We read with great interest the recent letter to the editor by Cadiñanos Loidi et al.1 which described a 45-year-old woman who presented with endobronchial tuberculosis and cutaneous and lymph node involvement. Although tuberculosis is prevalent worldwide, certain unusual presentations can make the etiological diagnosis challenging. We would like to highlight the imaging findings of an uncommon presentation of thoracic tuberculosis in a case we recently encountered.
A 67-year-old man presented with a subcutaneous nodule in the sternal region with no inflammatory signs and progressive growth noted 2 months previously. One month later, the lesion exuded an odorless white secretion, and similar lesions in the axillary and clavicular regions also showed signs of fistulization. The patient reported daily intermittent fever during the evening, asthenia and weight loss. Physical examination showed bilateral cervical, supraclavicular and axillary lymphadenopathy with fistulization. Laboratory test results were normal and an HIV test was negative. A tuberculin skin test was positive, with 8mm induration.
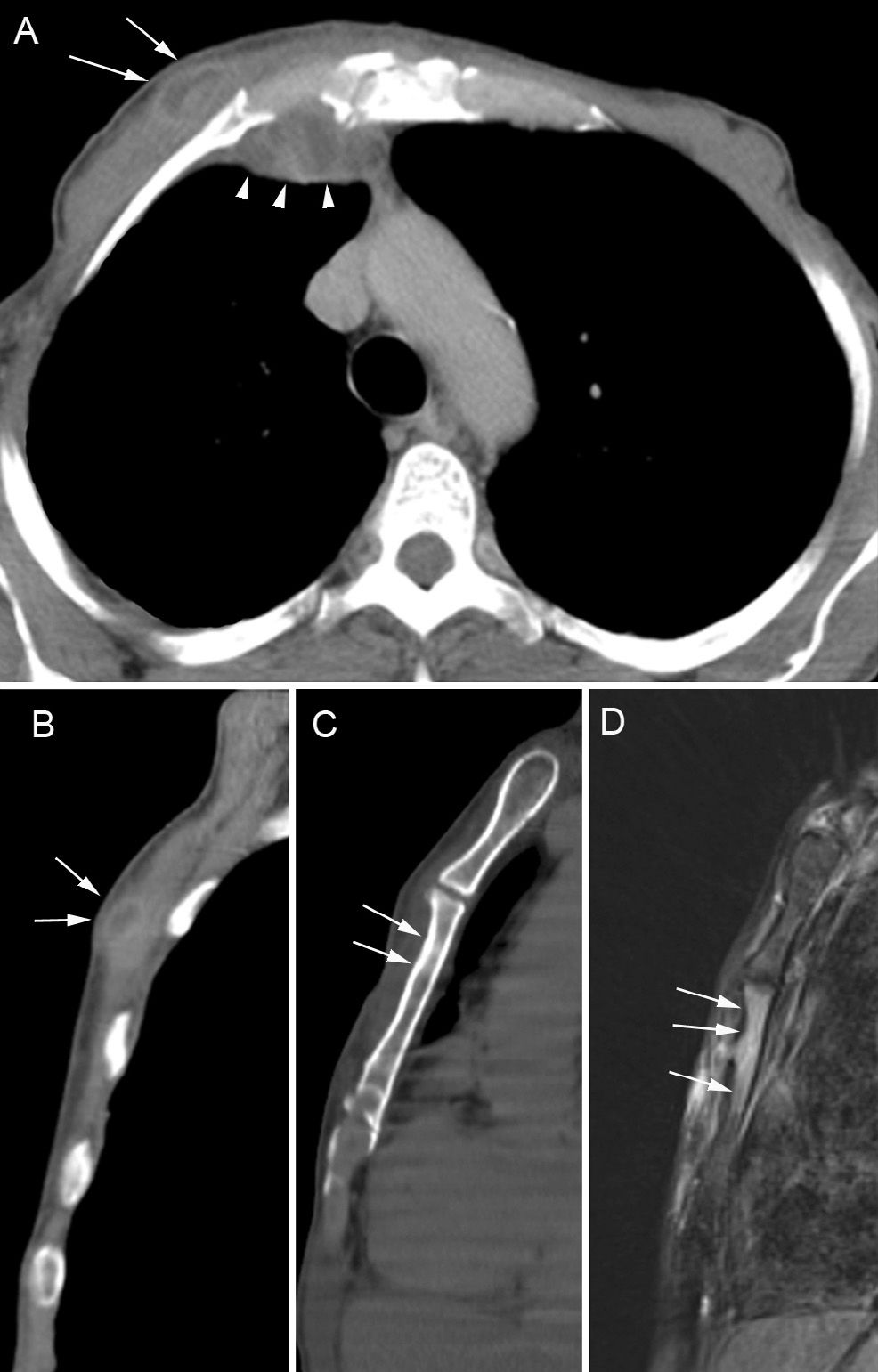
Chest CT showed fluid collection in the soft tissues of the right anterior chest wall, adjacent to the ipsilateral chondrosternal joint, with cortical thickening of the sternal body (Fig. 1A–C). The lungs were normal. Sagittal T2-weighted MRI with fat saturation showed bone marrow edema in the sternum (Fig. 1D). A biopsy of the sternal lesion showed chronic, granulomatous, suppurative inflammation with caseous necrosis. Sternal fluid secretion and biopsy material were positive for Mycobacterium tuberculosis. The bacteria were sensitive to anti-tuberculosis drugs. The patient was given four-drug (isoniazid, pyrazinamide, ethambutol and rifampin) anti-tuberculosis treatment for 2 months (intensive care phase) and isoniazid and rifampin for 4 months (maintenance phase), and achieved complete clinical recovery. One year later the patient was asymptomatic.
Axial (A) and sagittal (B) reformatted chest CT images show hypodense collection in the soft tissues of the right anterior chest wall, adjacent to the sternum (arrows). The collection communicates with another internal parietal collection (arrowheads). Another sagittal image (C) shows thickening of the cortical bone on the anterior surface of the sternal body (arrows). A sagittal T2-weighted MR image with fat saturation (D) shows high signal intensity of the sternal bone marrow.
Mycobacterial infections of the sternum are very rare and usually develop secondary to sternotomy, Bacillus Calmette–Guérin vaccination, or immunosuppression.2,3 Complications of tuberculous sternal osteomyelitis include secondary infection, fistula formation, spontaneous sternal fracture, tracheal compression, and rupture of tuberculous abscess into the mediastinum, pleural cavity, or subcutaneous tissues.2
On standard X-rays and CT images, sternal changes may be minimal and unassociated with significant bone destruction. In this situation, it may be difficult to differentiate between osteomyelitis and inflammatory soft tissue lesions. Cortical thickening may merely be a periosteal reaction secondary to the inflammation of surrounding soft tissue. In these cases, MRI may provide valuable diagnostic information by showing inflammatory changes in sternal bone marrow characterized by low and variable signal intensity on T1- and T2-weighted images, respectively.1,3 Indeed, some associated features suggestive of tuberculosis, including fistulae, heterogeneous soft-tissue masses and sternoclavicular joint abnormalities, are valuable for diagnosis.4 However, no radiographic (CT or MRI) finding is pathognomonic for sternal tuberculosis. Thus, definitive distinction between tuberculous sternal osteomyelitis and other causes of sternal infection rests largely on histopathological and/or microbiological examination.3,5
The majority of authors have argued that standard anti-tuberculous chemotherapy is sufficient to treat sternal tuberculosis, although some believe that surgical debridement should be utilized. No consensus guideline regarding treatment regimen and duration has been developed. Aspiration and anti-tuberculous chemotherapy are the treatments of choice. Close follow-up is essential to detect complications that may necessitate surgery. Surgical treatment is advised when removal of a large sequestrum is necessary, when the diagnosis is doubtful, and in non-responding cases.2 In conclusion, MRI may be useful for the diagnosis of sternal tuberculosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Canella C, Zanetti G, Marchiori E. Tuberculosis esternal: papel de la imagen médica. Arch Bronconeumol. 2015;51:100–101.