CA) en el que las tasas aumentaron significativamente, seguido de un segundo período en el que las tasas disminuyeron significativamente (12 CA) o se mantuvieron estables (4 CA) desde finales de la década de los ochenta o principios de los noventa. En las mujeres, las tendencias al alza en la TEME (todas las edades) se observaron durante todo el período en todas las CA. En 13 CA, se detectó con el análisis de regresión un período inicial en el que las tasas se mantuvieron estables o disminuyeron significativamente, seguido de un segundo período en el que las tasas aumentaron significativamente desde finales de los años ochenta o principios de los noventa.
ConclusionesNuestro estudio muestra diferencias de género en las tendencias de mortalidad por cáncer de pulmón en España. Estas diferencias pueden explicarse por el aumento del uso de tabaco en las mujeres y la disminución del uso entre los hombres.
Lung cancer is one of the main public health problems today and, with an estimated 2.1 million new cases and 1.8 million deaths, remains the leading cause of cancer incidence and mortality worldwide (2018).1
In the European Union (EU) in 2019, lung cancer has the highest predicted age-standardized cancer mortality rate in both sexes (32.3/100,000 men and 14.8/100,000 women) corresponding to 183,200 and 96,800 predicted deaths in men and women respectively (23% of total men cancer deaths and 16% of total women cancer deaths).2
The declines in lung cancer mortality rates in EU men since the late 1980s have continued over recent years3 and are projected to persist for the near future.4 In women, although rates are still appreciably lower than those for men, steady upward trends have been observed since the 1970s (for generations born in the 1950s and 1960s) or even earlier in some countries through the first decade of the 2000s5 and is expected to increase over time.2 European countries where women started smoking earlier showed higher lung cancer rates also earlier.6,7 However, despite this general trend, in some countries (where rises were earlier and mortality rates were higher) there has been a leveling off in overall rates8 and a decrease in middle-aged and young women.9 Notably, one in 7 deaths in Spain in 2016 were attributable to smoking in Spain.10
In previous reports, we thoroughly analyzed lung cancer mortality trends in Spain (as a whole)11,12 and in Andalusia (the second largest Spanish autonomous community)13,14 showing that although mortality rates began to decrease slightly among men in the 1990s, they increased significantly among women during the same period (and are expected to increase over the next years),15,16 with a decrease in the male-to-female mortality ratio. Notwithstanding, there are no reports analyzing trends in lung cancer mortality by sex and Autonomous Communities (ACs).17
Monitoring lung cancer mortality trends in Spain by autonomous communities can offer an interesting image from an epidemiological and public health perspective, since Spanish women started smoking later than their European counterparts.18,19 Supporting the design and evaluation of public health interventions, as well as for the evaluation of treatment effectiveness. Therefore, we propose to update and refine the earlier assessments of lung cancer mortality rates in Spain during the period of 1980–2018 by sex and ACs.
MethodsData sourceData on population and lung cancer death records (International Classification of Diseases code 162 for the 9th edition, and codes C33 and C34 for 10th edition) were retrieved from the National Institute of Statistics for the study period (1980–2018). Intercensal populations were estimated on 1 July of each year based on official census information.
Statistical analysisSpain is administratively divided in 17 regions called autonomous communities. Individual records broken down by sex, age, year of death and autonomous community of residence were used to compute age-standardized rates (ASR) per 100,000 women, at all ages and truncated 30–64 years (using the World standard population by the direct method) and expressed as rates per 100,000 person-years.
Trends were analyzed using joinpoint (segmented) regression software.20 This helped to identify inflection points (so-called joinpoints) where a significant change in linear slope of the trend occurred, according to the method proposed by Kim et al.21 This method uses a statistical algorithm to define a best-fitting regression line through mortality data across time, determining how many, if any, joinpoints should be used to determine where significant changes take place. Tests of significance used a Monte Carlo permutation method with 4499 replicates. The models incorporate variation using the standard error of the rate; the annual percentage change (APC) for each segment is estimated by fitting a regression line to the natural logarithm of the rate, using calendar year as an independent variable.22 The analysis began with the minimum number of joinpoints (e.g. 0 joinpoint, representing a straight line) and tested whether one or more joinpoints were significant.
To quantify the trend over the whole period, we computed the average annual percent change (AAPC) as a geometrically weighted average of the various APCs from the joinpoint regression analysis, with weights being equivalent to the length of each segment during the specified time interval.22 This represented a summary measure of the trend over the study period (1980–2018). If an AAPC lied entirely within a single joinpoint segment, the AAPC was equal to the APC for that segment. To determine the direction and magnitude of recent trends, AAPCs were also evaluated for the last available 10 years (2009–2018).
We allowed a maximum of two joinpoints and an associated p<0.05 represented the likelihood that the APC or AAPC was significantly different from zero. In describing the trend analysis results, the terms “increase” or “decrease” indicate statistical significance (p<0.05), while non-significant results are reported as “stable”. All analyses were performed using the Joinpoint Regression Program, Version 4.7.0.0.
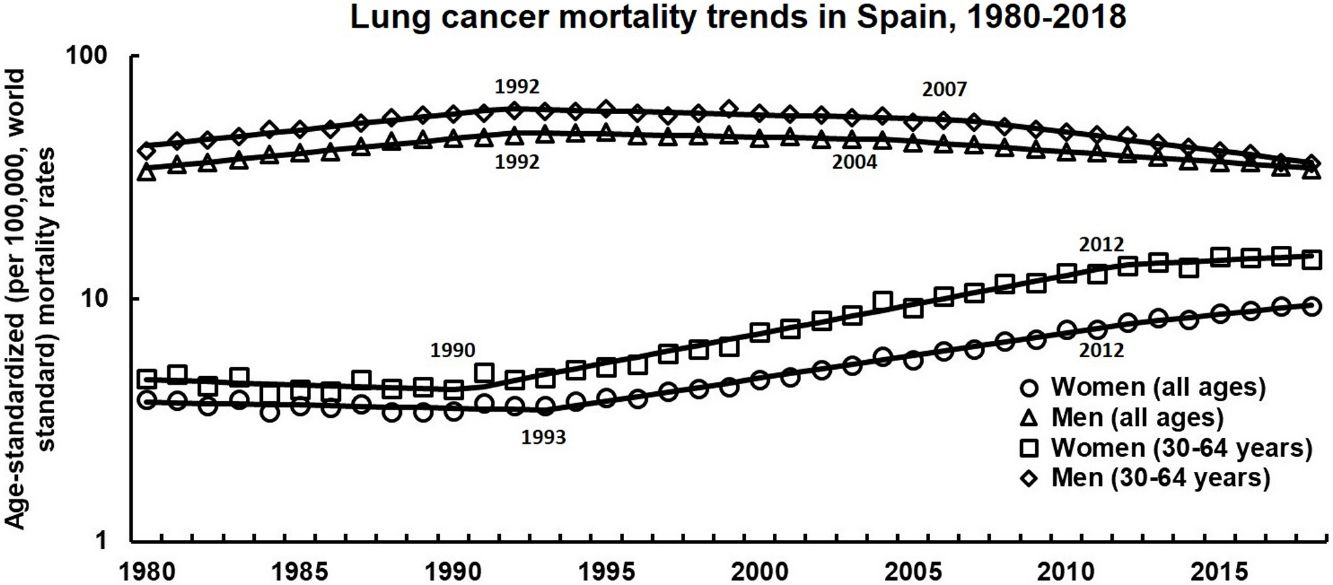
ResultsOverall and truncated (30–64 years) ASMRs due to lung cancer in men and women (1980–2018) are illustrated in Fig. 1. Lung cancer ASMRs (all ages) in men changed during the study period from 33.5/100,000 in 1980 to 34.2 in the year 2018, with an average annual decrease of −0.4% (p<0.05). However, joinpoint analysis identified three time periods: an initial period of statistically significant increase (1980–1992 APC: 2.9%, p<0.05) and two period of decrease in rates (1992–2004: −0.5% per year, p<0.05 and 2004–2018: −1.9%, p<0.05). Something similar is observed in ASMRs (30–64 years), although in the last period the rates accelerate their decline (2007–2018; −3.5%, p<0.05). In women, lung cancer ASMRs (all ages) changed during the study period from 3.9/100,000 in 1980 to 9.3/100,000 in the year 2018, with an average annual increase of 3.1% (p<0.05). However, joinpoint analysis identified three time periods: an initial period with a statistically significant decrease (1980–1993; −0.6%), and two periods of rate increases (1993–2012; 4.4%, p<0.05 and 2012–2018; 3.0%, p<0.05). Something similar is observed in the ASMRs (30–64 years), although in the last period the rates slowed down (2012–2018; 1.4%, p<0.05).
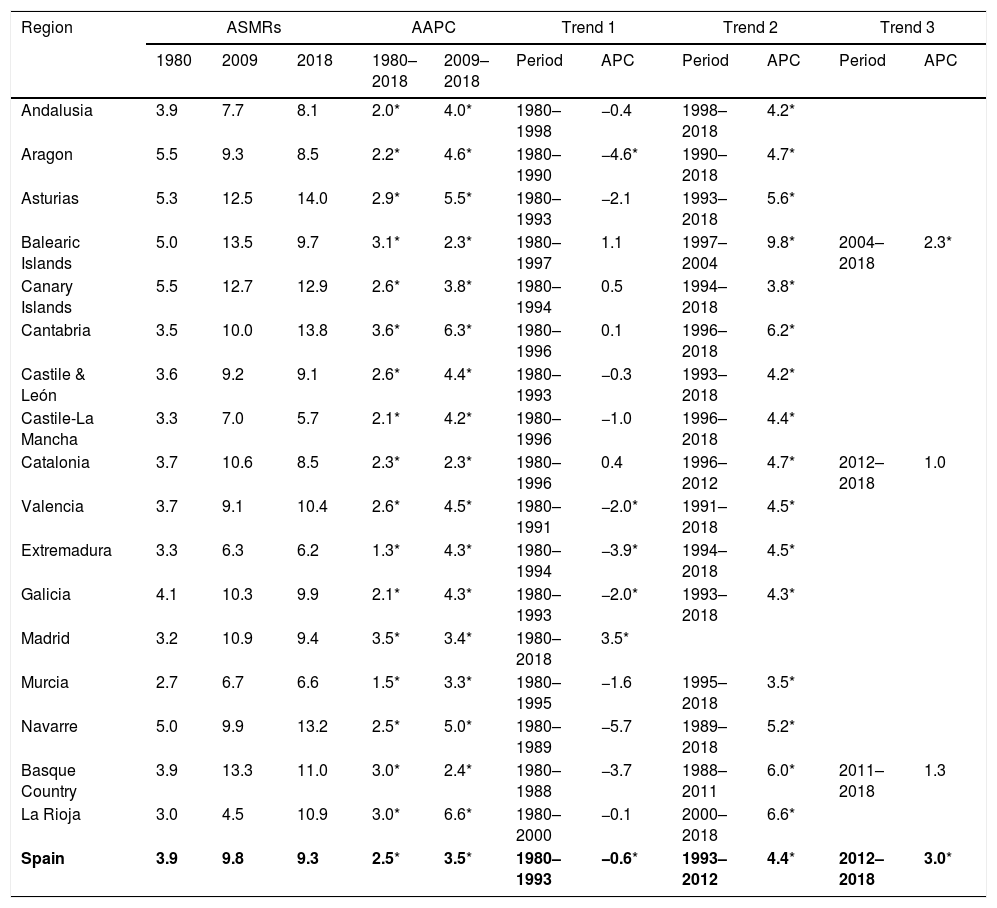
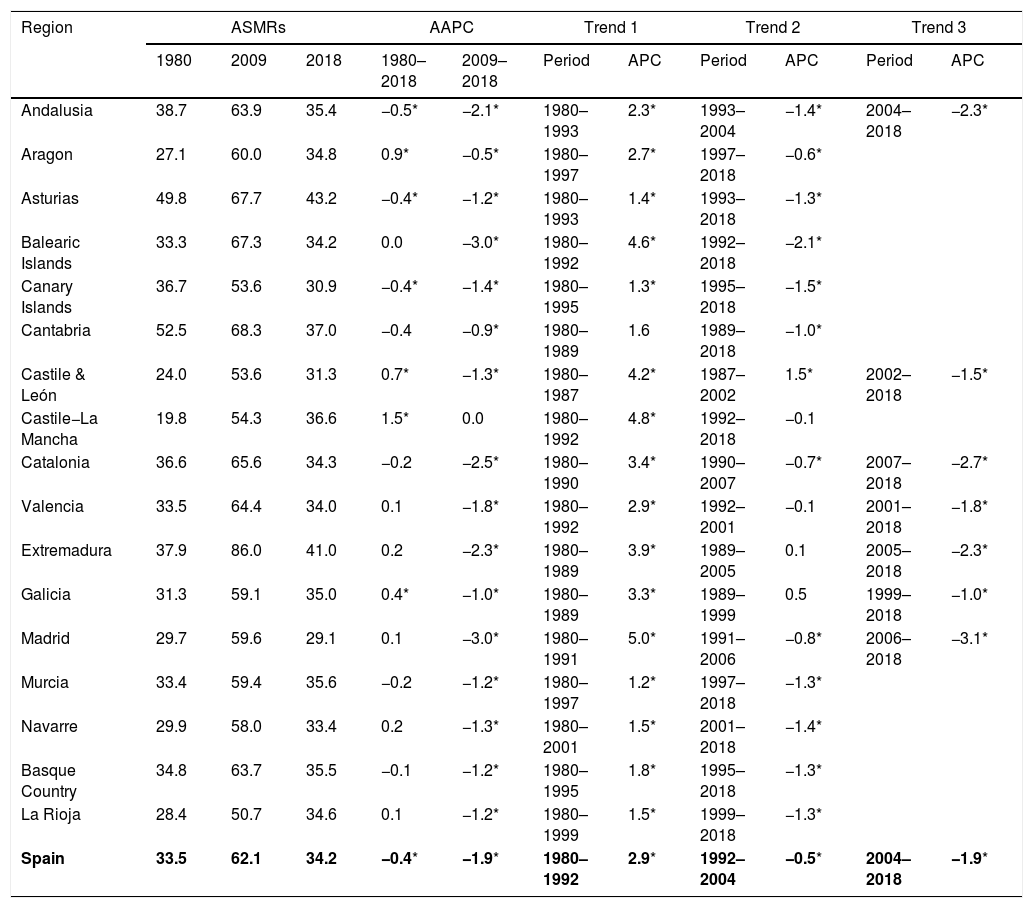
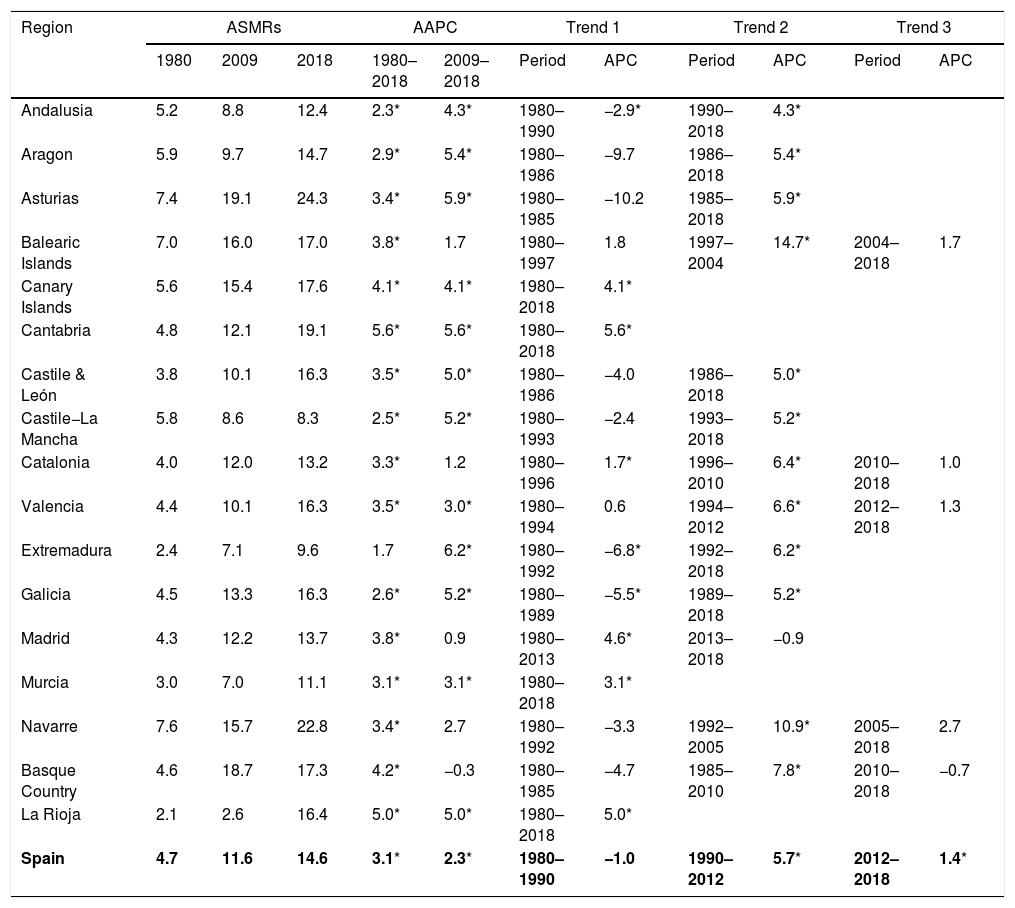
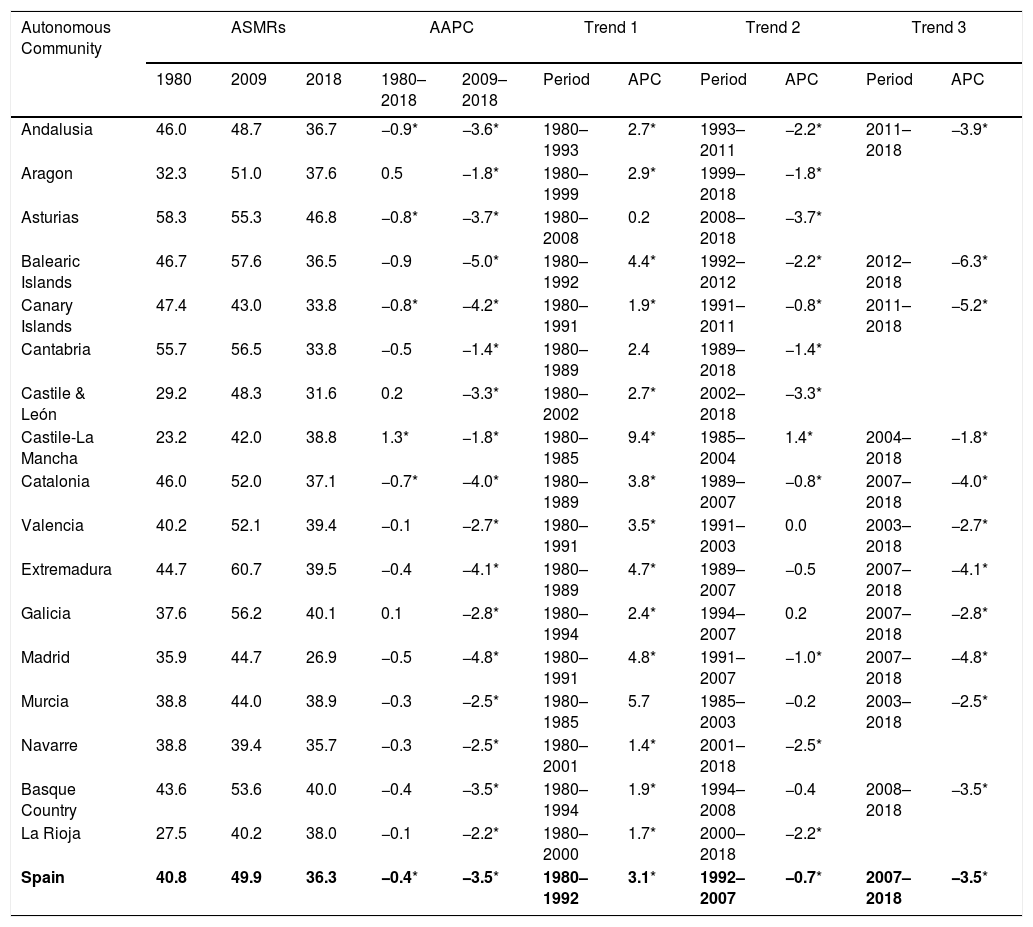
Tables 1–4 show ASMRs (all ages and 30–64 years) for the years 1980, 2009 and 2018, the AAPCs for the entire study period (1980–2018) and the last ten years (2009–2018), and the results of the joinpoint regression analysis (i.e. the points in which rates changed significantly) and the APC for each trend by sex and Autonomous Community.
Age-standardized per 100,000 (world standard population) mortality rates and joinpoint results. Women (all ages) Spain 1980–2018.
| Region | ASMRs | AAPC | Trend 1 | Trend 2 | Trend 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1980 | 2009 | 2018 | 1980–2018 | 2009–2018 | Period | APC | Period | APC | Period | APC | |
| Andalusia | 3.9 | 7.7 | 8.1 | 2.0* | 4.0* | 1980–1998 | −0.4 | 1998–2018 | 4.2* | ||
| Aragon | 5.5 | 9.3 | 8.5 | 2.2* | 4.6* | 1980–1990 | −4.6* | 1990–2018 | 4.7* | ||
| Asturias | 5.3 | 12.5 | 14.0 | 2.9* | 5.5* | 1980–1993 | −2.1 | 1993–2018 | 5.6* | ||
| Balearic Islands | 5.0 | 13.5 | 9.7 | 3.1* | 2.3* | 1980–1997 | 1.1 | 1997–2004 | 9.8* | 2004–2018 | 2.3* |
| Canary Islands | 5.5 | 12.7 | 12.9 | 2.6* | 3.8* | 1980–1994 | 0.5 | 1994–2018 | 3.8* | ||
| Cantabria | 3.5 | 10.0 | 13.8 | 3.6* | 6.3* | 1980–1996 | 0.1 | 1996–2018 | 6.2* | ||
| Castile & León | 3.6 | 9.2 | 9.1 | 2.6* | 4.4* | 1980–1993 | −0.3 | 1993–2018 | 4.2* | ||
| Castile-La Mancha | 3.3 | 7.0 | 5.7 | 2.1* | 4.2* | 1980–1996 | −1.0 | 1996–2018 | 4.4* | ||
| Catalonia | 3.7 | 10.6 | 8.5 | 2.3* | 2.3* | 1980–1996 | 0.4 | 1996–2012 | 4.7* | 2012–2018 | 1.0 |
| Valencia | 3.7 | 9.1 | 10.4 | 2.6* | 4.5* | 1980–1991 | −2.0* | 1991–2018 | 4.5* | ||
| Extremadura | 3.3 | 6.3 | 6.2 | 1.3* | 4.3* | 1980–1994 | −3.9* | 1994–2018 | 4.5* | ||
| Galicia | 4.1 | 10.3 | 9.9 | 2.1* | 4.3* | 1980–1993 | −2.0* | 1993–2018 | 4.3* | ||
| Madrid | 3.2 | 10.9 | 9.4 | 3.5* | 3.4* | 1980–2018 | 3.5* | ||||
| Murcia | 2.7 | 6.7 | 6.6 | 1.5* | 3.3* | 1980–1995 | −1.6 | 1995–2018 | 3.5* | ||
| Navarre | 5.0 | 9.9 | 13.2 | 2.5* | 5.0* | 1980–1989 | −5.7 | 1989–2018 | 5.2* | ||
| Basque Country | 3.9 | 13.3 | 11.0 | 3.0* | 2.4* | 1980–1988 | −3.7 | 1988–2011 | 6.0* | 2011–2018 | 1.3 |
| La Rioja | 3.0 | 4.5 | 10.9 | 3.0* | 6.6* | 1980–2000 | −0.1 | 2000–2018 | 6.6* | ||
| Spain | 3.9 | 9.8 | 9.3 | 2.5* | 3.5* | 1980–1993 | −0.6* | 1993–2012 | 4.4* | 2012–2018 | 3.0* |
ASMR, age-standardized mortality rates using the world standard population; AAPC: average annual percent change; APC: annual percentage change.
Age-standardized per 100,000 (world standard population) mortality rates and joinpoint results. Men (all ages) Spain 1980–2018.
| Region | ASMRs | AAPC | Trend 1 | Trend 2 | Trend 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1980 | 2009 | 2018 | 1980–2018 | 2009–2018 | Period | APC | Period | APC | Period | APC | |
| Andalusia | 38.7 | 63.9 | 35.4 | −0.5* | −2.1* | 1980–1993 | 2.3* | 1993–2004 | −1.4* | 2004–2018 | −2.3* |
| Aragon | 27.1 | 60.0 | 34.8 | 0.9* | −0.5* | 1980–1997 | 2.7* | 1997–2018 | −0.6* | ||
| Asturias | 49.8 | 67.7 | 43.2 | −0.4* | −1.2* | 1980–1993 | 1.4* | 1993–2018 | −1.3* | ||
| Balearic Islands | 33.3 | 67.3 | 34.2 | 0.0 | −3.0* | 1980–1992 | 4.6* | 1992–2018 | −2.1* | ||
| Canary Islands | 36.7 | 53.6 | 30.9 | −0.4* | −1.4* | 1980–1995 | 1.3* | 1995–2018 | −1.5* | ||
| Cantabria | 52.5 | 68.3 | 37.0 | −0.4 | −0.9* | 1980–1989 | 1.6 | 1989–2018 | −1.0* | ||
| Castile & León | 24.0 | 53.6 | 31.3 | 0.7* | −1.3* | 1980–1987 | 4.2* | 1987–2002 | 1.5* | 2002–2018 | −1.5* |
| Castile−La Mancha | 19.8 | 54.3 | 36.6 | 1.5* | 0.0 | 1980–1992 | 4.8* | 1992–2018 | −0.1 | ||
| Catalonia | 36.6 | 65.6 | 34.3 | −0.2 | −2.5* | 1980–1990 | 3.4* | 1990–2007 | −0.7* | 2007–2018 | −2.7* |
| Valencia | 33.5 | 64.4 | 34.0 | 0.1 | −1.8* | 1980–1992 | 2.9* | 1992–2001 | −0.1 | 2001–2018 | −1.8* |
| Extremadura | 37.9 | 86.0 | 41.0 | 0.2 | −2.3* | 1980–1989 | 3.9* | 1989–2005 | 0.1 | 2005–2018 | −2.3* |
| Galicia | 31.3 | 59.1 | 35.0 | 0.4* | −1.0* | 1980–1989 | 3.3* | 1989–1999 | 0.5 | 1999–2018 | −1.0* |
| Madrid | 29.7 | 59.6 | 29.1 | 0.1 | −3.0* | 1980–1991 | 5.0* | 1991–2006 | −0.8* | 2006–2018 | −3.1* |
| Murcia | 33.4 | 59.4 | 35.6 | −0.2 | −1.2* | 1980–1997 | 1.2* | 1997–2018 | −1.3* | ||
| Navarre | 29.9 | 58.0 | 33.4 | 0.2 | −1.3* | 1980–2001 | 1.5* | 2001–2018 | −1.4* | ||
| Basque Country | 34.8 | 63.7 | 35.5 | −0.1 | −1.2* | 1980–1995 | 1.8* | 1995–2018 | −1.3* | ||
| La Rioja | 28.4 | 50.7 | 34.6 | 0.1 | −1.2* | 1980–1999 | 1.5* | 1999–2018 | −1.3* | ||
| Spain | 33.5 | 62.1 | 34.2 | −0.4* | −1.9* | 1980–1992 | 2.9* | 1992–2004 | −0.5* | 2004–2018 | −1.9* |
ASMR, age-standardized mortality rates using the world standard population; AAPC: average annual percent change; APC: annual percentage change.
Age-standardized per 100,000 (world standard population) mortality rates and joinpoint results. Women (30–64 years) Spain 1980–2018.
| Region | ASMRs | AAPC | Trend 1 | Trend 2 | Trend 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1980 | 2009 | 2018 | 1980–2018 | 2009–2018 | Period | APC | Period | APC | Period | APC | |
| Andalusia | 5.2 | 8.8 | 12.4 | 2.3* | 4.3* | 1980–1990 | −2.9* | 1990–2018 | 4.3* | ||
| Aragon | 5.9 | 9.7 | 14.7 | 2.9* | 5.4* | 1980–1986 | −9.7 | 1986–2018 | 5.4* | ||
| Asturias | 7.4 | 19.1 | 24.3 | 3.4* | 5.9* | 1980–1985 | −10.2 | 1985–2018 | 5.9* | ||
| Balearic Islands | 7.0 | 16.0 | 17.0 | 3.8* | 1.7 | 1980–1997 | 1.8 | 1997–2004 | 14.7* | 2004–2018 | 1.7 |
| Canary Islands | 5.6 | 15.4 | 17.6 | 4.1* | 4.1* | 1980–2018 | 4.1* | ||||
| Cantabria | 4.8 | 12.1 | 19.1 | 5.6* | 5.6* | 1980–2018 | 5.6* | ||||
| Castile & León | 3.8 | 10.1 | 16.3 | 3.5* | 5.0* | 1980–1986 | −4.0 | 1986–2018 | 5.0* | ||
| Castile−La Mancha | 5.8 | 8.6 | 8.3 | 2.5* | 5.2* | 1980–1993 | −2.4 | 1993–2018 | 5.2* | ||
| Catalonia | 4.0 | 12.0 | 13.2 | 3.3* | 1.2 | 1980–1996 | 1.7* | 1996–2010 | 6.4* | 2010–2018 | 1.0 |
| Valencia | 4.4 | 10.1 | 16.3 | 3.5* | 3.0* | 1980–1994 | 0.6 | 1994–2012 | 6.6* | 2012–2018 | 1.3 |
| Extremadura | 2.4 | 7.1 | 9.6 | 1.7 | 6.2* | 1980–1992 | −6.8* | 1992–2018 | 6.2* | ||
| Galicia | 4.5 | 13.3 | 16.3 | 2.6* | 5.2* | 1980–1989 | −5.5* | 1989–2018 | 5.2* | ||
| Madrid | 4.3 | 12.2 | 13.7 | 3.8* | 0.9 | 1980–2013 | 4.6* | 2013–2018 | −0.9 | ||
| Murcia | 3.0 | 7.0 | 11.1 | 3.1* | 3.1* | 1980–2018 | 3.1* | ||||
| Navarre | 7.6 | 15.7 | 22.8 | 3.4* | 2.7 | 1980–1992 | −3.3 | 1992–2005 | 10.9* | 2005–2018 | 2.7 |
| Basque Country | 4.6 | 18.7 | 17.3 | 4.2* | −0.3 | 1980–1985 | −4.7 | 1985–2010 | 7.8* | 2010–2018 | −0.7 |
| La Rioja | 2.1 | 2.6 | 16.4 | 5.0* | 5.0* | 1980–2018 | 5.0* | ||||
| Spain | 4.7 | 11.6 | 14.6 | 3.1* | 2.3* | 1980–1990 | −1.0 | 1990–2012 | 5.7* | 2012–2018 | 1.4* |
ASMR, age-standardized mortality rates using the world standard population; AAPC: average annual percent change; APC: annual percentage change.
Age-standardized per 100,000 (world standard population) mortality rates and joinpoint results. Men (30–64 years) Spain 1980–2018.
| Autonomous Community | ASMRs | AAPC | Trend 1 | Trend 2 | Trend 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1980 | 2009 | 2018 | 1980–2018 | 2009–2018 | Period | APC | Period | APC | Period | APC | |
| Andalusia | 46.0 | 48.7 | 36.7 | −0.9* | −3.6* | 1980–1993 | 2.7* | 1993–2011 | −2.2* | 2011–2018 | −3.9* |
| Aragon | 32.3 | 51.0 | 37.6 | 0.5 | −1.8* | 1980–1999 | 2.9* | 1999–2018 | −1.8* | ||
| Asturias | 58.3 | 55.3 | 46.8 | −0.8* | −3.7* | 1980–2008 | 0.2 | 2008–2018 | −3.7* | ||
| Balearic Islands | 46.7 | 57.6 | 36.5 | −0.9 | −5.0* | 1980–1992 | 4.4* | 1992–2012 | −2.2* | 2012–2018 | −6.3* |
| Canary Islands | 47.4 | 43.0 | 33.8 | −0.8* | −4.2* | 1980–1991 | 1.9* | 1991–2011 | −0.8* | 2011–2018 | −5.2* |
| Cantabria | 55.7 | 56.5 | 33.8 | −0.5 | −1.4* | 1980–1989 | 2.4 | 1989–2018 | −1.4* | ||
| Castile & León | 29.2 | 48.3 | 31.6 | 0.2 | −3.3* | 1980–2002 | 2.7* | 2002–2018 | −3.3* | ||
| Castile-La Mancha | 23.2 | 42.0 | 38.8 | 1.3* | −1.8* | 1980–1985 | 9.4* | 1985–2004 | 1.4* | 2004–2018 | −1.8* |
| Catalonia | 46.0 | 52.0 | 37.1 | −0.7* | −4.0* | 1980–1989 | 3.8* | 1989–2007 | −0.8* | 2007–2018 | −4.0* |
| Valencia | 40.2 | 52.1 | 39.4 | −0.1 | −2.7* | 1980–1991 | 3.5* | 1991–2003 | 0.0 | 2003–2018 | −2.7* |
| Extremadura | 44.7 | 60.7 | 39.5 | −0.4 | −4.1* | 1980–1989 | 4.7* | 1989–2007 | −0.5 | 2007–2018 | −4.1* |
| Galicia | 37.6 | 56.2 | 40.1 | 0.1 | −2.8* | 1980–1994 | 2.4* | 1994–2007 | 0.2 | 2007–2018 | −2.8* |
| Madrid | 35.9 | 44.7 | 26.9 | −0.5 | −4.8* | 1980–1991 | 4.8* | 1991–2007 | −1.0* | 2007–2018 | −4.8* |
| Murcia | 38.8 | 44.0 | 38.9 | −0.3 | −2.5* | 1980–1985 | 5.7 | 1985–2003 | −0.2 | 2003–2018 | −2.5* |
| Navarre | 38.8 | 39.4 | 35.7 | −0.3 | −2.5* | 1980–2001 | 1.4* | 2001–2018 | −2.5* | ||
| Basque Country | 43.6 | 53.6 | 40.0 | −0.4 | −3.5* | 1980–1994 | 1.9* | 1994–2008 | −0.4 | 2008–2018 | −3.5* |
| La Rioja | 27.5 | 40.2 | 38.0 | −0.1 | −2.2* | 1980–2000 | 1.7* | 2000–2018 | −2.2* | ||
| Spain | 40.8 | 49.9 | 36.3 | −0.4* | −3.5* | 1980–1992 | 3.1* | 1992–2007 | −0.7* | 2007–2018 | −3.5* |
ASMR, age-standardized mortality rates using the world standard population.; AAPC: average annual percent change; APC: annual percentage change;.
In women, upward trends in ASMRs (all ages) were observed for the whole period in all the ACs, although some slope differences were detected (Table 1). The sharpest increases were observed in Cantabria (3.6%, p<0.05) and Madrid (3.5%, p<0.05). Joinpoint regression analysis did not detect changes in Madrid where a significant upward trend was observed throughout the study period. In 13 ACs, an initial period was detected in which the rates remained stable or significantly decreased, followed by a second period in which the rates increased significantly since the late 1980s or early 1990s. In three ACs, a third period (since 2004–2012) was observed in which rates remained stable (Catalonia and the Basque Country) or increase (Balearic Islands). ASMRs (30–64 years) exhibited upward trends (Table 3) in almost all the ACs (Extremadura was the only region that remained stable). Joinpoint analysis did not detect changes in 4 of the ACs (Cantabria, La Rioja, Canary Islands and Murcia, in which a significant increase (p<0.05) was observed (5.6%, 5.0%, 4.1% and 3.1% respectively) through the study period. An initial period was detected in 7 ACs in which the rates remained stable or significantly decreased, followed by a second period in which the rates increased significantly since the late 1980s or early 1990s. In 6 autonomous communities (Balearic Islands, Catalonia, Valencia, Navarre, Basque Country and Madrid) the rates stabilized since the early 2000–2010s.
In men, stable (10 ACs), downward (3 ACs) or upward (4 ACs) trends in ASMR (all ages) were observed throughout the study period (Table 2). Joinpoint analysis detect changes in all ACs: an initial period was detected in all ACs in which the rates significantly increased, followed by a second period in which the rates decreased significantly (12 ACs) or remained stable (4 ACs) since the late 1980s or early 1990s. In Castile & Leon, two initial periods of increase in rates were observed (1980–1987, 4.2%, p<0.05 and 1987–2002, 1.5%, p<0.05). A third period is observed in 7 ACs where an acceleration of the downward trend was observed from early 2000s onwards. A similar pattern was observed in the ASMR (30–64 years) although the declines during that third period were observed in 11 communities and were greater (Table 4).
DiscussionOur study reports on recent trends in lung cancer mortality in Spanish ACs shows that recently, ASMR (30–64 years) accelerated its decrease in men and slowed its increase in women (similar to what was observed in some countries),9 but with some additional key findings. According to data from the national statistics institute in Spain (2018) 22,153 people died from lung cancer (17,194 men and 4959 women), being the first cause of death from cancer in men and the second in women (after breast cancer).
These data deserve some comments. First, although men have a much higher lung cancer mortality rate than women in all Spanish ACs (in 2018, the ratio of male/female ASMRs all ages ranged from 6.6 in Extremadura to 2.4 in the Canary Islands), as reported previously,15 the sex gap is narrowing in Spain (the ratio of male/female ASMRs all ages fell from 13.3 in 1989 to 3.7 in 2018). In Europe, the ratio of male/female rates fell from 5.1 in 199423 to 2.2 in 2019.2 Second, these mortality trends are unevenly distributed among ACs, presenting considerable variability across sex. Third, the joinpoint analysis helped us identify the time points at which trends changed in the several ACs (allowing us to generate hypotheses about why these changes occurred at that particular point and help local health policy makers to identify local factors that may have influenced and act accordingly.10
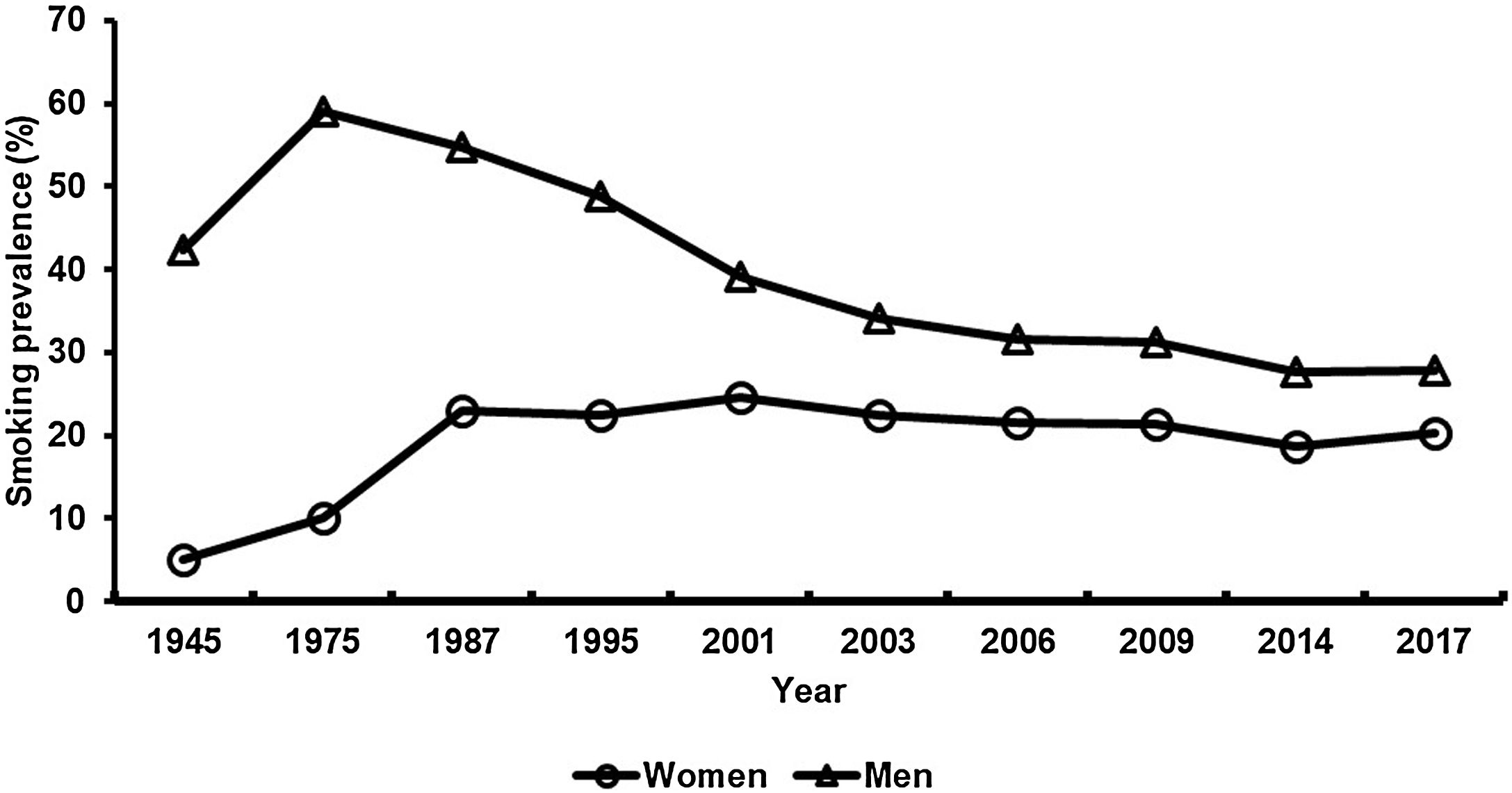
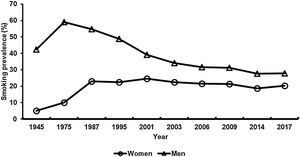
Individual cigarette smoking is by far the most common risk factor for lung cancer; other risks include passive smoke inhalation, residential radon,24 occupational exposures including do it yourself activities,25 infection and genetic susceptibility.26 Very recently, another study evaluated Smoking-Attributable Mortality in Spain in 2016, showing one in 7 deaths in Spain in 2016 were attributable to smoking.10 Although more men smoke than women (Fig. 2), the gap has narrowed27: in 1945, the prevalence of male smokers was eight times higher than that of female smokers (42% vs. 5%), but the latest Spanish National Health Survey in 2017 showed smaller differences in prevalence between the sexes (27.9% in men and 20.2% in women). The increase observed in women, since the early 1990s, in ASMR could be due to the increase in tobacco consumption since the 1970s (the prevalence increased from 5% in 1975 to 24.7 in 2001, when the figures began to fall till 2014 (18.6%). Prevalence of tobacco smoking trend seems to accurately explain the mortality due to lung cancer with a time interval of about 30 years.28
Rates of smoking prevalence for men and women in Spain, 1945–2017.
The first policies (explicitly consider tobacco as a drug and include it as a substance subject to the policies and controls of the National Drug Plan 1985) to confront the phenomenon of smoking in Spain were adopted in the mid-1980s. Policies began by regulating tobacco advertising on billboards and institutional media, a ban on television, and the appearance of the first educational programs in schools and early interventions in the primary care and public health system.29 In 2006 (Law 28/2005 on health measures against smoking) Spain implemented a partial smoking ban followed by a comprehensive ban in 2011 (Law 42/2010). After the adoption of national tobacco control laws, several tobacco control policies were developed, especially by autonomous governments, including treatment policies with a relevant impact.30 In addition, this year 2020 in Spain there has been a relevant regulatory change in the policies for financing treatments for smoking cessation. This measure is expected to further decrease the prevalence of smoking and its repercussions on health, as has already been demonstrated previously.31
Six years after the national smoke-free regulation was implemented the overall prevalence of Spanish daily smokers decreased from 33.5% in 1999 to 30.2% in 2011 (APC=−1.7% for men and −1.0% for women), also mean number of cigarettes decreased from 17.6 cig/day in 1999 to 14.2 in 2011 (this decrease being larger in men; however, an acceleration of the downward trend in women was observed from 2007 onwards).32 During the period 2009–2017, the population of ex-smokers increased (5.16%)33 and it is estimated that smoking prevalence will decrease during 2012–2025 in all age groups for both sexes except for women aged 40–64.34
The geographical variations for ASMRs differ between men and women, which is largely attributed to differences in the prevalence of smoking between autonomous communities by sex. In women, the highest prevalence in 2017 was found in Andalusia (24.6%), Valencia (22.8%) and Navarre (21.8%), and the lowest prevalence in Galicia (5.9%), Castile- Leon (7.4%) and Catalonia (7.6%). In men, the highest prevalence in 2017 was found in Valencia (32.5%), Murcia (30.4%) and Aragon (30.4%). Smoking rates have declined in Spain, but this decline varied by AC. In women, the greatest reduction in the long-term smoking prevalence (1987–2017) were Madrid (−37%), the Basque Country (−32%) and Cantabria (−27%) and in men, Canary Islands (−58%), Madrid (−55%) and Asturias (−55%).35
Our findings (ASMRs 30–64 years stabilized in Balearic Islands, Catalonia, Valencia, Navarra, the Basque Country and Madrid since the early 2000s) are plausible considering the evidence that has revealed decreasing or at least stabilizing female lung cancer rates in countries with comprehensive tobacco control programs.36
The present study has some methodological considerations. Due to the lack of availability of data on morbidity, we have used mortality data since this is the only source of data on the level of the autonomous community that is available which satisfies the criteria of continuity and globality.37 A limitation of studies based on death certificates is that they may be influenced by the quality of the death records, including problems of data validity and reliability. Nevertheless, in Spain, although certification can be improved, death certificates have been considered accurate to estimate the burden of cancer.38 Another problem related to death certificates is that during the study period, 2 different classification systems were used, ICD-9 and ICD-10, but the trend of the main causes of mortality was not greatly affected by revisions in the ICD-10.39 Furthermore, our study has analyzed truncated rates (30–64 years), in which the quality of information on cause of death is better.
In conclusion, our study shows gender differences in lung cancer mortality trends in Spain. These differences may be explained by the increased use of tobacco among women and the decreased use among men.
Authors’ contributionAll authors contributed to the conception and design of the work; the acquisition, analysis, and interpretation of data; drafting the work and revising it critically for important intellectual content; approved the version to be published; and are responsible for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are properly investigated and resolved.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNo conflicts of interest were declared from the authors.