The rapid introduction of new information and communication technologies into medical practice has prompted the Spanish Society of Pulmonology and Thoracic Surgery to publish a position paper on sleep-disordered breathing, especially in relation to positive pressure treatment. It should be pointed out that the scientific literature is to some extent controversial due to a paucity of large randomized multicenter studies with long-term follow-up. Moreover, the telematics devices and systems on the market vary widely. As a result, the recommendations are based primarily on a consensus of expert professionals. Another very important aspect addressed extensively in this document is the obvious lack of regulations on telemedicine and the operations of commercial companies. The most important recommendations included in this position paper are that telemedicine is primarily advocated in subjects with travel problems or who live far from the hospital, in patients with poor CPAP compliance, and in most cases treated with non-invasive mechanical ventilation. A key element is patient individualization. It is imperative that the relevant technical, legal and ethical requirements (medical device regulations, data protection, and informed consent) are met. Finally, expert professionals from our society must contribute to and become involved in spearheading this technological change.
Como consecuencia de la rápida introducción de las nuevas tecnologías de información y comunicación (TIC) en la práctica médica, la Sociedad Española de Neumología y Cirugía Torácica ha promovido la elaboración de un documento de posicionamiento aplicado a los trastornos respiratorios del sueño, especialmente en relación con el tratamiento con presión positiva. Cabe mencionar que la literatura científica es en parte controvertida debido a que no existen suficientes estudios multicéntricos aleatorizados, con elevado número de pacientes y seguimiento a largo plazo. Además, los equipos y sistemas telemáticos en el mercado son diferentes. Como consecuencia, las recomendaciones se basan sobre todo en un consenso de profesionales expertos. Otros aspectos muy importantes son la clara ausencia de normativa o las funciones propias de las casas comerciales, que en este trabajo se abordan ampliamente. Las recomendaciones más importantes incluidas en el documento de posicionamiento son que la telemedicina se destina, básicamente, a sujetos con problemas de desplazamiento o con domicilio lejano, a aquellos que no cumplen de forma adecuada el tratamiento con CPAP y a la mayoría de los casos con ventilación mecánica no invasiva. Un elemento clave es la individualización de los pacientes. Es imperativo que se cumplan los requisitos técnicos, legales y deontológicos pertinentes (normativa de los productos sanitarios, protección de datos y consentimiento informado). Por último, los profesionales expertos de nuestra sociedad han de contribuir e implicarse en el liderazgo de este cambio tecnológico.
As a consequence of the rapid incorporation of information and communication technologies (ICT) in this respiratory medicine specialty, the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) has sponsored the development of this position paper on telemedicine (TM) in sleep-disordered breathing (SDB), addressing in particular the use of continuous positive airway pressure (CPAP) and non-invasive mechanical ventilation (NIV). The purpose of this document is to establish criteria for good quality clinical practice in TM. This article is divided into sections which include theoretical and practical aspects and which, importantly, take into account the opinion of health technology suppliers (represented by the FENIN Federation) and various legal aspects (ICAM - Law Society of Madrid).
To give greater visibility and to facilitate the dissemination of this position paper, the recommendations of the working group will first be described and the grounds for these recommendations will then be discussed in detail.
Recommendations- 1
TM refers to the remote practice of medicine using ICTs with the aim of improving healthcare, collaboration between health professionals, and patient care pathways.
- 2
TM has a wide range of uses, including diagnosis, follow-up, work and management. The level of evidence is sometimes limited. Factors that are key to success include treating subjects on an individualized basis and determining diseases and disease stages. Not all clinical processes require TM. It must be used in certain well-established situations and introduced progressively, building on solid groundwork. Scaling up to health system-wide application is not yet possible. At present the use of TM should be encouraged, as it is here to stay.
- 3
There are 2 forms of TM: synchronous and asynchronous. The first involves real-time contact (video conferencing) and the second involves deferred contact (data broadcast via devices); asynchronous contact is much easier to implement and should be used initially.
- 4
Physicians should use their professional judgment on the proper use of TM in a specific patient and should not compromise their ethical obligation to provide clinically appropriate care in favor of adopting new technologies. Care must be taken to ensure that the TM meets the same standards of clinical practice as face-to-face medicine. It is essential to understand that TM must never replace a medical visit if it is clearly necessary.
- 5
TM requires that the relevant technical, ethical and legal requirements are met: 1) equipment must comply with medical product standards; 2) data obtained must be processed in accordance with data protection regulations; and 3) patients must be properly informed and agree to the use of such techniques by giving informed consent.
- 6
Proper training in TM equipment and techniques is essential. This is a key consideration for the various healthcare professionals involved, and for patients and suppliers. Failure to properly prepare and coordinate remote care undermines clinical practice.
- 7
Medical professionals must show that they are appropriately informed and trained by obtaining certification from the Spanish Federation of Sleep Medicine (FESMES), and they must help spearhead this technological change, which will result in valuable developments in clinical practice in coming years. Support from non-health professionals, such as biomedical engineers and suppliers, is essential.
- 8
Collaboration between the different actors involved in monitoring and follow-up is essential. In this regard, equipment manufacturers, service providers and, of course, health professionals must work closely together by establishing joint care protocols. It is essential to take into account concepts of rights and duties.
- 9
With regard to SDB, although there are some differences in the use of TM, this committee recommends this approach in two specific situations: in subjects who do not adequately comply with CPAP therapy, and in patients with NIV, especially at baseline or when, in the opinion of the doctor, monitoring is required.
- 10
Currently TM, while very useful, is not always appropriate for all subjects at the start of CPAP therapy. Moreover, no factors have been identified to predict which subjects will be poor compliers. However, given the good compliance that can be achieved nowadays, TM could be incorporated after the first month of poor compliance. Finally, it should be noted that TM can be cost effective because it reduces loss of working hours and avoids travel, of particular interest in the case of patients with difficulties accessing transport.
In summary, the working group believes that TM is beneficial and assists significantly in the delivery of health services, especially if subjects, their diseases, and their status are adequately identified. It is essential to establish technological quality regulations and precise legal and clinical indications. The COVID-19 pandemic has shown that the use of TM will increase exponentially, for both medical visits and patient monitoring, similar to the situation in other professional activities and procedures, and even teaching. Telemedicine is here to stay.
IntroductionThe World Health Organization defines TM as the delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries. TM can make a significant contribution to continuing professional development, to different research and evaluation activities, to improving the welfare of individuals and communities, and to establishing efficient and cost-effective care circuits.1–3
In this position paper, we will address SDB and its place within the different care circuits, the necessary elements, and the different actors involved in the use of the TM.
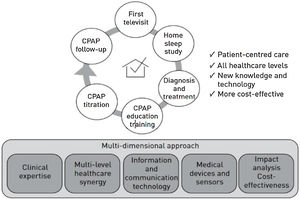
Fig. 1 and the figures in Appendix A.1 and A.2 show the main elements involved and the basic concepts underlying the implementation of TM, which must be simple and constant, and promote robust cost-effective development.
The editors of this position paper believe that following the format of the American Academy of Sleep Medicine (AASM) and the American Thoracic Society statements will allow SEPAR to more clearly express and disseminate its TM guidelines in SDB.4,5 Therefore, after the initial recommendations, the manuscript is divided into several sections that will address theoretical aspects, the point of view of suppliers—a novel aspect of our paper—, practical and technological matters, and the current legal and data protection considerations (which we also consider to be a crucial issue). Finally, an overall framework will be proposed that we believe will be useful for understanding TM in the context of clinical care, especially from the point of view of different levels of care networks.
All chapters have been drawn up on the basis of the literature retrieved from the PubMed database (2000–2018) using the following key words: continuous positive airway pressure, CPAP, mechanical ventilation, sleep apnea, information and communication technology, ICT, TM (telemedicine), sleep-disordered breathing (SDB), and the literature provided by each of the authors individually.
Theoretical considerationsThere are 2 distinct types of TM (Table 1): synchronous, i.e., a real-time interaction (video conferencing or telephone coaching); and asynchronous, which involves deferred contact (automatic electronic messaging, remote monitoring platforms).6–9 Table A.1 in the appendix shows a series of studies listed by type of TM used.
Types of telemedicine.
| Synchronous: real-time (e.g. video conferencing) |
| Asynchronous: deferred results |
| Electronic messages |
| Remote monitoring with delayed reception |
| Transmission and storage of tests |
| Access to collected therapeutic data |
| Automated care and self-management systems |
| Interactive voice response |
| Web platform access |
| Notifications via text messages |
| Questionnaire notifications. Apps |
Synchronous TM involves mechanisms by which medical care is delivered in real time, including video visits or video consultations. In this modality, the meeting is intended to function as a face-to-face visit. Video and telephone contacts are beneficial for patients in terms of avoiding the cost and time associated with travelling to the hospital or loss of hours at work.10 In many cases it could also be used to perform routine chronic follow-up of patients with CPAP or NIV, review compliance, and monitor the associated disease. This approach will be limited if some kind of physical examination is needed; however, in sleep medicine, many stable patients can be properly evaluated without a face-to-face physical examination. If necessary, adequate coordination with primary care (via care networks) could solve the problem in many cases,11,12 or perhaps a simple face-to-face visit would suffice. It is clear that both professionals and patients need training if visits, assessments, and therapeutic management are to be conducted appropriately.
The AASM has highlighted some specific considerations for this modality, the most important of which are the following: 1) the technical skills needed to apply this type of TM on an online platform with the appropriate bandwidth and support systems; 2) patient documentation, including advice about tests, treatments, and prescriptions, all administered to the same standards as face-to-face visits.13–15
In asynchronous TM, also called store and forward, the encounter between patients and the healthcare provider does not occur in real time. The asynchronous mode is used in cases in which diagnosis or consultation of the forwarded information is not urgent and can be deferred. This modality comprises the largest volume of activity today. Examples include the following: 1) electronic messages from the supplier to the patient (email, text and WhatsApp messages) to communicate appointments or decisions; 2) remote monitoring with delayed receipt of data (equipment transmitting signals); 3) storage of medical test data for later analysis; 4) access to therapeutic information stored in databases (Philips Encore Anywhere or ResMed Airview platforms), and finally 5) automated care and self-management systems, such as platforms with patient feedback systems, based on questionnaires or data collected from CPAP or NIV equipment, designed to provide advice or recommendations regarding the information obtained. Personal mobile devices (smartphones or tablets) may include applications that are related to prescribed treatments or linked to other medical devices. Data can be analyzed on the basis of a set of pre-specified criteria or filters (compliance thresholds, residual respiratory event rate, mask leaks) and automatically downloaded clinical interventions that can be pre-programmed.15–33
In this context, there are some basic considerations to bear in mind: understanding sleep as a source of health; appropriate patient selection and personalized diagnosis and treatment; finally, optimization of care circuits and management needs.
The authors mention 3 basic considerations underlying the switch from clinical care to TM: 1) it must be easy to use and it must be personalized, since complexity can sometimes lead to problems and dropout32; 2) incorporation should be gradual in general, and it should be remembered that it is not always essential in all care settings involved in patient management, and 3) TM should also assist in the work of clinical management. However, as shown in Table A.1, not all studies have reached the same conclusions, probably because of their different characteristics.
Suppliers’ point of view: current optionsThe use of interconnected health technology (eHealth) is revolutionizing the way patients and professionals interact with health systems. These technologies can be applied in different areas: they can be used to access clinical information, to promote healthy habits, and even to interact in the clinical follow-up of various groups of patients, in particular chronic cases that place a heavy burden on health services.34–36 TM is a potentially useful element in the changes that are currently being introduced. As mentioned, personalization of patients in the process is essential. Table 2 shows the various functions of TM. In this case, related to positive pressure equipments.
Basic concepts related to the application of telemedicine and positive pressure equipment.
| Devices | CPAP/BIPAP/ST/Servo ventilator/auto-CPAP/life support ventilators Diagnostic equipment | |||
| Transfer method | Pressure sensors/pneumotachographs generate a series of signals from the equipment which are transmitted to the platform via bluetooth, WiFi or 3G, | |||
| Recommended mini signals | Pressure, leaks, compliance, residual events, device settings, and tidal volume, if applicable | |||
| Other optional signals | Mean or minimum SatO2, oxygen saturation index, breathing rate, % spontaneous inspirations and expirations, technical functioning of the equipment | |||
| Save data, number of days | Summary information: unlimited. Detailed information (graphs) | |||
| Visualizations | Trend curves, tables, summaries, or graphs | |||
| Alarms (description) | Yes. User definable: usage problems, treatment problems, data reception problems, even reminders (contact with patients, other professionals, receive surveys or contact with suppliers) | |||
| Communication (route) | Bilateral. Enables shared screen communication between suppliers and professionals (for example, making comments) | |||
| Change "remote setting" | Yes, depending on model (not in life support equipment) | |||
| What clinical data can be incorporated? | Defined by default: date of birth, BMI, sex, hospital | |||
| Unlimited in a free text field | ||||
| Others | Mask type | Circuit type | Equipment type (model)/humidification | Use/data processing |
To understand the different concepts, we should remember that the technological solutions currently in use can monitor and control CPAP and NIV equipment connected via bluetooth, cellular (3G/4G) or other modems, or WiFi to platforms or information systems hosted on remote servers that provide suppliers, patients and clinicians with data, in an environment with the proper legal set-up. In this section, we will discuss 2 points: firstly, the main advantages of ICT and the possibilities it offers the clinician, the service provider, and the patient, and secondly, what technology will bring us in the future.
In relation to the first point, ICTs provide the clinician with access to complete data on the equipment in use (pressure, leaks, residual events, and compliance). Moreover, in CPAP, for example, the prescription can be adjusted remotely. In NIV, remote parameter changes are not yet definitively permitted in all patients, but this option will probably become a possibility in non-serious subjects in the near future.
Both suppliers and service providers must work together with clinical professionals in order to have an agile exchange of information. This will promote the availability of data online, which will facilitate the efficient redistribution of resources and processes.
It is absolutely essential that the patient is involved in the control of their disease. In order to achieve improved compliance, they must be empowered by setting their own objectives (self-control) and providing them with detailed information on the course of their treatment so that corrective measures can be implemented if necessary.
After current possibilities have been described, we can turn our thoughts to what technology will bring us in the future. The following points can be considered in this regard:
- 1
As mentioned above, patients must take on shared responsibility for the control of their disease. Their relationship with healthcare workers, suppliers, and service providers will improve, although personalization of treatment and the development of user-friendly technology is essential.36 The emergence of apps is another useful option today, not only in the sense of receiving data from equipment, but also in the clinical follow-up of subjects.37 This new relationship should be based on new training models implemented among the various actors involved in the procedures.
- 2
In the move toward personalized cluster therapy, the incorporation of telemonitoring will be accompanied by the generation of large amounts of data (big data) from various sources that will dictate better procedures and handling of subjects in different settings, i.e., to customize treatment.
- 3
Technology will be an essential element in the overall management of SDB, but it should be based on cooperation, information sharing, and shared responsibility among suppliers, service providers, patients, health professionals, and health managers.
- 4
The challenge now is to incorporate innovation in SDB under an appropriate legal and regulatory framework with an appropriate level of reimbursement, probably based on results and quality of services.
TM can provide many other options in the clinical management of patients with sleep apneas (Fig. 2), from the first clinical visit to the follow-up of treatment,38 all related with the current concepts of precision and P4 medicine.39,40Table 3 gives an overall comparison of current technological procedures in which TM could potentially be used in the future. This section will address CPAP equipment, new diagnostic possibilities, and finally, NIV.
Potential use of telemedicine today.
| Current procedures | Future remote procedures | |
|---|---|---|
| Diagnosis | Hospital PSG | PSG/RP remote transmission Smartphone with a variety of built-in sensors |
| Home PSG (RP) | New equipment with multi-day logs and remote transmission (future) | |
| Titration, if applicable, and treatment | Hospital PSG | Remote titration and settings |
| Simplified home devices | Automatic devices with remote transmission | |
| Treatment using automatic devices | ||
| Follow-up | Hospital visits | Video conferencing |
| In an outpatient setting by medical personnel/nurse | Apps |
Proper understanding of TM in the context of current CPAP equipment can only be achieved with an in-depth knowledge of conventional equipment. Current devices feature significant improvements in their functioning, in addition to a number of telematic features (Table A.2). Equipment has been developing very rapidly in recent years and ever smaller devices are becoming available, with leak compensation and memory cards that transmit data for CPAP monitoring (leaks, residual events, pressures, and compliance). In addition, new features have been developed, such as more convenient ways of delivering flow and the ability to adjust various parameters remotely.
DiagnosisThe technology is now sufficiently advanced to perform multiple telematic interventions (Fig. 2).41,42Table 3 shows standard procedures and new initiatives in patient management. The transfer of home diagnostic procedures to the internet is feasible43–47 and helps avoid testing in the hospital, which is more expensive and less “real” as the subject is not in their usual setting.
Furthermore, the use of smartphones with built-in sensors (for example, a pulse oximeter) can capture not only O2 saturation data, but also respiratory movements or position.48–51 It should be borne in mind that diagnostic procedures are changing rapidly, as can be seen from the study recently published by Han et al.,52 which discusses some very different options (Fig. A.3): new skin sensors, connected telematically to a laptop, were used collect many of the signals analyzed during traditional sleep studies. According to the AASM, medical professionals have the same responsibilities towards their patients during simplified telematic studies as they do during conventional studies.53 With regard to training and certification, there are currently a number of telematic options available for remote education and support.38,54,55 Finally, 2 points must be emphasized. First, the need for teaching TM in universities, not only in general terms, but also specifically for each entity where it is required.56 Second, with regard to equipment, new options need to be considered, such as the possibility of registering multiple recordings during the night.57
Follow-upAs mentioned in the theoretical section, some synchronous and asynchronous strategies are summarized in Table A.1. Their results are partly contradictory, probably due to the short follow-up time and the different technologies used, and few cost-effectiveness studies are available, all of which complicates their transfer to the health system. It is therefore necessary to work gradually towards this goal, building on solid foundations in order to take advantage of the great potential of TM as soon as possible. In this regard, a study that highlights the difficulties of implementation was recently published by Hwang et al. In this study, the authors developed a randomized clinical trial with a large number of subjects and evaluated remote monitoring of CPAP parameters with automated patient responses and web-based education (Tele-OSA). The usefulness of TM in improving short-term CPAP compliance in patients with very poor baseline compliance was demonstrated.31
Mechanical ventilationNIV devices have also improved greatly in recent years, and new features have been incorporated (Table A.3). Home NIV is an established treatment for patients with hypoventilation for various causes (neuromuscular and thoracic diseases), obesity syndrome with or without SAHS, and others. It usually starts with an outpatient visit with adaptation and training to achieve appropriate comfort parameters.58–62 However, some authors have initiated NIV remotely in the patient’s home.63,64 Subjects requiring NIV are usually complex, and it should be noted that leaks, asynchrony, central events, glottic closure, changes in upper airway resistance, or secretions may occur during nighttime NIV. All these events can lead to desaturations, awakening, alterations in sleep architecture, and poor nighttime adherence. In addition, it should be noted that all ventilators are different and, as a result, it is very difficult, if not impossible, to learn all the algorithms used, and this can cause problems or even errors. It is worth remembering that each supplier programs its ventilators with different parameters or settings, so medical staff need to know and understand the equipment to optimize its clinical performance.65–68
After daytime adaptation, ventilator settings should ideally be adjusted in a sleep lab.69,70 It is clear, then, that due to the clinical complexity of patients and the technological complexity of current NIV equipment, the ventilatory parameters must be established by experts, and the correct settings are not always achieved during the first night of titration. Parameters must therefore be adjusted gradually, and TM has great potential in this field.71
Data on usage, such as leaks, pressures, tidal volume, and residual events, can be downloaded from NIV devices. Furthermore, after the device data are dumped into the corresponding software, flow curves, pressure, tidal volume, and leaks can be evaluated in detail, and patient-ventilator asynchronies can be evaluated.72,73 The integration of various parameters such as nighttime oximetry will probably reduce the number of sleep studies needed to adjust ventilation.68
Also, as in CPAP, signal transmission for remote patient monitoring can be incorporated via web platforms that collect daily data from the equipment.74 In this way, interventions such as telephone calls can be made, if necessary. However, caution must be exercised: commercial devices use different data transmission technologies, and there is no clear industry standard. Although the possibility exists, it is not feasible at this time to remotely adjust ventilatory parameters when the treatment is applied for life support (unlike CPAP). However, in the case of NIV, the data provided by the devices are very useful and can serve as a basis for adjustments initiated by health professionals.
As mentioned in previous paragraphs, TM needs to be simple and very user-friendly. For this reason, more and more manufacturers are incorporating different forms of remote connectivity into their devices, including WiFi, 3G, and bluetooth with a cloud web platform. Ventilators automatically transmit data at a certain frequency when the device is not in use, and the clinician then can access it using a secure code. The main advantage of these platforms is that they can be configured to provide only the data that the clinician is interested in reviewing, thus simplifying the data uploading process. Alarms can also be set to alert the provider or clinician to certain events (hours of use, leaks, volume/minute, residual events, etc.). However, a bench test of various ventilators identified significant differences, so they must be carefully evaluated.72,73,75–77
To date, despite the paucity of published studies, evidence suggests that the data retrieved from ventilators, while only indicative, have been useful in monitoring different clinical conditions78–85 (Table A.4). Therefore, more studies are needed to address short- and long-term monitoring. For this reason, several clinical trials currently underway in France, the UK and the Netherlands will shed more light on this issue. The French health system, in which remote NIV monitoring is the most widespread, has established the following recommendations:
- A
Telemonitoring must be prescribed by the physician and patients must give their consent.
- B
All telemonitoring systems must provide at least the following parameters: daily use, respiratory rate, volume/minute, residual events, and leaks.
- C
Telemonitoring is a medical act, so the clinician must check the default alerts and, if necessary, establish an action plan for the patient.
- D
Patients must be included in a treatment education program during their telemonitoring period.
- E
Healthcare professionals and the telemonitoring supplier must be paid for their services, so that the work carried out in this care modality is recognized.
Thus, it is essential to involve and integrate other departments, such as home care, manufacturers, suppliers of home respiratory therapies, primary care, social work and, of course, health professionals (Fig. 1).
With regard to TM in overall terms, 2 very recent studies came to partly divergent conclusions, highlighting the difficulties of obtaining definitive conclusions in this field. One, published by Schoch et al. found that the application of TM during the first month did not have a positive impact on compliance.86 The other, by Lugo et al., working in a virtual sleep unit based entirely on telemedicine in which patients were always managed remotely (including initial diagnosis, treatment, and follow-up), demonstrated the utility and cost effectiveness of this new technological tool.87
Legal, regulatory, and data protection issuesFrom a legal point of view, medical treatments for SDB should observe the following: 1) regulatory standards for medical devices used for these treatments and CPAP supplier management; 2) patient involvement in the process (informed consent); and 3) patient data collection and transmission via the most modern TM systems. Table 4 outlines the most important points.
Legal, regulatory, and data protection issues.
| Regulatory control |
| Compliance with manufacturing, import, and distribution requirements in Spain and the EU |
| Public hospitals/health services periodical tender |
| Patient involvement |
| Identification of medical professional |
| Information on the use and delivery of pressurized equipment |
| Data processing by the physician |
| Patient response to unforeseen or urgent circumstances |
| Data collection and transmission using any type of telemedicine device |
| Pseudonymization and encryption of personal data |
| Confidentiality |
| Availability and access to data in the event of an incident |
| Regular verification, evaluation, and evaluation of technical, organizational, and safety measures |
| Informed consent |
| Data responsibility and processing: hospital/medical consulting rooms |
Regulatory control of CPAP equipment, classified as medical devices, is governed in Spain by Royal Decree 1591/2009, in which they are defined as: any instrument, device, equipment, software, material, or other item, used alone or in combination, including software designed by the manufacturer for specific diagnostic or therapeutic purposes, and required for the proper functioning of devices intended for use in human beings. Furthermore, in accordance with this legislation, an accessory to the medical product is an article specifically intended by the manufacturer to be used together with a product so that that product can be used according to its intended purpose. This regulation is in accordance with European Regulation (EU) No 2017/745 of the European Parliament and of the Council of 5 April 2017 on medical devices. These regulations set out certain obligations that must be met for products of this type, summarized as follows: 1) compliance with manufacture, import, and distribution requirements within Spain and the European Union and 2) the CE mark of conformity (regulated by Directive 93/68/EEC).
The main commercial enterprises operating in our country are obliged to comply with such requirements. However medical professionals and health institutions must be aware of these obligations and demand that they are met. Furthermore, paragraph 5 of the Annex to Royal Decree 1030/2006 of 15 September 2006, establishing the portfolio of common services of the National Health System and the procedure for its updating, includes the indication, prescription and conduct, as applicable, of diagnostic and therapeutic procedures. Therefore, public hospitals and health services regularly publish invitations to tender for public sector contracts for the management of home respiratory therapy and other assisted ventilation techniques, which are currently governed by Law 9/2017 on Public Sector Contracts.
The patient's involvement in the CPAP therapy process (informed consent). In accordance with State Law 41/2002, of 14 November, Basic Regulation of Patient Autonomy and of Rights and Obligations in Information and Clinical Documentation, the treatment of CPAP and other similar sleep disorders requires informed consent from the client. This can be obtained verbally if the procedures are deemed not to present risks or disadvantages that might have a noticeable and predictable negative impact on the patient's health. It is therefore not mandatory, but it is advisable, to obtain the patient's authorization in writing.
In any case, the attending physician must always record the events and circumstances relating to the entire care process for such therapies and the patient's agreement must be noted “in real time” in the patient's medical history, and the patient must also be informed that they can withdraw their consent to the indicated therapy at any time. We must remember that the patient always has the right to access and obtain a copy of his or her medical record. In written documents that collect patient informed consent, it is advisable to include at least the following sections: 1) identification of the reporting physician, 2) data on the use and transmission of CPAP data from the patient's home (utilities, parameters, etc.), 3) processing in the hospital or physician's office of data obtained/transmitted, and 4) patient response in unforeseen or urgent circumstances.
The collection and transmission of patient data via the most modern TM systems. Recently enacted European legislation, namely, the General Data Protection EU Regulation 2016/679, reinforces the protection of natural persons. This regulation was transposed into Spanish law by Organic Law 3/2018. In our case, TM systems and applications designed to transmit CPAP data or similar information must guarantee the highest security measures to prevent data breaches including, but not limited to, the following: 1) the anonymization and encryption of personal data; 2) the ability to ensure ongoing confidentiality, integrity, availability and resilience of treatment systems and services; 3) the ability to quickly restore availability of and access to personal data in the event of a physical or technical incident, and 4) regular verification, evaluation and assessment of the effectiveness of technical and organizational measures to ensure treatment safety.
If such data are transmitted or are accessible from countries that are not members of the European Union (hosted servers or service providers in third countries), steps must be taken, in advance, to verify that the country in question offers similar guarantees to those of the European Union. Finally, 2 important issues in this type of therapy and the teletransmission of the data obtained must be addressed: 1) the patient's consent to the processing of their data is consubstantial and inseparable from their consent to treatment, so it is advisable to unify both in the same document (and if they are discussed in 2 different documents, provide them at the same time) and 2) the hospital or medical consulting room is always responsible for processing the medical data obtained and transmitted, while the suppliers involved (the manufacturer, the service or maintenance supplier, etc.) shall be contracted for such purposes, and must therefore sign express agreements with that hospital or medical consulting room, in accordance with the requirements of EU Regulation 2016/679.
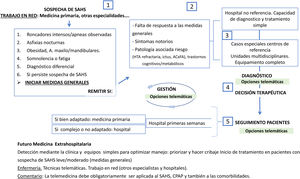
Overall structural frameworkCurrently, the most important issues in SDB, and in SAHS in particular, are waiting lists and costs, associated diseases, patient follow-up, and inadequate coordination between primary care, hospitals, and suppliers. Finally, it should be borne in mind that NIV is an important factor, and as such represents the future of respiratory medicine, and requires a high level of preparation.
Therefore, to care for all patients, coordination among primary and specialized medicine and suppliers is essential to avoid destabilizing the system. This balance is paramount. The implementation of TM can be widespread, as shown in Figs. 1–3 and in Figures A.1 and A.2, which show different options.
Fig. 3 is an example of a potential structural framework, combining TM with standard clinical practice. Primary care detects and treats basic problems; non-reference hospitals, using unsophisticated technology, manage non-complex cases, and referral hospitals treat the most complicated patients. Follow-up is personalized to the needs of each patient. The use of TM in NIV according to the protocol established by SEPAR will certainly be very useful.
In this setting, as can be seen in Fig. 3, TM and new technologies (as the tools they are) will be very useful if they are properly implemented. At present, TM and ICT have been implemented for monitoring and treatment, and it use for visits and consultations is expected to increase significantly, now that the technology is available: virtual units have been set up and telematic meetings are held in various hospitals and offices with professionals seeing patients remotely. New sensors and equipment will also be used for diagnostic procedures. It is worth repeating the importance of careful evaluation in the implementation of these systems, taking into account the various clinical options and the actors involved, and thus ensuring that TM is both efficient and effective.
Finally, and this is a very important consideration: the COVID-19 pandemic has highlighted the need for TM and has enhanced teleworking in different fields of clinical practice and teaching. It is almost certain that other options that have not yet come to light will be developed soon.88–90
Conflict of interestsJosep M. Montserrat Canal has received support from Philips for one of his researchers. Javier González-Cappa and María Tato Cerdeiras (Philips Ibérica, S.A.) were not involved in the final conclusions of the manuscript. Monique Suárez-Girón, Carlos Egea, Cristina Embid, Monica Matute-Villacís, Luis de Manuel Martínez, Ángel Orteu, Olga Median declare that they have no conflict of interest.
FundingInstituto de Salud Carlos III (PI17/01068).
Please cite this article as: Montserrat Canal JM, Suárez-Girón M, Egea C, Embid C, Matute-Villacís M, de Manuel Martínez L, et al. Posicionamiento de la Sociedad Española de Neumología y Cirugía Torácica en el uso del la telemedicina en los trastornos respiratorios del sueño y ventilación mecánica. Arch Bronconeumol. 2021;57:281–290.