The association between some factors of the familial and social environment with smoking in non-student adolescents with asthma has not been explored. The aim of the study was to determine the association between family structure, educational level, parental approval of smoking, parents who smoke, and smoking friends with smoking in non-student adolescents with asthma.
Subjects and methodsIn a cross-sectional study, data were obtained by means of a structured questionnaire applied to 4778 non-student adolescents aged 13–18 years. Diagnosis of asthma was performed using a questionnaire based on the International Study of Asthma and Allergy in Childhood questionnaire. The smoking habit was determined by application of a self-administered questionnaire. Odds ratios (OR) were determined for smoking using logistic regression.
ResultsFrom the total sample, asthma prevalence was 6.6% and of active smoking, 34.2%. Age at initiation of asthma symptoms was 5.15±3.52 years, and that of active smoking was 13.65±2.07 years. Percentage of non-intact family (40.1% vs 32.7%) was greater in the group of adolescents with asthma. Logistic regression models show that parental approval of smoking (adjusted OR=5.57; 95% confidence interval=2.48–12.51) and smoking friends (adjusted OR=2.92; 95% confidence interval=1.04–8.19) are associated with smoking in non-student adolescents with asthma.
ConclusionIn this study, parental approval of smoking and having friends who smoke appear to be associated with smoking among non-student adolescents with asthma.
La asociación de algunos factores del entorno familiar y social con el tabaquismo en adolescentes no escolarizados con asma no ha sido estudiada. El objetivo de este estudio fue determinar la asociación de estructura familiar, nivel de estudios, aprobación parental del tabaquismo, progenitores fumadores y amigos fumadores con el tabaquismo de los adolescentes no escolarizados con asma.
Sujetos y métodosEn un estudio transversal, se obtuvieron datos mediante un cuestionario estructurado aplicado a 4.778 adolescentes no escolarizados, de edades comprendidas entre 13 y 18 años. El diagnóstico de asma se estableció con el empleo de un cuestionario basado en el cuestionario International Study of Asthma and Allergy in Childhood. El hábito tabáquico se determinó con la aplicación de un cuestionario autoadministrado. Se determinaron las odds ratios (OR) para el tabaquismo utilizando una regresión logística.
ResultadosEn la muestra global, la prevalencia del asma fue del 6,6% y la del tabaquismo activo del 34,2%. La edad de inicio de los síntomas de asma fue de 5,15±3,52 años, y la del tabaquismo activo fue de 13,65±2,07 años. El porcentaje de familias no intactas (40,1% frente a 32,7%) fue mayor en el grupo de adolescentes con asma. Los modelos de regresión logística ponen de manifiesto que la aprobación parental del tabaquismo (OR ajustada=5,57; intervalo de confianza del 95%=2,48–12,51) y los amigos fumadores (OR ajustada=2,92; intervalo de confianza del 95%=1,04–8,19) se asocian al tabaquismo en los adolescentes no escolarizados con asma.
ConclusiónEn este estudio, la aprobación parental del tabaquismo y el hecho de tener amigos que fuman muestran una asociación con el tabaquismo en los adolescentes no escolarizados con asma.
Although some research indicates a reduction in the prevalence of smoking in certain Western countries,1 recent studies show that the incidence of smoking among adolescents continues to increase and constitutes an important public health problem.2,3
The negative consequences of smoking on health has been widely documented, including 5 million deaths annually related with the consumption of tobacco and an increased risk for diseases such as lung cancer, cardiovascular diseases, bronchitis and asthma, among others.4–7 Asthma in adolescents is currently one of the most frequent chronic respiratory diseases.8,9 The negative effects of asthma on a person's quality of life include the limitation of physical activity, frequent hospitalizations, school absenteeism and poor academic results, among others.9–11 Despite previous research indicating that individuals with asthma can present fewer respiratory symptoms and fewer hospitalizations when they live in a smoke-free home and have family support for their treatment,12,13 some recent reports about the prevalence of cigarette use indicate that adolescents with asthma smoke significantly more than healthy adolescents.14–16
Some theories have been proposed to explain the greater prevalence of smoking in adolescents, although no consensus has been reached.14,17 An interesting proposal is that the lower level of studies and parental approval of smoking could explain the high prevalence of smoking in this population group, as shown in some research papers.18 Nevertheless, there have been no studies analyzing the relationship between level of studies and parental approval of smoking with tobacco consumption in adolescents with asthma who do not attend school.
Adolescence is a stage in life during which habits and behaviors may be acquired that are health risks. According to some authors, individuals with lower level of studies have a greater probability for developing some diseases and behaviors or habits that entail risk for their health, such as smoking.19–21
Keeping in mind the relationship that exists between actively smoking and the development or aggravation of asthma,22 there is a clear need to carry out studies in order to determine to what extent certain factors favor the development of smoking in adolescents with asthma. Due to this reason, we have developed this study with the aim to determine the relationship between family structure, level of studies, parental approval of smoking, parents who smoke and friends who smoke with the tobacco habit of adolescents with asthma who do not attend school.
Subjects and MethodsWe carried out a cross-sectional study based on population research. A total of 5000 adolescents were invited to participate in a previous, more extensive, longitudinal study done between January and December of 2009, with the main objective of detecting and preventing addictions. Out of this group, the questionnaires of 1321 adolescents were not included in the final sample. The reasons for exclusion were that they were either incomplete (10%), contained incorrect information (7%), or corresponded with adolescents who had suffered asthma at some point in their life but who did not meet the established criteria for the diagnosis of asthma in the present study (83%). Thus, we analyzed the data of 3679 adolescents aged between 13 and 18. The sample corresponded with approximately 30% of the adolescents of our region. The data were analyzed in 2010 in the Tampico-Madero area of Mexico. This region with 2 cities is located in the southern part of the state of Tamaulipas, on the Gulf coast of Mexico, and is situated 542km to the northeast of Mexico City. It covers an area of 1492.7km2 and a population of 605,431 inhabitants.
The response to the questionnaire was done with the collaboration of staff that had been especially prepared. The staff who administered the survey was trained with presentations and workshops in order to increase their understanding of the group of participants and to establish common criteria for the comprehension of certain elements of the questionnaire, such as those related with asthma and smoking.
The sample of adolescents who did not attend school was made up of young people who resided in different neighborhoods of the participating cities and were not included in the regulated school system. The questionnaires were administered at the adolescents’ homes, work centers, sports/leisure areas, or other public places including parks, social centers, etc.
In addition, we obtained informed consent from all the adolescents and their parents or guardians before participating in the study. At all times, the adolescents had the option to abandon the study, even after having completed the questionnaire.
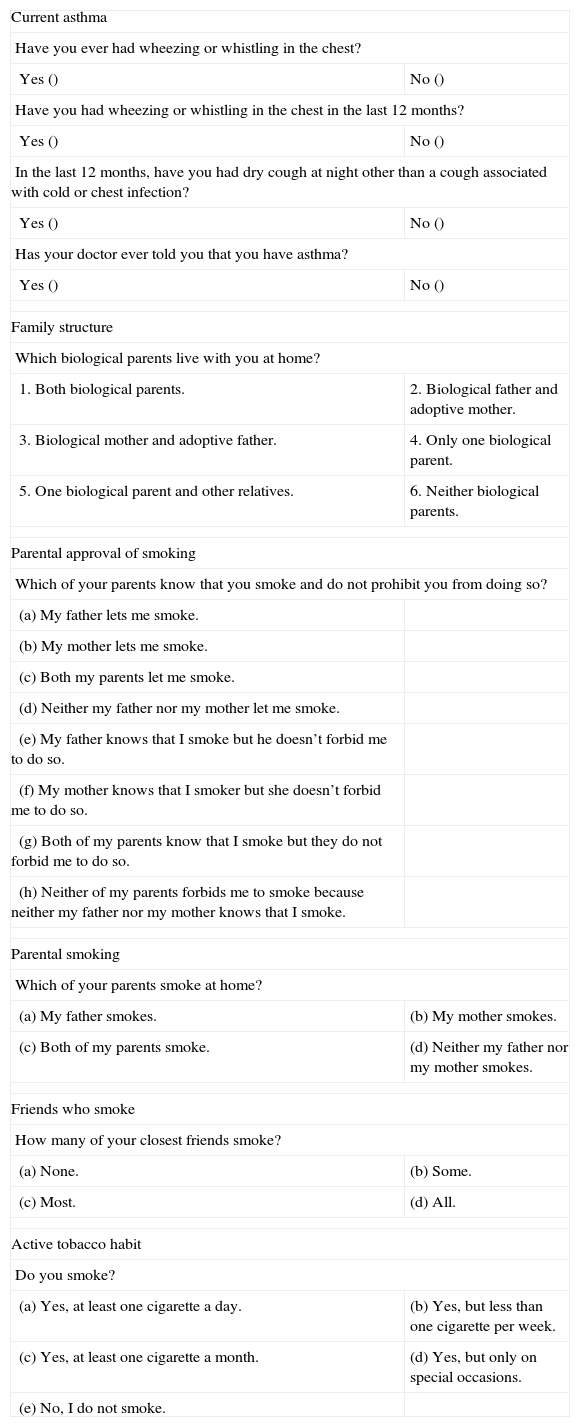
Obtaining InformationWe used a survey based on the one used in the International Study of Asthma and Allergic Diseases in Childhood. Said program was developed to provide greater validity to the epidemiologic studies about asthma, allergic rhinoconjunctivitis, and atopic excema.23 With the aim to determine the level of comprehension of the questions of the survey, we carried out 2 pilot studies with a difference of 15 days between them. Each of these studies interviewed 20 adolescents. The coincidence was 85%. In the questionnaire, we included general questions related with sociodemographic data. The questions were close-ended, multiple choice, and binomial.
Parameters of InterestCurrent AsthmaThe adolescents were classified as affected by asthma if they had an affirmative response to the 2 following questions: (1) have you had wheezing or whistling in your chest in the last 12 months? and (2) has your doctor ever told you that you have asthma?
Family StructureThis variable was defined depending on the presence of the biological father, biological mother, or both biological parents in the adolescent's home.
Level of StudiesThe level of studies was determined according to the number of academic years of schooling, in the following manner: (1) unacceptable, if the academic level was less than complete secondary education; and (0) acceptable, if the academic level was higher than complete secondary education.
Parental Approval of SmokingIf at least one of the parents allowed their teenager to smoke, this was considered explicit parental approval of smoking. The parental approval of smoking was considered non-explicit when the adolescents indicated that at least one of the parents was aware of his/her smoking, but took no steps to impede it.
Parental SmokingIt was considered that there was parental smoking in the home if at least one of the adolescent's parents was a smoker.
Friends Who SmokedThe adolescents were considered to have smoker friends when either some or most of their friends smoked.
Active SmokerThe adolescents were considered active smokers when, at the time of the interview, they declared themselves as smokers.
Statistical AnalysisWe used dichotomic variables (yes or no) to indicate the presence or absence of a certain characteristic. We performed a descriptive analysis of these variables. We created a 2×2 contingency table, the χ2 test was applied, while the odds ratios (OR) and 95% confidence intervals were calculated to determine the association between family structure, level of studies, parental approval of smoking, parental smoking or friends who smoke and active smoking in adolescents with and without asthma who do not attend school. We used the logistic regression model for the multivariable analysis. The data were analyzed with the SPSS 19.0 statistical program. A P value <.05 was considered statistically significant.
The study was approved by the ethics committee of the Medical School of Tampico at the Universidad Autónoma of Tamaulipas.
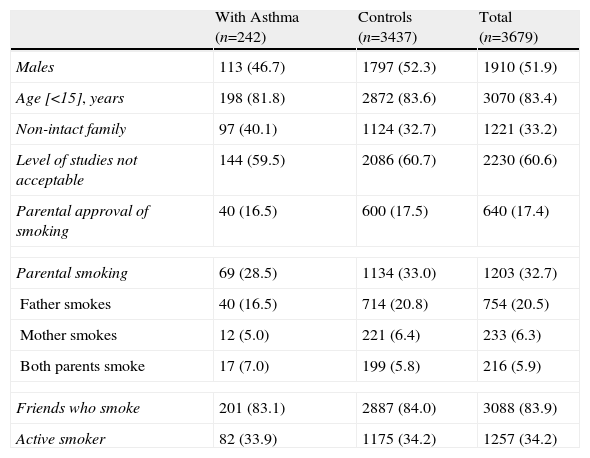
ResultsIn the total sample, the prevalence of asthma was 6.6% and that of active smoking was 34.2%. The age of onset of the asthma symptoms was 5.15±3.52, and the age of initiation in smoking was 13.65±2.07 (12.65±2.67 in the adolescents with asthma and 13.73±2.01 in those who did not have asthma). We identified a group of 3437 adolescents without asthma. These adolescents were used as a control group for the analysis. The presence of a non-intact family was registered in 33.2% of adolescents, and 17.4% declared that at least one of the parents knew that he/she smoked but did not prohibit it. Table 1 indicates the characteristics of the adolescents with and without asthma. The percentage of subjects with a non-intact family (40.1% compared with 32.7%) was greater in the group of adolescents with asthma.
Percentage Distribution by Sex, Age, Family Structure, Level of Studies, Parental Approval of Smoking, Parental Smoking, Friends Who Smoke, and Active Tobacco Habit in Adolescents With Asthma Who Do Not Attend School and Controls.a
| With Asthma (n=242) | Controls (n=3437) | Total (n=3679) | |
| Males | 113 (46.7) | 1797 (52.3) | 1910 (51.9) |
| Age [<15], years | 198 (81.8) | 2872 (83.6) | 3070 (83.4) |
| Non-intact family | 97 (40.1) | 1124 (32.7) | 1221 (33.2) |
| Level of studies not acceptable | 144 (59.5) | 2086 (60.7) | 2230 (60.6) |
| Parental approval of smoking | 40 (16.5) | 600 (17.5) | 640 (17.4) |
| Parental smoking | 69 (28.5) | 1134 (33.0) | 1203 (32.7) |
| Father smokes | 40 (16.5) | 714 (20.8) | 754 (20.5) |
| Mother smokes | 12 (5.0) | 221 (6.4) | 233 (6.3) |
| Both parents smoke | 17 (7.0) | 199 (5.8) | 216 (5.9) |
| Friends who smoke | 201 (83.1) | 2887 (84.0) | 3088 (83.9) |
| Active smoker | 82 (33.9) | 1175 (34.2) | 1257 (34.2) |
In the group of adolescents with asthma, the age at onset of the asthma symptoms in males was 4.86±3.15, while in females it was 5.41±3.81. Analogously, the age of initiation in smoking among males was 12.76±2.54, while in females it was 12.47±2.90. On the other hand, the age at onset of the asthma symptoms in teenage smokers was 4.91±3.61 and in non-smoker adolescents it was 5.28±3.48.
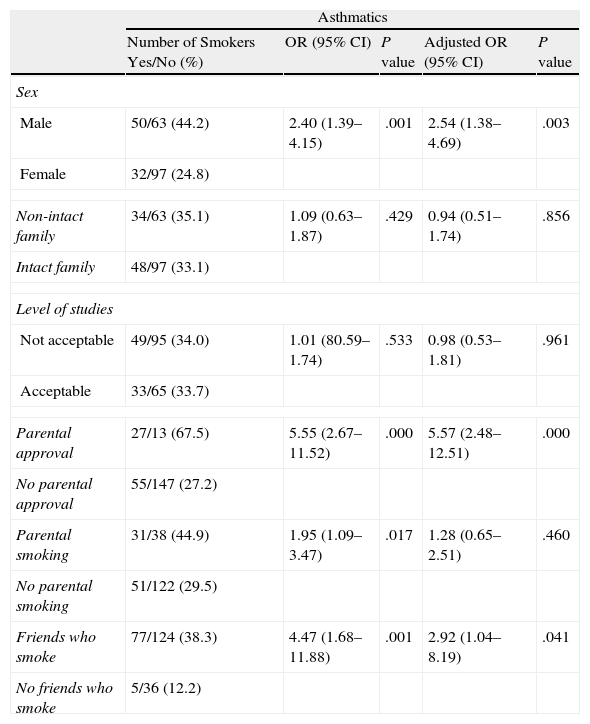
We observed a greater percentage of tobacco habit among the adolescents whose parents approved of smoking, in those whose parents were smokers and in those who had friends who smoked (Table 2).
Association Between Family Structure, Level of Studies, Parental Approval of Smoking, Parental Smoking, Friends Who Smoke and Smoking in Adolescents With Asthma Who Do Not Attend School (n=242).
| Asthmatics | |||||
| Number of Smokers Yes/No (%) | OR (95% CI) | P value | Adjusted OR (95% CI) | P value | |
| Sex | |||||
| Male | 50/63 (44.2) | 2.40 (1.39–4.15) | .001 | 2.54 (1.38–4.69) | .003 |
| Female | 32/97 (24.8) | ||||
| Non-intact family | 34/63 (35.1) | 1.09 (0.63–1.87) | .429 | 0.94 (0.51–1.74) | .856 |
| Intact family | 48/97 (33.1) | ||||
| Level of studies | |||||
| Not acceptable | 49/95 (34.0) | 1.01 (80.59–1.74) | .533 | 0.98 (0.53–1.81) | .961 |
| Acceptable | 33/65 (33.7) | ||||
| Parental approval | 27/13 (67.5) | 5.55 (2.67–11.52) | .000 | 5.57 (2.48–12.51) | .000 |
| No parental approval | 55/147 (27.2) | ||||
| Parental smoking | 31/38 (44.9) | 1.95 (1.09–3.47) | .017 | 1.28 (0.65–2.51) | .460 |
| No parental smoking | 51/122 (29.5) | ||||
| Friends who smoke | 77/124 (38.3) | 4.47 (1.68–11.88) | .001 | 2.92 (1.04–8.19) | .041 |
| No friends who smoke | 5/36 (12.2) | ||||
CI: confidence interval; OR: odds ratio.
The results of the bivariate analysis indicate that the parental approval of smoking, smoking parenteral and friends who smoke, were associated with smoking among asthmatic adolescents who do not attend school.
The results of the logistic regression models that included all the variables are presented in Table 2. Parental approval of smoking, and friends who smoke continued to show an intense association with smoking in adolescents with asthma who do not attend school.
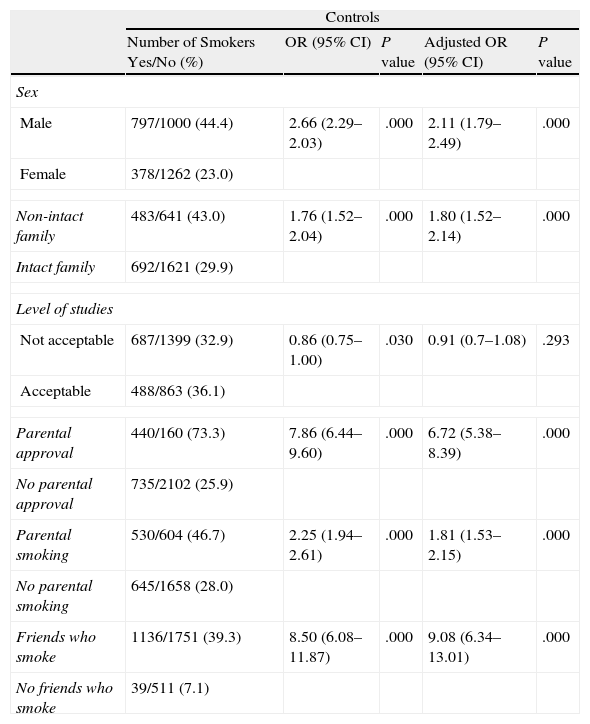
Control GroupIn the group of adolescents with asthma who do not attend school, the age of initiation in smoking was 13.73±2.01. In this group, a higher prevalence of smoking was observed in individuals who lived in a non-intact family, in those who had parents who approved of smoking, in those who had parents who smoked and in those who had friends who smoked (Table 3). In the bivariate analysis, parental approval of smoking, parental smoking and friends who smoke were associated with smoking in adolescents with asthma who do not attend school. The logistic regression analysis showed that non-intact family, parental approval of smoking, parents who smoke, and friends who smoke are associated with smoking in adolescents with asthma who do not attend school.
Association of Family Structure, Level of Studies, Parental Approval of Smoking, Parental Smoking, and Friends Who Smoke With Smoking in Adolescents Without Asthma Who Do Not Attend School (Control Group) (n=3437).
| Controls | |||||
| Number of Smokers Yes/No (%) | OR (95% CI) | P value | Adjusted OR (95% CI) | P value | |
| Sex | |||||
| Male | 797/1000 (44.4) | 2.66 (2.29–2.03) | .000 | 2.11 (1.79–2.49) | .000 |
| Female | 378/1262 (23.0) | ||||
| Non-intact family | 483/641 (43.0) | 1.76 (1.52–2.04) | .000 | 1.80 (1.52–2.14) | .000 |
| Intact family | 692/1621 (29.9) | ||||
| Level of studies | |||||
| Not acceptable | 687/1399 (32.9) | 0.86 (0.75–1.00) | .030 | 0.91 (0.7–1.08) | .293 |
| Acceptable | 488/863 (36.1) | ||||
| Parental approval | 440/160 (73.3) | 7.86 (6.44–9.60) | .000 | 6.72 (5.38–8.39) | .000 |
| No parental approval | 735/2102 (25.9) | ||||
| Parental smoking | 530/604 (46.7) | 2.25 (1.94–2.61) | .000 | 1.81 (1.53–2.15) | .000 |
| No parental smoking | 645/1658 (28.0) | ||||
| Friends who smoke | 1136/1751 (39.3) | 8.50 (6.08–11.87) | .000 | 9.08 (6.34–13.01) | .000 |
| No friends who smoke | 39/511 (7.1) | ||||
CI: confidence interval; OR: odds ratio.
As has been observed in a sample of 3679 adolescents who do not attend school, our study indicates that parental approval of smoking and having friends who smoke seem to be associated with smoking in teenagers with asthma who do not attend school. These results are similar to those obtained in studies carried out in adolescents who do attend school, both with and without asthma.3,13,14,16 As far as we know, this is the first paper that explores the risk factors for smoking in a selected sample of adolescents with asthma who do not attend school.
In previous research, it has been shown that the acquisition and the development of some habits and behaviors that are health risks, such as smoking, may be favored by the approval, either explicit or not, of the parents of the teenager, or due to lack of supervision of activities outside the home of adolescents with and without asthma.15,24 In our study, adolescents with asthma whose parents did not forbid the consumption of tobacco had a risk for developing tobacco habit that was 5.57 times higher. Mexico is considered a developing country in which, according to the last population census, there are approximately 7 million young people who neither work nor study (called NINIS in México) and another 7 million who are illiterate.25 It is obvious that parental control over the activities of adolescents and the lack of opportunities to either study or work can favor the development of habits that are health risks, such as active smoking. It is important for smoking prevention programs to be reviewed, and those strategies be reinforced, with the aim of reaching the objectives for which they have been designed. This argument is especially important when we consider the fact that smoking precedes experimentation with other drugs and the damage to the state of health is greater in adolescents who suffer asthma.
According to our data, the fact that the parents are smokers is not associated with smoking in their asthmatic teenagers who do not attend school. However, it is important to mention that in previous research it has been observed that there being parents who smoke in the home of adolescents favor their smoking.16,26 Otten et al., in their study, demonstrated that an adolescent with asthma who smokes is 4 times more likely to have parents who smoke compared with adolescents who do not smoke.27 In addition, in a previous study, we have documented that adolescents with asthma who have parents who smoke present a risk of becoming smokers that is double to that of adolescents with parents who do not smoke.15 The theory for explaining the way in which parental smoking is associated with smoking in their teenage children is not clear. It has been speculated that there is the possibility that in the homes of adolescents with parents who smoke, there may be a perception that asthma is not a serious disease, that smoking does not cause injury to one's health, or there may be a tacit approval of tobacco consumption.
The results of the studies analyzing the etiology of smoking in adolescents with and without asthma have coincided in indicating that socialization with friends who smoke is an important risk factor for the development of tobacco habit.16 Hublet et al. observed that the adolescents with asthma who socialize with friends who smoke have a risk for smoking that is 8 times higher than adolescents whose friends do not smoke.14 Our results back this observation by showing that adolescents who have friends who smoke are 2.92 times more likely to smoke than adolescents with non-smoker friends. Many theories have been proposed to explain the association between the presence of friends who smoke and the development of smoking. During adolescence, teenagers are under a lot of pressure to initiate habits or behaviors that present health risks. In our study group made up of adolescents who do not attend school and have no formal work, another element could be in play here: disappointment given the lack of opportunities to either study or work, which could be a risk factor for starting to smoke.
Previous research papers have reported that living in a home with only one or neither of the biological parents has also been associated with developing a tobacco habit.28,29 In this present study, we do not observe that the family structure was associated with smoking in adolescents with asthma who do not attend school.
On the other hand, several articles, such as those of Hublet et al., among others, have demonstrated that a low level of studies is associated with developing habits and behaviors that entail health risks in adolescents.3,14 In Mexico, according to the latest population census, the average number of years attending school in the population aged >15 is 8.6 years.14 In our study, the average number of years that the adolescent subject with asthma had attended school was 9.42±2.43 years, and in those who did not have asthma the average was 9.62±2.55 years. According to the analysis of this research, a low level of studies was not associated with smoking among the adolescents with asthma who did not attend school.
Asthma is a chronic respiratory disease; during its evolution, there are exacerbation crises that can be prevented if certain risk factors, such as smoking, are identified and eliminated in an early phase of the course of the disease.13 This is important to keep in mind because in this study the age of onset of the asthma symptoms was <2 and that of active smoking was 10. It is evident that there is an important period of time during which parents can intervene in a positive manner in the education of their children in order to avoid their acquiring habits or behaviors that put their state of health at risk, being persons with disease.
This study has methodological limitations that are important to take into account when generalizing the result. First of all, the detection of asthma and smoking was done with the questionnaires completed by the participants themselves: no objective test was used for diagnosing either asthma or smoking, such as lung function studies or carbon dioxide determinations. Consequently, the results should be interpreted with caution, given the possibility of a selection bias, information bias, or influence of confounding factors. However, in previous research, it has been demonstrated that the use of questionnaires completed by the participants themselves can be considered effective for measuring the diagnosis of asthma and smoking in epidemiological studies. Future studies should include lung function tests, carbon dioxide determinations, and other objective respiratory evaluations. Secondly, the data are only from adolescents who do not attend school.
In conclusion, the prevalence of smoking was equal in adolescents with asthma who did not attend school and in those who did not have asthma. Some risk factors for smoking within the surroundings of the adolescent, such as parental approval of smoking and friends who smoke, are equally important in the groups of adolescents with or without asthma. Consequently, smoking prevention programs should pay more attention to the family and social context of adolescents with or without asthma. It is important to raise the awareness of family members and friends of adolescents in order for them to understand that asthma is a severe disease that can worsen with active smoking.
Conflict of InterestThe authors declare having no conflict of interests.
| Current asthma | |
| Have you ever had wheezing or whistling in the chest? | |
| Yes () | No () |
| Have you had wheezing or whistling in the chest in the last 12 months? | |
| Yes () | No () |
| In the last 12 months, have you had dry cough at night other than a cough associated with cold or chest infection? | |
| Yes () | No () |
| Has your doctor ever told you that you have asthma? | |
| Yes () | No () |
| Family structure | |
| Which biological parents live with you at home? | |
| 1. Both biological parents. | 2. Biological father and adoptive mother. |
| 3. Biological mother and adoptive father. | 4. Only one biological parent. |
| 5. One biological parent and other relatives. | 6. Neither biological parents. |
| Parental approval of smoking | |
| Which of your parents know that you smoke and do not prohibit you from doing so? | |
| (a) My father lets me smoke. | |
| (b) My mother lets me smoke. | |
| (c) Both my parents let me smoke. | |
| (d) Neither my father nor my mother let me smoke. | |
| (e) My father knows that I smoke but he doesn’t forbid me to do so. | |
| (f) My mother knows that I smoker but she doesn’t forbid me to do so. | |
| (g) Both of my parents know that I smoke but they do not forbid me to do so. | |
| (h) Neither of my parents forbids me to smoke because neither my father nor my mother knows that I smoke. | |
| Parental smoking | |
| Which of your parents smoke at home? | |
| (a) My father smokes. | (b) My mother smokes. |
| (c) Both of my parents smoke. | (d) Neither my father nor my mother smokes. |
| Friends who smoke | |
| How many of your closest friends smoke? | |
| (a) None. | (b) Some. |
| (c) Most. | (d) All. |
| Active tobacco habit | |
| Do you smoke? | |
| (a) Yes, at least one cigarette a day. | (b) Yes, but less than one cigarette per week. |
| (c) Yes, at least one cigarette a month. | (d) Yes, but only on special occasions. |
| (e) No, I do not smoke. | |
Please cite this article as: Vázquez-Rodríguez CF, et al. Tabaquismo en adolescentes no escolarizados mexicanos con asma. Relación con estructura familiar, nivel de estudios, aprobación parental del tabaquismo, progenitores fumadores y amigos fumadores. Arch Bronconeumol. 2011;48:37–42.