Severe alpha-1 antitrypsin (AAT) deficiency is associated with Pi*ZZ genotypes in more than 90% of cases, and is a risk factor for developing chronic obstructive pulmonary disease (COPD), liver cirrhosis and, rarely, neutrophilic panniculitis and granulomatous polyangiitis.1
Pregnancy is associated with mechanical overload of the respiratory system due to displacement of the diaphragm and changes in the position of the respiratory muscles and the chest wall, resulting in a reduction in residual volume and functional residual capacity. It also causes an increase in oxygen consumption due to the shunt effect of the placental circulation and the development of new maternal and fetal tissues, and an increase in respiratory rate due to stimulation of the respiratory center by progesterone and estradiol, most marked from the fifth month of gestation.2,3
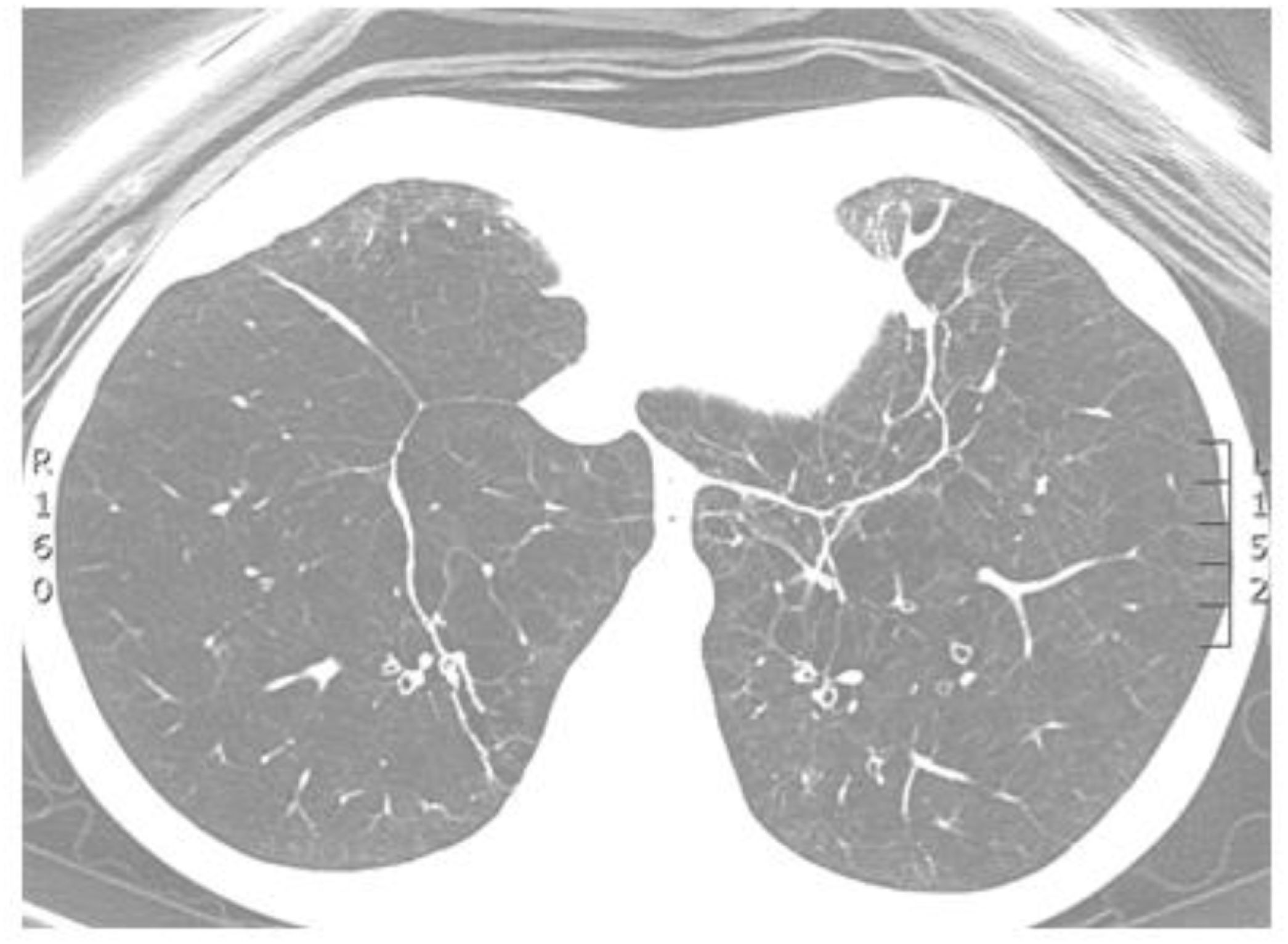
Clinical caseWe report the case of a 40-year-old woman, a former smoker with a 14 pack-year history, diagnosed at the age of 32 with COPD and AAT deficiency, Pi*ZZ genotype, with serum AAT levels of 23mg/dL (normal: 103–240). Chest computed tomography showed bilateral basal emphysema and lung function consistent with very severe obstruction, hypoxemia, and very limited exercise tolerance (Fig. 1). No hepatic involvement was detected.
In January 2013, at the age of 33, chronic oxygen therapy and intravenous infusions of commercial AAT (Prolastine®) were added to her COPD drug and rehabilitation regimen. Dyspnea developed even on minimal exertion and her respiratory function worsened progressively, so an assessment for lung transplantation was proposed.
In January 2020, she reported a 10-week pregnancy. She was informed of the lack of evidence on the management and outcome of pregnancy in her situation, but she decided to continue the gestation. At week 31, the patient was admitted to hospital for strict monitoring of fetal well-being. Her regular treatment with Prolastine® was maintained throughout the pregnancy, with good tolerance. At week 37+1, an elective cesarean section was performed with epidural anesthesia, with the birth of an infant 2400g, 46cm and APGAR test score of 10/10. She was discharged 3 days after delivery, and received a bilateral lung transplant in June 2021. She is currently stable, with no dyspnea and significantly improved lung function (Table 1).
Body mass index and lung function data.
| Variables | 2013 | 2019 | 2020Gestation week 31 | 2021Post-lung transplantation |
|---|---|---|---|---|
| BMI (kg/m2) | 15.4 | 16.9 | 18 | 17.3 |
| FVC (L/% predicted) | 1.9/50 | 2.2/59 | 1.7/47 | 3.3/89 |
| FEV1 L/% predicted) | 0.6/22 | 0.5/17 | 0.4/14 | 3.2/105 |
| FEV1/FVC (%) | 35 | 24 | 24 | 96.3 |
| TLC (L/% predicted) | 8.4/156 | 8.9/159 | 6.4/116 | |
| RV (L/% predicted) | 5.4/320 | 6.4/340 | 4.0/214 | |
| DLCO mmol/min/kPa/% predicted) | 6.8/59 | 5.4/22 | 18.4/75 | |
| KCO (% ref) | 43 | 28 | 77 | |
| pH | 7.490 | 7.430 | ||
| PO2 (mmHg) | 59 | 64 | ||
| PCO2 (mmHg) | 36 | 36 | ||
| 6MWT (m) | 550 | 457 | 603 | |
| Initial SatO2 (%) | 98 | 94 | 98 | |
| Final SatO2 (%) | 98 | 89 | 98 |
6MWT: 6-minute walk test; BMI: body mass index; DLCO and KCO: CO diffusion tests; FEV1: forced expiratory volume in 1 second; FVC: forced vital capacity; pH, PO2 and PCO2: arterial blood gases; RV: residual volume; SatO2: blood oxygen saturation; TLC: total lung capacity.
Pi*ZZ genotypes express serum AAT concentrations of 10–15%, and 80% of the scant protein levels secreted show reduced anti-elastase capacity.1 The available literature on severe AAT deficiency in pregnant women is very limited, and reported complications include preeclampsia, recurrent miscarriages, premature rupture of membranes, and reactivation of panniculitis. In this case, a term pregnancy was achieved, thus reducing neonatal morbidity and healthcare needs in childhood and adulthood. In 1977, Giesler et al.4 (Houston, Texas) published the first case of a 37-year-old woman with a Pi*ZZ genotype and severe COPD who had an uncomplicated vaginal fetal delivery. At that time, induced abortion was recommended for similar cases, but since then another 4 cases with a successful outcome have been published.5 In our opinion, therefore, the decision on termination or continuation of pregnancy should be left to the discretion of the patient and her physicians, who will weigh up the risk-benefit implications of the decision.