Underdiagnosis is one of the problems with the greatest impact on respiratory disease management and requires specific interventions. Access to quality spirometry is especially important and is an objective of the Master Plan for Respiratory Diseases of the Department of Health of the Generalitat de Catalunya.
ObjectiveTo determine the current use of spirometry at public hospitals in Catalonia, possible deficiencies and options for improvement.
MethodsA cross-sectional survey of 65 public hospitals in Catalonia in 2009. Descriptive analyses were developed for each public health-care region.
ResultsA lack of uniformity was observed in the use of spirometry at the regional level (between 0.98 and 1.50 spirometries per 100 inhabitants). We identified two factors associated with a higher rate of spirometry: (i) the existence of a Respiratory Medicine Department at the hospital, and (ii) the existence of a set location to carry out spirometries. Several areas for improvement also were identified: quality control of the test itself, the inclusion of spirometry in electronic health-care records and continuing education programmes.
ConclusionsThe results of this study have identified areas for improvement in spirometry programmes.
El infradiagnóstico es uno de los problemas de mayor impacto en las enfermedades respiratorias y requiere intervenciones específicas. Una de ellas es tener acceso a una espirometría de calidad. Este es uno de los objetivos del Plan Director de Enfermedades Respiratorias del Departament de Salut de la Generalitat de Catalunya.
ObjetivoConocer la utilización de la espirometría hospitalaria en Cataluña, y conocer los posibles déficits y las opciones de mejora.
MétodoEstudio transversal mediante una encuesta a los 65 hospitales públicos de Cataluña durante el año 2009. Se realizó un análisis descriptivo para cada región sanitaria.
ResultadosSe observó una falta de homogeneidad en la utilización de la espirometría a nivel territorial (de 0,98 a 1,50 espirometrías por 100 habitantes). Se identificaron 2 factores que están asociados a una mayor tasa de espirometrías: la existencia de un servicio de neumología en el centro y disponer de una ubicación estable para realizar espirometrías. Como áreas de mejora se identificaron el control de calidad de la prueba, la inclusión en los sistemas hospitalarios de información y los programas de formación continuada.
ConclusionesLos resultados de este estudio han permitido identificar las áreas de mejora para un programa a desarrollar.
Respiratory diseases are the third leading cause of death in developed countries,1 and the impact on the healthcare system is very high. In Catalonia (Spain), respiratory diseases lead to 10% of hospital admissions, 20% of which are related to chronic obstructive pulmonary disease (COPD).2 The incidence of COPD in subjects over the age of 40 years is around 10%.3,4 COPD exacerbation is a major health problem, due to the high risk for patients in terms of survival, and frequent exacerbations increase mortality.5 Mortality during admission is 6.7% and one-year mortality after the onset of exacerbation is 33%,6 although in Catalonia, Almagro et al.7 reported a mortality of 22% with a high percentage of re-admissions. Thirty-eight percent (38%) of patients are readmitted within the year and the mean time from discharge to readmission is 5 months.8
Underdiagnosis is one of the most serious issues in the management of respiratory diseases and COPD in particular,9 a problem that has remained constant over the years. Only one third of COPD patients are aware that they have this disease10 and 21% of patients admitted due to COPD exacerbation state that they are not regularly seen by a doctor for their respiratory problem.11 In addition to underdiagnosis, the percentage of misdiagnoses must also be considered.12,13 Pellicer Císcar et al.14 observed that even in the hospital setting, the failure to perform spirometry testing is the most important factor in explaining the misdiagnosis of COPD. Compared to patients with chronic heart failure, COPD patients have much lower chance of having confirmatory tests, even if both conditions co-exist.15,16
Reducing underdiagnosis and obtaining the correct diagnosis require specific procedures, but the most important is to guarantee access to quality spirometry.17,18
One of the major challenges facing all healthcare systems consists of identifying the most appropriate strategies for establishing priorities and implementing decisions in the front line of care.19,20 The Department of Health of the Generalitat de Catalunya uses their Master Plans21 for bringing strategic planning to the operative plans, with the aim of improving patient care. One of the objectives of the Respiratory Diseases Master Plan (PDMAR) is to guarantee that the clinician has access to quality spirometry, regardless of the healthcare setting in which he/she works. In this context, the aim of this study was to determine the use of spirometry in hospitals of the Catalonia public health system, and to highlight any possible deficits, areas for improvement and possible regional imbalances in lung function studies, particularly spirometry.
Materials and MethodsThis study was carried out within the framework of the public hospital network of Catalonia. The public health system of Catalonia is a national healthcare system which guarantees cover for the entire population, financed by public taxes. The patient does not have to make any payment at the time of receiving care. The services are financed by the Catalan Healthcare Service (CatSalut), which purchases services from different suppliers. The survey was distributed among the hospital network (XHUP) with which CatSalut has contracted service provision. These suppliers, both privately and publicly owned, make up the network of hospitals for public use and constitute the greatest part of the total healthcare network of Catalonia.
SurveyA cross-sectional study was conducted using a survey distributed to the 65 hospitals of the Catalan public network during the first quarter of 2009 (Appendix 1). The surveys were distributed via the hospital administration departments, who designated a contact person in the Respiratory Medicine departments who could provide additional responses and information if necessary. The results were collected between April and June 2009. A maximum of three attempts were made to obtain the data, with a telephone reminder after the second attempt.
DataThe survey collected information on the activity of the hospital, lung function tests that were performed in each hospital, whether basic (forced spirometry) or complex (lung volumes, carbon monoxide diffusing capacity, arterial blood gases), number of spirometries carried out in the previous year, information on the spirometers, person requesting the spirometries and the location where these are carried out, quality control procedures performed, inclusion in hospital databases, information on the professionals carrying out and interpreting the tests, training received, etc. (Appendix 1).
With regard to the location where the spirometry is carried out, for the purposes of this study, the “lung function laboratory” was defined as a set space identified as such in which at least one nursing professional regularly carried out spirometries, carbon monoxide diffusing capacity (DLCO) determinations and/or lung volumes.
IndicatorsThe indicators calculated were as follows: number of spirometries per 100 hospital beds, per 100 discharges, per 100 outpatient consultations, per 100 emergency consultations and per 100 inhabitants. All were calculated for one year. Results were obtained overall and by healthcare region.
Statistical AnalysisA descriptive analysis was initially performed of the survey items for the whole of Catalonia, for each of the healthcare regions and for the healthcare sectors within the Barcelona healthcare region. The number of cases and frequencies of the categorical variables and central tendency statistics and dispersion of continuous variables were calculated. The variation ratio (VR) was used to describe the magnitude of the difference between regions. This is the ratio between the highest and lowest values of the rates for the complete set of regions studied. It is an indication of how much the region with the highest rate varies with respect to the region with the lowest rate.
The number of spirometries carried out in each hospital is distributed using a Poisson law. To explore the association between the number of spirometries carried out in each hospital and the various factors of the survey, a multilevel Poisson regression model was constructed, including the number of discharges from the hospital as the offset. The factors studied were the existence of a Respiratory Medicine department in the hospital, whether the patients admitted were seen by a pulmonologist, the number of lung function tests performed, the availability of a set location for performing spirometries, if there was quality control of the tests, the availability of a data system, formal training for professionals and if they had undergone that training in the last year. An association with a P-value of less than .05 was considered significant. The SPSS v18 programme was used for data management and the STATA v11 for the statistical analysis.
ResultsResponsesAll 65 hospitals in the Catalan public healthcare network completed the survey and it was determined that 8 of them, due to their specific specialist nature, did not carry out spirometries. The results presented below are derived from the 57 hospitals in which spirometries were carried out. The survey was piloted in three hospitals in Barcelona and Vic (in which the authors of the design are currently employed) to assess the feasibility of the items to be completed. Survey completion was the responsibility of the physicians in charge of each of the lung function laboratories, who in turn designated the professional who would complete the survey. We do not have data on their professional category and/or responsibilities.
Presence of a PulmonologistIn 34.5% (n=19) of the hospitals there was a Respiratory Medicine department, in 34.5% (n=19) there was a Respiratory Medicine section, 25.5% (n=14) had a consultant pulmonologist and 5.5% (n=3) did not have any of these three resources. Respiratory patients who were admitted were treated in 24.1% (n=13) of the cases primarily by pulmonologists, in 35.2% of cases (n=19) by internists and in the remaining 40.7% (n=22), care was shared between pulmonologists and internists.
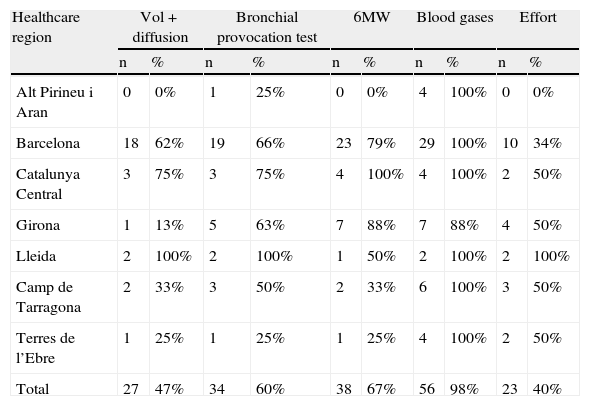
Types of TestsTable 1 shows the type of lung function tests that were carried out in the 57 hospitals in the study. Spirometry was carried out in all centres. In 85.9% (n=49) of the centres, at least three of these tests were carried out. Testing was performed in paediatric patients in all healthcare regions, but only in 67% of the hospitals (n=39). Spirometry was carried out in various locations in or outside the hospital that were not mutually exclusive: 47% (n=27) of the hospitals had a set location; of these, 37% (n=21) had a lung function laboratory as previously defined. Spirometry was also performed in other hospital settings: in 37% (n=21), they were performed in outpatient clinics, in 26% (n=15) in the day hospital, in 10% (n=17) in the conventional ward, in 7% (n=4) in the patient's home, in 14% (n=8) in the Respiratory Medicine ward and in 10% (n=17) in the general medicine ward.
Number and Percentage of Hospitals With Lung Function Testing in Each Healthcare Region. Catalonia, 2009.
| Healthcare region | Vol+diffusion | Bronchial provocation test | 6MW | Blood gases | Effort | |||||
| n | % | n | % | n | % | n | % | n | % | |
| Alt Pirineu i Aran | 0 | 0% | 1 | 25% | 0 | 0% | 4 | 100% | 0 | 0% |
| Barcelona | 18 | 62% | 19 | 66% | 23 | 79% | 29 | 100% | 10 | 34% |
| Catalunya Central | 3 | 75% | 3 | 75% | 4 | 100% | 4 | 100% | 2 | 50% |
| Girona | 1 | 13% | 5 | 63% | 7 | 88% | 7 | 88% | 4 | 50% |
| Lleida | 2 | 100% | 2 | 100% | 1 | 50% | 2 | 100% | 2 | 100% |
| Camp de Tarragona | 2 | 33% | 3 | 50% | 2 | 33% | 6 | 100% | 3 | 50% |
| Terres de l’Ebre | 1 | 25% | 1 | 25% | 1 | 25% | 4 | 100% | 2 | 50% |
| Total | 27 | 47% | 34 | 60% | 38 | 67% | 56 | 98% | 23 | 40% |
6MW: 6-minute walking test; Vol+Diffusion: volume+diffusion.
In all hospitals, the spirometer was calibrated, mainly by nursing or technical staff: 81% (n=43) nursing staff, 30% (n=16) technical staff and 17% (n=9) physicians, although in some cases the calibration was performed equally by different professionals. The interpretation of the tests depended on the organization of each centre. In 11% (n=6) of the cases, each doctor interpreted the tests that he/she had requested him/herself. In 87% (46%) of the hospitals, the tests were interpreted by pulmonologists and in 19% (n=10) by the internists as well. In 9% (n=5) of the centres, the results were interpreted by family doctors and in one hospital by the nursing staff.
Seventy-one percent (71%) (n=40) of the hospitals stated that they carried out quality control of the tests. Since the question allowed for an open answer, the centres responded in a varied manner. The most frequent responses were the use of healthy volunteers or professionals, direct supervision of the test or data obtained from the spirometry equipment itself and/or the visual analysis of the flow-volume curves.
In 35% (n=2 0), the information provided by the spirometry was available in the hospital data system: it was entered manually in 9 centres and automatically in 11. In 24.5% (n=13) of the hospitals, the precise contents of the spirometry report were transferred to the hospital database or clinical records. In 20.8% (n=11) of the cases, the spirometry data were not entered in an unbundled format (pdf format), so the data could not be individually manipulated, in only 7.5% (n=4) of the hospitals, the data were entered in an unbundled format, and the spirometry report in its entirety was incorporated in an unbundled format in 3.8% (n=2) of the hospitals.
Training of ProfessionalsIt was observed that only one hospital selected professionals with previous training, while in the majority of the centres (86.8%, n=46), professionals were selected and then received training. In 43.9% (n=25) of the hospitals, the professionals performing the spirometries received internal non-formal training and in 26.3% (n=15), they received internal formal training. When asked about what type of continuing education was given, 25% (n=14) only carried out training at the time the professionals were selected and 14% (n=8) carried out regular yearly training, while 59.6% (n=34) carried out training spontaneously. When asked how long it was since the professional involved in performing the spirometries had done a course, 14.8% (n=8) of the hospitals answered less than 3 months, 5.6% (n=3) between 3 and 6 months, 20.4% (n=11) less than one year, 24.1% (n=13) between 1 and 2 years and 35.2% (n=19), more than 2 years.
Request for ExaminationsThe survey showed that of the professionals requesting spirometry, 57% (n=30) were the hospital pulmonologists, 18% (n=9) hospital internal medicine specialists, 11% (n=6) were other hospital physicians, 3% (n=2) pulmonologists from outside the hospital, 4% (n=2) were primary care physicians and 2% (n=1) doctors from other hospitals.
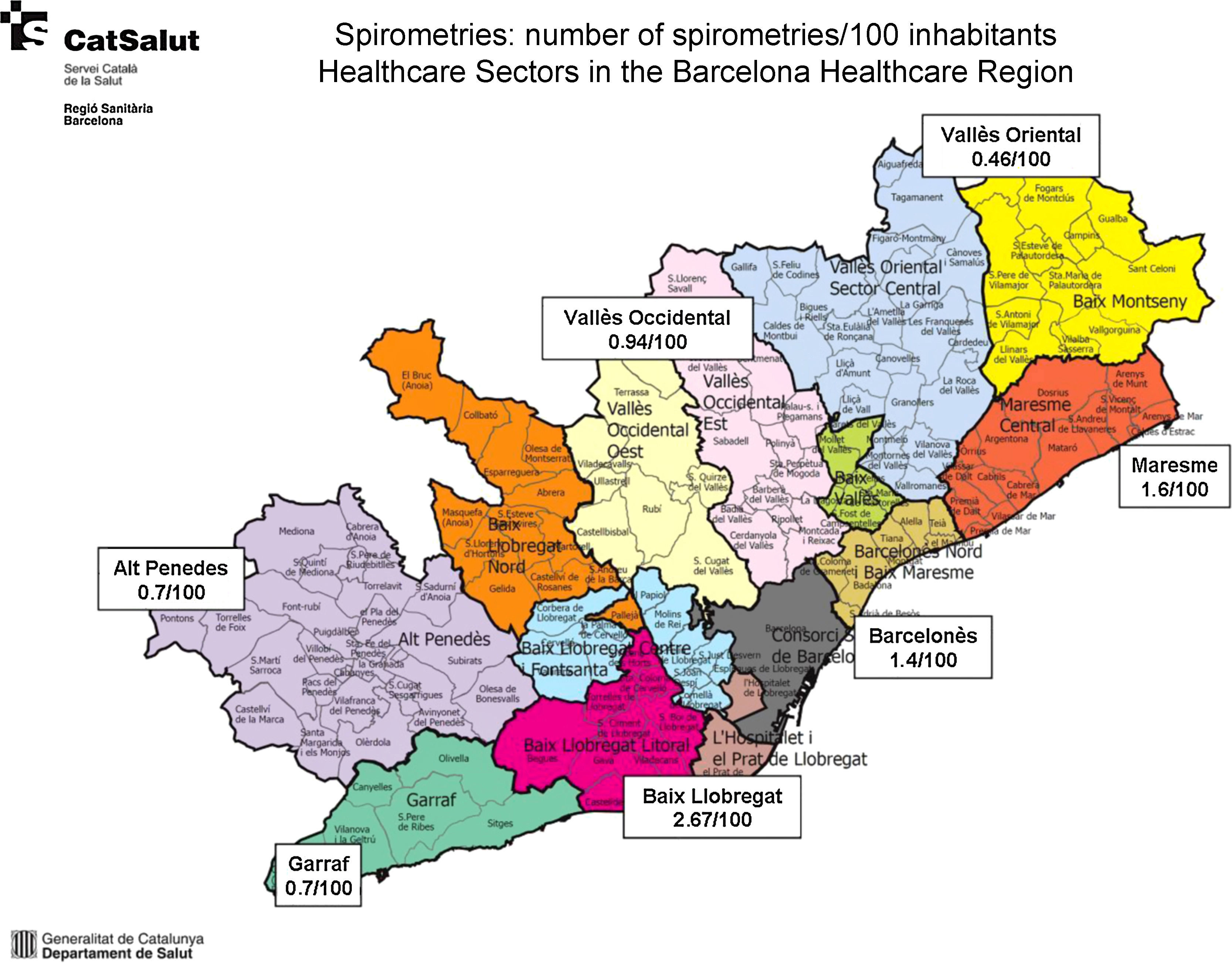
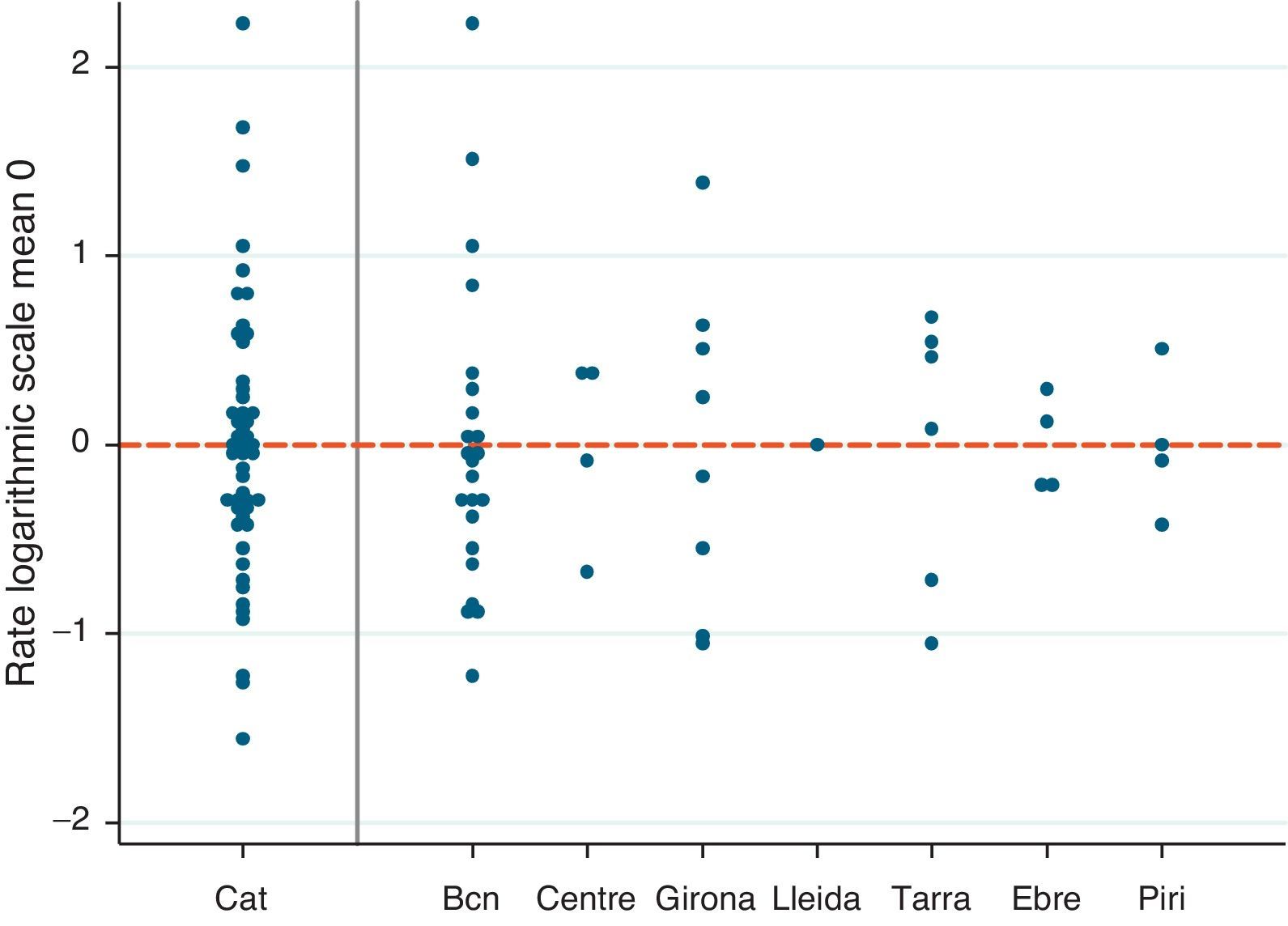
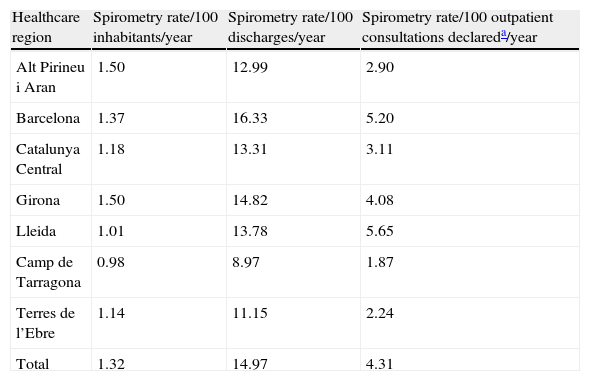
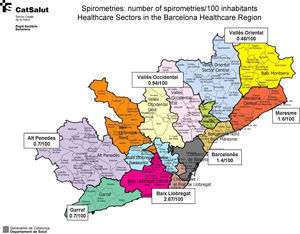
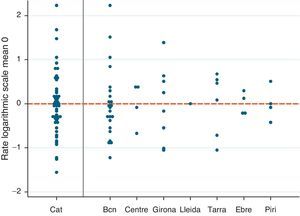
Distribution of the Number of ExaminationsThe rate of spirometries per 100 hospital discharges/year was 14.97, with a VR of 1.82, indicating an 82% greater use of spirometry between the region with the highest rate compared to the region with the lowest rate. The rate of spirometries per 100 inhabitants/year was 1.32, with a VR of 1.53; Fig. 1 shows the wide variability in the Barcelona healthcare region. This region was analyzed by healthcare sector, since it accounts for 67.8% of the whole population of Catalonia (Figs. 1 and 2 and Table 2).
Spirometry rates per centre (Catalonia, 2009). The spirometry rate per centre for the whole of Catalonia and by healthcare region are presented on a logarithmic scale and centred on the mean to improve comparability. Each point represents a hospital centre. Bcn: Barcelona healthcare region; Cat: total Catalonia; Centre: Central healthcare region; Ebre: Terres de l’Ebre healthcare region; Girona: Girona healthcare region; Lleida: Lleida healthcare region; Piri: Alt Pirineu healthcare region; Tarra: Tarragona healthcare region.
Spirometry Rate by Catalan Healthcare Regions. Catalonia, 2009.
| Healthcare region | Spirometry rate/100 inhabitants/year | Spirometry rate/100 discharges/year | Spirometry rate/100 outpatient consultations declareda/year |
| Alt Pirineu i Aran | 1.50 | 12.99 | 2.90 |
| Barcelona | 1.37 | 16.33 | 5.20 |
| Catalunya Central | 1.18 | 13.31 | 3.11 |
| Girona | 1.50 | 14.82 | 4.08 |
| Lleida | 1.01 | 13.78 | 5.65 |
| Camp de Tarragona | 0.98 | 8.97 | 1.87 |
| Terres de l’Ebre | 1.14 | 11.15 | 2.24 |
| Total | 1.32 | 14.97 | 4.31 |
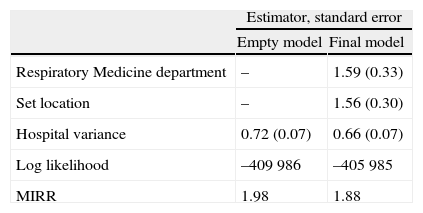
Table 3 shows the analysis of the association between the numbers of spirometries carried out in each centre and the different factors surveyed, using a multilevel Poisson regression model. Among the various factors investigated, a statistically significant association was observed between the existence of a Respiratory Medicine department at the site and the availability of a set location for performing spirometries. The presence of these factors in a centre increased the spirometry rate by 59% and 56%, respectively. This could explain part (8%) of the difference between the centres, although it remains considerable. In this respect, the median incidence rate ratio (MIRR) is interpreted in such a way that the mean increase in the rate of spirometries between any two centres is 98% in the empty model and 88% in the final model. This suggests wide variability between the rates per centre, as shown in Fig. 1 and Table 2. In this figure, the points represent the spirometry rates in each centre logarithmized and centred at zero for better comparability.
Multilevel Poisson Model Between Number of Spirometries and Various Factors Surveyed.
| Estimator, standard error | ||
| Empty model | Final model | |
| Respiratory Medicine department | – | 1.59 (0.33) |
| Set location | – | 1.56 (0.30) |
| Hospital variance | 0.72 (0.07) | 0.66 (0.07) |
| Log likelihood | –409 986 | –405 985 |
| MIRR | 1.98 | 1.88 |
The Poisson regression model is used in studies with count variables in a unit of space or time, in this case the number of spirometries carried out in one year. The coefficients of the model are interpreted in terms of incidence rate ratio. Taking as an example the variable “Respiratory Medicine department”, the presence of this in a centre increases the spirometry incidence rate by 59%.
The empty model is presented first to show the reduction, both in terms of plausibility (log-likelihood) and the variance between centres, represented by the inclusion of the variables “Respiratory Medicine department” and “set location”.
The median incidence rate ratio (MIRR) represents the median distribution of the difference in spirometry rates between any 2 centres.
There was little homogeneity in the results of the hospital spirometry survey between the hospitals and healthcare regions of Catalonia with respect to the use of spirometry, which may be a contributory factor to the underdiagnosis9,22 of respiratory diseases.23
In some studies, this heterogeneity has been attributed to factors such as accessibility to the test15 or the physician not requesting the test. In our study, variability cannot be attributed to accessibility, since all the healthcare regions have the necessary infrastructure for performing spirometry. The variability may be explained by the existence or non-existence of a Respiratory Medicine department and by the availability of a set location for performing spirometries. These factors are associated with a greater number of spirometries. Having a Respiratory Medicine department implies the explicit recognition of the distribution of tasks within the centre. Accordingly, in view of the survey data, we suggest that the most important aspect is not the structure in itself (i.e. the existence of the department) but rather the explicit recognition of the importance of lung function testing. Some studies attribute the under-use of spirometry, compared to other tests such as echocardiograms, to the characteristics of the disease itself.15,16,24 We have not identified an indicator that would allow us to determine the appropriate range for spirometries per discharge volume or per hospital bed or per 100 inhabitants, but we do consider that obtaining those results when beginning to design a master plan could provide us with our own indicator for evaluating results in the future, while not forgetting that this will always be a process indicator, rather than a results indicator.
It is likely that the differences in use of spirometry in the hospitals can be explained by various factors, from those centred on the professionals themselves to organizational factors. Adherence to clinical practice guidelines by professionals25 or the basic training of personnel caring for respiratory patients in the hospitals may alter the use of spirometry. Thus, as we show in our study, in hospitals which had a Respiratory Medicine department and a set location for carrying out spirometries, a greater number of spirometries were performed. This result confirms that significant work needs to be carried out by pulmonologists in all healthcare settings and systems to encourage the use of spirometry by other specialists and primary care physicians.
Spirometry is a test which depends highly on the professional performing it. The importance of the training of that professional at the time of carrying out the spirometry has been documented26–28 and this implies an organizational need for professionals who have already received training before accessing the lung function laboratory. The need for homogeneous, standardized, continuing education programmes accepted by all organizations in order to achieve high quality spirometry has also been demonstrated. Our survey highlights the lack of rigour in the area of continuing spirometry education, since at the time of selecting the professionals for carrying out spirometries, the majority of hospitals do not take into account prior training, and the training that is given is neither formal nor systematic.
When the quality control of the spirometers is analyzed, the diversity of responses to an open question on how quality control is performed is remarkable. Telemedicine strategies could probably help improve this quality control and achieve an increase in quality spirometries.29 Another area needing improvement has also been detected, namely, access to spirometry data via the hospital data systems. To our understanding, it is crucial that spirometry is not left behind in the ongoing development of computerized clinical records.
The evaluation of the other lung function tests demonstrates that all healthcare regions have access to complex lung function testing, except for Vall d’Aran, a healthcare region in the high mountains, which nevertheless, has well-established connections to the nearest healthcare area. It is also of note that the 6-minute walking test is not widely disseminated among all the hospitals, as might be expected from its ease of use30 and its importance in the integral evaluation of COPD patients.31
Study LimitationsThe methodology used in this study was a survey. Although there are no methodological alternatives for conducting the study, the limitations of this information source must be taken into account. In this study, the primary care network was not assessed, but we have recently started a survey of all the public network health centres in Catalonia. Since no other regional, national or international studies have been published, we cannot compare our data with the existing literature. There is no indicator in the literature regarding the number of spirometries per inhabitant; accordingly, one of the objectives initially proposed with respect to the assessment of the variability of the results and a comparison with the literature could not be estimated. For this reason, the statistical and clinical relevance of spirometry rates per inhabitant and year was not evaluated.
Other limitations of the study could include the bias in information derived from the person completing the survey and the fact that the estimated rates could not be standardized for age and sex of the patients. Part of the variability observed could be explained by the different population structure of each healthcare area, as well as severity levels or different comorbidities.
ConclusionsThe analysis of the use of spirometry in the hospital setting has allowed us to: (a) define the existence of a Respiratory Medicine department and a set location for performing spirometries as factors related with the more frequent performance of these tests; (b) draw up a homogeneous, decentralized and “self-replicating” training programme for all healthcare regions in Catalonia, which would allow quality spirometry to be performed within constantly changing organisations32; (c) determine the need for the inclusion of spirometry in hospital databases (electronic clinical records), thus standardizing data transfer and promoting interoperability; and (d) set up spirometry quality control models using information and communication technology.29 It has also allowed us to determine an indicator for the use of forced spirometry in a population (0.98–1.53 spirometries per 100 inhabitants), which to our knowledge does not appear in the reviewed literature.33 These changes should impact both on the professionals themselves and on the organizational structures of the hospitals, and in all cases should guarantee access to quality spirometry for all clinicians, regardless of the healthcare level at which they work.
Conflict of InterestsThere are no conflicts of interest or sources of funding.
The authors would like to thank all the participating centres for the collaboration in data collection and Jordina Capella and Cristian Tebé Cordomí (Agency for Health Information, Evaluation and Quality of the Department of Health of the Generalitat de Catalunya) for their invaluable help with the statistical analysis of the data in this paper.
B. Avilés (Hospital de Palamós); F. Burgos (Hospital Clínic, Barcelona); J. Clotet (EAP Ponts, Lleida); J. Delclós (University of Texas School of Public Health, United States); J. Escarrabill (PDMAR, Agency for Health Information, Evaluation and Quality [AIAQS]); J. Giner (Hospital de la Santa Creu i Sant Pau, Barcelona); M.A. Llauger (EAP Encants, CAP Maragall, Barcelona); R. Hervàs (CAE Dr. Barraquer, Sant Adrià del Besòs, Barcelona); F. Martín (EAP Tarragona, CAP Jaume I, Tarragona); C. Martín, A. Moreno (Hospital Vall d’Hebron, Barcelona); F. Moya (TIC Salut); N. Roger (Consorci Hospitalari de Vic); C. Rubies, T. Salas (Departament de Salut, Área TICs); E. Torrente (Agency for Health Information, Evaluation and Quality [AIAQS]).
PDMAR Steering Committee: J. Escarrabill (Agency for Health Information, Evaluation and Quality [AIAQS]); C. Hernández (Hospital Clínic, Barcelona); J. Jiménez (CatSalut, Barcelona); M.A. Llauger (EAP Encants, CAP Maragall, Barcelona); N. Roger (Consorci Hospitalari de Vic); A. Rosas (General Regulatory, Planning and Evaluation Directorate; Department of Health, Barcelona); E. Saltó (General Public Health Directorate, Barcelona); R. Tresserras (General Regulatory, Planning and Health Resources Directorate; Department of Health, Barcelona), E. Torrente (Agency for Health Information, Evaluation and Quality [AIAQS]).
Please cite this article as: Roger N, et al. Encuesta de utilización de la función pulmonar en los hospitales públicos de Cataluña en 2009. Arch Bronconeumol. 2013;49:371–7.
See Appendix 1.