Takotsubo cardiomyopathy (TC) is characterized by transient and reversible systolic abnormality of the left ventricle's apex mimicking a myocardial infarction but with nonexistence of coronary artery disease.1
The etiology of TC is not well known, however the most accepted theories are catecholamine-induced cardiotoxicity and microvascular dysfunction that leads to ventricular dysfunction. Risk factors include estrogen deficiency and emotional or physical stress.1
Major complications from flexible bronchoscopy are rare (1–5%), and severe complications related to cardiovascular events are rarer still.2 We describe a case of TC induced by bronchoscopy with bronchoalveolar lavage (BAL).
A 76-year-old woman, natural from Peru, was referred to our bronchoscopy unit in order to complete the study of a recently diagnosed interstitial lung disease (ILD), with antinuclear antibodies (ANA 1:160, mottled). As a relevant personal history she had hypertension under medical treatment and obesity (IMC 31).
Patient was sedated with midazolam, fentanyl and propofol. The BAL was performed with instillation of 100cm3 of sterile normal saline into lingula and 60cm3 was collected for culture tests and cytology study. During the procedure hypoxemia was observed, high-flow oxygen therapy was required and finally the sedation was reversed with flumazenil.
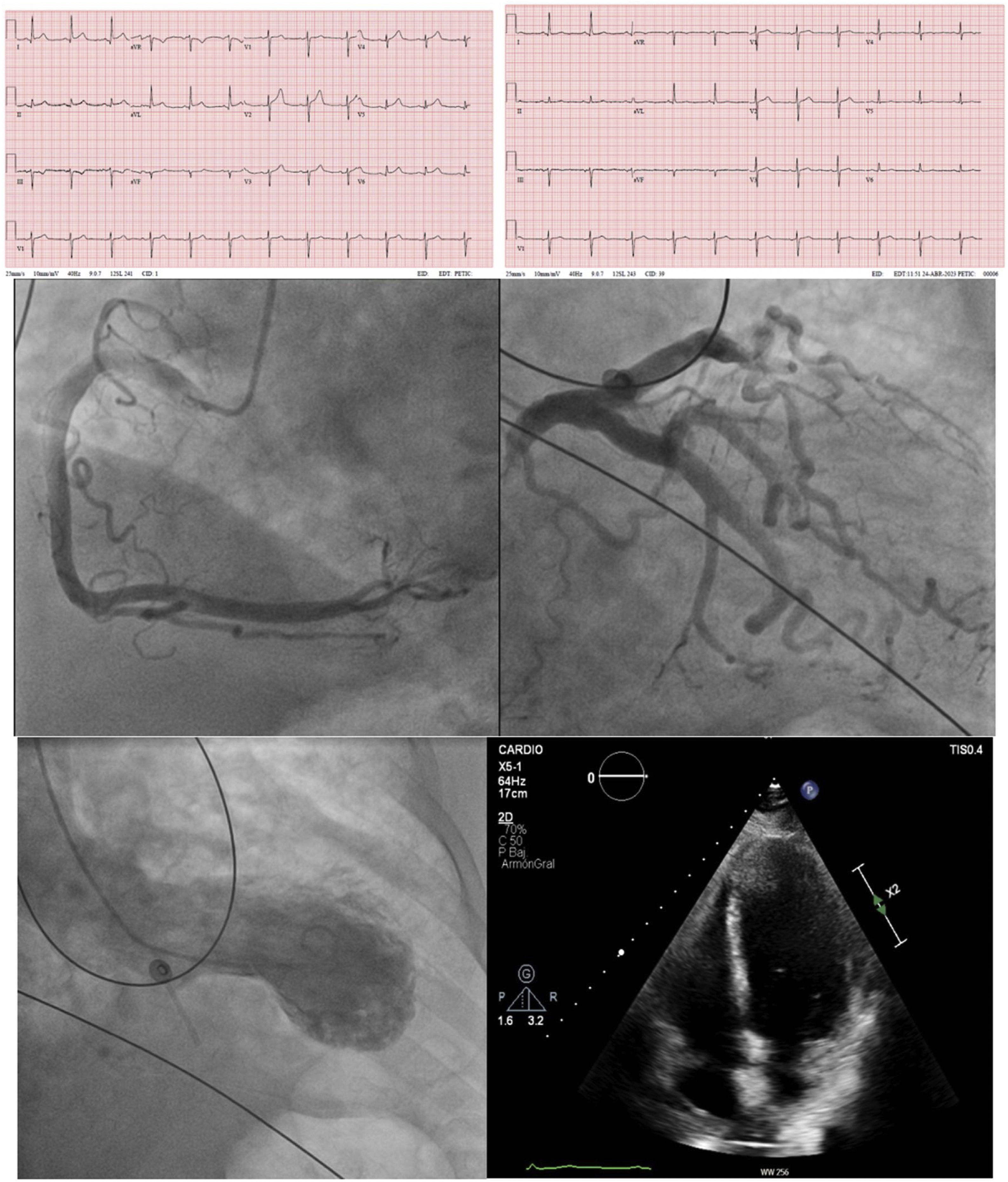
Ten minutes later she started with chest pain. In the recovery her vital signs were BP 170/100, HR 89 lpm, SaO2 91%. Electrocardiogram showed sinus rhythm with diffuse ST elevation, rectification in DIII and AVF, with a mild elevation of ultra-sensitive troponine and creatine kinase. The patient was transferred to the hemodynamics room to perform an invasive coronary angiography, showing coronary arteries without lesions. Ventriculography showed left ventricular ejection fraction 50% at the expense of akinesia of the entire apical cap, which suggested TC. At the follow-up after 2 months the ECG and the echocardiography returned to normal (Fig. 1).
(a) ECG on the left performed with chest pain shows diffuse ST-segment elevation in I, II, avL and V1–V6, rectification in III and avF. ECG on the right performed after 2 months shows normalized leads. (b) Coronary angiogram on the left reveals the arteries without coronary disease. Left: right coronary artery. Right: left coronary artery. (c) Left ventriculography in systolic frame shows apical segment akinesis with a mild depressed LVEF (46%). (d) Echocardiography performed 2 months later shows a preserved contractibility with normalization of the LVEF (60%).
Few cases have been reported in the literature of TC after flexible bronchoscopy, at least 1 case was related to BAL.3
Avoiding the bronchoscopy in myocardial infarction within firsts weeks is recommended due to the potential worsening of ischemia induced by the procedural related hypoxia.2 However, there is not much evidence about the effect of this procedure in other myocardial involvement.
In our case, the patient was an elderly woman with cardiovascular risk factors affected by ILD, who suffered a transient hypoxemia during the procedure. The use of flumazenil contributed to an increase of BP and the patient presented a stressful awakening from sedation. We hypothesized all these factors probably worked in combination contributing to the development of TC.
Although the incidence of such complications is rare and unpredictable, a novel subgroup of bronchogenic stress-induced cardiomyopathies have been proposed as one of the main triggers of TC.4 The authors emphasize the importance of minimizing risks and establishing proper management. Adequate level of sedation and use of supplementary oxygen allow to reduce the triggers of TC. Non-invasive hemodynamic and respiratory parameters monitoring during the examination and keeping patients in recovery after invasive procedures such as bronchoscopy5 contribute to a rapid detection of complications.
Conflict of InterestsThe authors state that they have no conflict of interests.