Bronchogenic carcinoma can present metastases in any territory during its evolution, and occasionally the symptoms derived from the organ in which they settle may be the presenting form.1 Metastases in the pituitary gland are an uncommon presentation of carcinomas; bronchogenic carcinoma is one of the potential tumours that can cause them, resulting in panhypopituitarism.2
We present the case of a patient with bronchogenic carcinoma who presented with panhypopituitarism due to a single pituitary gland metastasis three months before diagnosis of the primary tumour. To the best of our knowledge, this has not been previously described in Spanish medical literature.
A 77-year-old male ex-smoker (102packs/year), diagnosed with chronic obstructive pulmonary disease, was admitted to neurology for symptoms of asthenia, hyporeflexia, generalised weakness and hyponatraemia. On admission he was conscious and oriented, with arterial blood pressure 100/50mmHg, respiratory rate 18breaths/min and heart rate 80beats/min. Cardiac auscultation was normal; pulmonary auscultation detected crackles in the lower third of the left hemithorax and expiratory wheezing. Bilateral malleolar oedema was noted during the rest of the examination. Neurological examination revealed that the upper cognitive functions were normal, as were the cranial pairs, with cautious gait and normal static balance.
Complete blood count and coagulation were normal. Biochemistry tests revealed sodium of 120mmol/l and C reactive protein of 2.6mg/dl. A prolactin of 52.25ng/ml (normal values: 2.6–19) was notable in the hormone study. Tumour markers, blood and urine protein electrophoresis and immunofixation, urinary sediment and 24-h urinary protein were normal. The electrocardiogram showed sinusal rhythm, with no conduction or repolarisation abnormalities. Hyperinflation, with increased hila of vascular appearance, was observed on the chest X-ray.
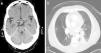
Cranial computed axial tomography (CT) revealed a 1cm suprasellar nodular lesion with well-defined borders in the upper part of the pituitary stalk, with moderate contrast enhancement (Fig. 1a). The first possibility raised was that it was in the pituitary stalk, infundibulum or adjacent meningeal structures. Brain magnetic resonance imaging (MRI) showed a 1cm suprasellar nodule, attached to the pituitary stalk that affected the hypothalamus and optic chiasm, consistent with an adenoma. There were no findings of interest on the magnetic resonance angiography of the circle of Willis. A 1.5cm×1cm×1.8cm mass was observed on the pituitary gland MRI, affecting the pituitary stalk and the hypothalamic region, consistent with metastasis. Bone scintigraphy was normal. The patient was discharged from neurology and followed-up in outpatients. Three months later, he was readmitted due to fever and bloody sputum, for which he was referred to Respiratory Medicine.
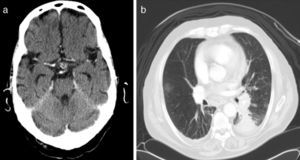
The chest X-ray did not show any significant changes with respect to the previous one. On the chest–abdominal–pelvic CT scan, a soft tissue density infiltrative lesion was noted which surrounded the left hilum and extended to the basal pyramid, with a slight decrease in volume in the left lower lobe and bilateral pleural effusion (Fig. 1b). Bronchoscopy revealed a tumour in the left sixth segment; the biopsy was consistent with undifferentiated small cell carcinoma. Spirometry showed a severe obstructive disorder, with a negative bronchodilator test. With the diagnosis of pituitary metastasis with hypopituitarism secondary to undifferentiated small cell carcinoma (stage IV), the patient began chemotherapy. He remained stable and tumour size was reduced in the first six months. However, he died one year later due to disease progression.
Pituitary gland metastases are an uncommon presentation of carcinomas, because the pituitary gland does not receive a direct systemic blood supply. Its incidence is 3.6% in 500 autopsies.2 A review from 1966 to 2004 found only 249 patients with metastatic involvement of the pituitary gland; breast and lung cancer were the most common primary tumours, occurring in two thirds of cases.3 At diagnosis, most had generalised disease, usually associated with five or more metastatic sites, especially bone; rarely, as in our case, was it the first manifestation of an occult primary carcinoma as the only site of metastasis.3 Cases secondary to bronchogenic carcinoma as a presenting form have been reported occasionally.1 Since metastatic lesions in the pituitary gland are very rare, it is difficult to distinguish them from adenomas. In fact, CT is of limited use in distinguishing benign tumours; MRI has better diagnostic specificity.
The most common clinical symptoms of pituitary gland metastases are diabetes insipidus when they occur in the posterior lobe, and hypopituitarism when they occur in the anterior lobe, as in our patient. Pituitary gland metastases are symptomatic in only 7% of patients. Diabetes insipidus, anterior pituitary dysfunction, visual field defects, headaches and ophthalmoplegia are the most commonly reported symptoms.4 Branch and Laws proposed that the triad of headache, ophthalmoplegia and diabetes insipidus was very indicative of metastases, even if the patient did not have confirmed cancer.5 Our patient did not present headache or ocular impairment. His presenting symptoms were derived from hyponatraemia secondary to hypopituitarism. Hyperprolactinaemia has been found in only 6.3% of reported cases, but very high levels generally indicate prolactinoma rather than metastases. The mean survival of these patients is 6–22 months.4
Please cite this article as: Pérez-Ferrer P, et al. Hipopituitarismo como forma de inicio de un carcinoma microcítico de pulmón. Arch Bronconeumol. 2013;49:216–7.