We present the case of a 48-year-old male patient who presented to our ER as a case of suicidal attempt, with a 4cm incisional neck wound. CT neck & chest on admission showed moderate pneumomediastinum. Oral contrast ruled out an esophageal tear.
48h after admission a CXR confirmed a massive pleural effusion with neck subcutaneous emphysema (Fig. 1a). A chest tube was inserted and 1500cm3/24h of clear serosanguinous fluid came out, for the next 2 days. Chylothorax was suspected but triglycerides (TG) were low (45mg/dl) as well as cholesterol level (58mg/dl). On 4th day of admission the fluid became milky and the diagnosis of chylothorax was confirmed, even though TG still remained low.
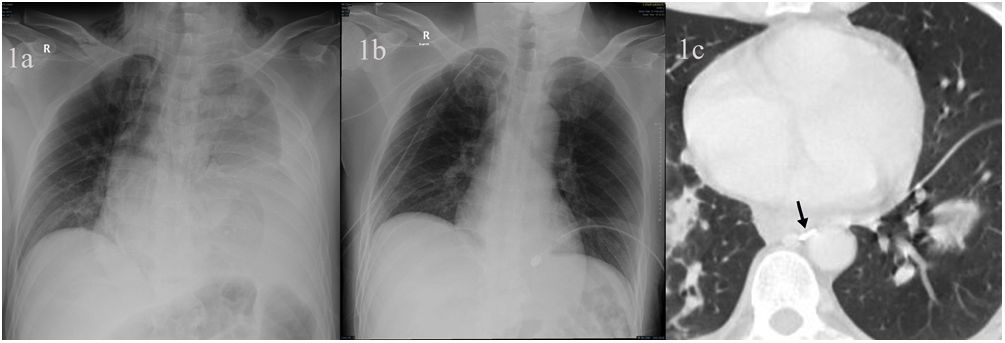
(a) Chest X-ray showing a left massive pleural effusion, pneumomediastinum and neck subcutaneous emphysema. (b) Postoperative chest X-ray, 24h after right VATS for clipping the thoracic duct. (c) Chest CT showing disseminated lung septic emboli. A metallic clip can be detected (black arrow), at T9 level, between the aorta and the azygos vein.
The patient was kept NPO, on total parenteral nutrition (TPN) and on 150μg/day of i.v. octreotide. During the first 7 days on this conservative treatment, the output ranged between 500 and 1000cm3 and for the next 5 days, between 1000 and 2000cm3. After this period, i.v. octreotide was stopped and the decision was taken to perform a right uniportal VATS thoracic duct ligation, clipping the duct at T8–T9 (Fig. 1b and c).
POD 3 the right chest tube was removed and the left one on POD 4. Patient was going to be discharged, but fever showed up. Endocarditis with septic emboli to the lung were confirmed (Fig. 1c). The patient died due to septic shock.
Chylothorax diagnosis is suggested by fluid inspection: haemoserous if the patient is fasting or milky in case the patient is eating.1 The pleural output is usually high, around 1000cm3/24h. Confirmation includes high TG levels, low cholesterol levels and presence of chylomicrons in pleural fluid. We would like to remark that low TG levels, like in our case, may be obtained in chylothorax fluid, in around 10–15% of cases.2,3
Conservative management would be the initial step recommended for treating these cases. 50% of them would be solved by leaving the patient NPO, on TPN and adding i.v octeotride.3 When the chyle output through the chest tube persists >500cm3/24h for more than 14 days or >1000cm3/24h for more than 5 days, an invasive intervention is usually needed.4
There are several options to repair the thoracic conduct: (a) interventional lymphographic embolization, with an overall success rate, in experienced centers, ranging between 45 and 70%. (b) Neck repair of the thoracic duct, using muscle flaps.5 (c) Thoracic ligation, through a minimally invasive video assisted approach, would remain one of the techniques most frequently used,1,2 due to its high rate of success (90% of cases). In our case we used a right sided single port VATS technique.
This case shows a strange complication from a neck injury: a chylothorax, containing low TG, something also uncommon. Although the chylothorax was surgically solved, the final outcome of the patient was death caused by septic endocarditis, probably related to chyle loss immunodeficiency and to central line (TPN) induced bacteriemia.
Conflict of InterestsThe authors state that they have no conflict of interests.