There is a significant lack of scientific evidence on the role of SAHS in the elderly despite the increasing ageing of the population. The objective of the present study is to analyse the current healthcare situation in Spain on the diagnosis and treatment of sleep apnoea in the elderly population (≥65 years) and its progress over the last few years.
Material and methodCross-sectional study. Healthcare information was collected on the diagnosis and treatment of patients of both sexes, ≥65 years old suspected of having SAHS and referred to sleep units (SU) between 2002 and 2008.
ResultsThere were 51,229 sleep studies performed in 16 SU. Of these, 24.3% were performed on subjects ≥65 years old (64.9% men), of which 71.5% had an apnoea-hypopnoea index (AHI) > 10 (68.6% treated with CPAP). There were no differences over time as regards mean age, mean AHI or percentage of studies done. A significant decrease was observed in the number of CPAP prescribed to men ≥65 years from 2002 to 2005 (P=.01) which subsequently increased up to 2008 (P=.01). This phenomenon was not observed in women ≥65 years.
ConclusionDespite the lack of evidence on the subject, healthcare activity due to suspected SAHS in the elderly population is intense; therefore it should be a priority to start clinical studies that may be able to answer key questions on the diagnosis and treatment of SAHS in this age group
Existe una importante falta de evidencia científica sobre el papel del SAHS en edades avanzadas a pesar del envejecimiento progresivo de la población. El objetivo del presente estudio es analizar el panorama asistencial actual en nuestro país sobre el diagnóstico y tratamiento del SAHS en individuos ≥65 años y su evolución a lo largo de los últimos años.
Material y métodoEstudio de corte trasversal. Fue recogida información asistencial sobre el diagnóstico y tratamiento de pacientes con sospecha de SAHS de ambos sexos con ≥65 años remitidos a las unidades de sueño (US) entre 2002 y 2008.
ResultadosFueron incluidos 51.229 estudios de sueño de 16 US. El 24,3% de los estudios fue realizado en individuos ≥65 años (64,9% varones), de los que el 71,5% mostró un IAH ≥ 10 (68,6% tratados con CPAP). No hubo cambios significativos a lo largo del tiempo en la edad media, IAH medio o porcentaje de estudios realizados. Se observó una disminución significativa en el número de CPAP prescritas en varones ≥ 65 años desde 2002 al 2005 (p = 0,01) que aumentó posteriormente hasta 2008 (p = 0,01). Este fenómeno no fue observado en mujeres ≥ 65 años.
ConclusiónA pesar de la escasa evidencia científica sobre el tema, la actividad asistencial por sospecha de SAHS en individuos de edades avanzadas es intensa por lo que se hace prioritaria la puesta en marcha de estudios clínicos que den respuesta a preguntas clave sobre el diagnóstico y el tratamiento del SAHS en esta franja de edad.
The population pyramid is changing in our country. In Spain, one of the countries with the oldest populations in the world, the percentage of individuals of at least 65 years of age was 20.8% in 2008 and will grow to 35% in the next decades.1 On the other hand, life expectancy has also been increasing in a parallel fashion2 and is expected to continue doing so. According to recent reports from the Spanish Institute of Statistics, life expectancy is 77 years for men and 84 years for women.1 No doubt socio-medical developments have had a decisive influence and have allowed people to reach an advanced age while maintaining good quality of life in many cases. It is therefore not surprising that older individuals demand the same diagnostic and therapeutic opportunities as younger individuals, and at the same time, due to inexorable deterioration over time, is this group of patients who monopolise the highest percentage of medical visits.3
Apnoea-hypopnoea syndrome during sleep (SAHS) affects 2–6% of the middle-aged population4–6 and 15–20% of individuals between 70 and 100 years of age,7 representing millions of people in our country. It is not known precisely, however, what percentage of sleep disordered breathing (SDB) may be due to natural deterioration associated with aging and what percentage in the elderly might be attributable to a pathological condition such as SAHS,8–16 which would have negative consequences in terms of morbidity,17–22 mortality23,24 and quality of life,25,26 and therefore to what extent this situation should be diagnosed and treated.27–29 In the absence of further evidence, the Spanish SAHS Consensus30 published in 2005 stressed the need to diagnosis and treat SAHS in elderly individuals. This recommendation was based on expert opinion because the diagnostic algorithm and treatment advocated by the Consensus was constructed from the results obtained in middle-aged individuals and was subsequently extrapolated to other age groups. A clear example of the lack of scientific evidence is that, to date, no clinical trials on the effect of continuous positive airway pressure (CPAP) treatment in the elderly with SAHS have been published,31 although this group of patients continues to be routinely diagnosed and treated in sleep units (SU).
The objective of the present study is to analyse the current healthcare situation in Spain in terms of diagnosis and treatment of sleep apnoea in the population ≥65 years of age, and its progress over the last few years, in an attempt to position this situation more accurately.
Material and MethodWe designed a cross-sectional study to collect information from various Spanish SUs using a questionnaire on healthcare activity between 2002 and 2008 (both included) in individuals older than 18 years referred for suspected SAHS from any source. The questionnaire included information on four groups: men younger than 65 years of age, men 65 years of age or older, women under 65 and women of 65 or older. The information is expressed as absolute number and percentage of the total or mean and standard deviation as appropriate. It included annual information from 2002 to 2008 (both included) for each group: number of diagnostic studies (either by full polysomnography or respiratory polygraphy), mean age, apnoea-hypopnoea index (AHI), percentage of studies with an AHI ≥10 and number of treatments with CPAP.
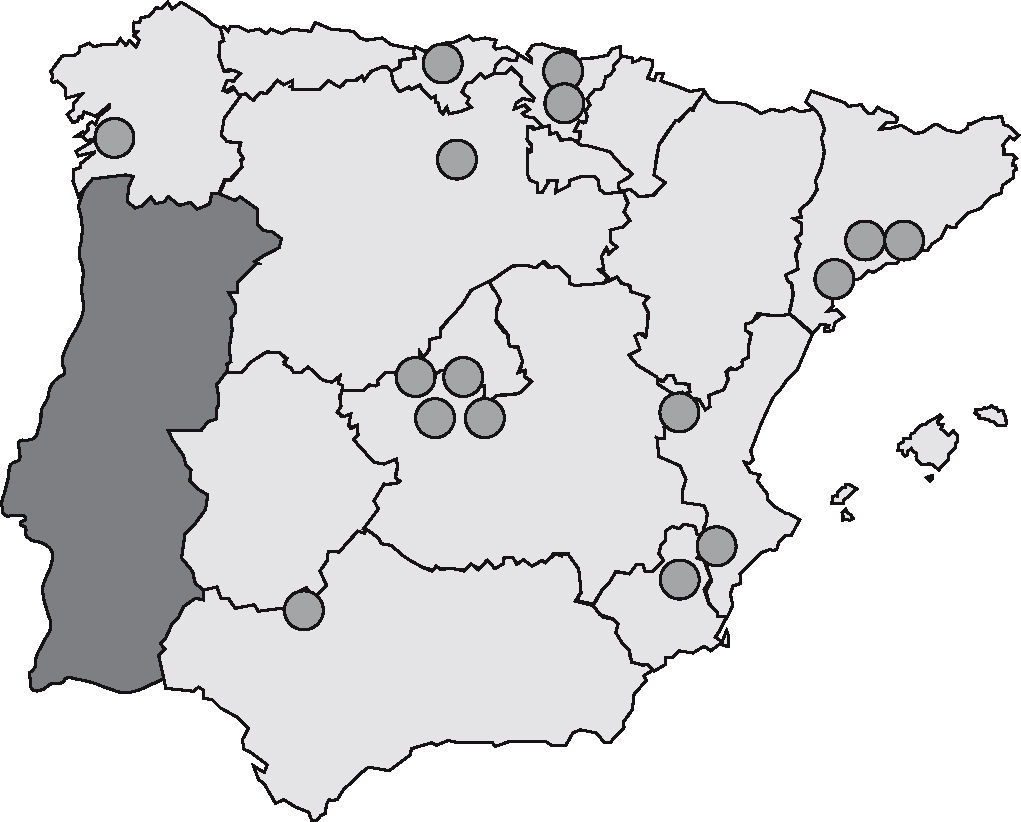
The questionnaire was sent via e-mail on three separate occasions (one initial and two reminders) to all SUs using the area directory for sleep disordered breathing, non-invasive mechanical ventilation and critical care of the SEPAR (the Spanish Society of Pneumology and Thoracic Surgery). The area directory contains most of the current e-mail address of the most relevant SUs in Spain (64 SUs). In any case, these addresses were reviewed and if any were missing they were later added to achieve maximum coverage. Figure 1 shows the geographic location of the centres whose information was ultimately collected. It seemed to be evenly distributed throughout the entire country, but the highest concentration of SU respondents were in the larger cities (Madrid and Barcelona) which was expected given the higher number of SUs in these two cities.
The SPSS version 11.0 statistical package (Chicago, IL) was used to analyse the results. The variables were tabulated as mean (standard deviation) or as absolute number (percentage of the total). To evaluate variables' progression over time (p for trend) analysis of variance for repeated measures was used, taking into account the number of measurements made over time as well as statistical adjustments necessary for this purpose. A value of P< 0.05 was considered significant.
ResultsInformation was collected from 16 SUs with a total of 51,229 diagnostic sleep studies performed between January 2002 and December 2008 (no. studies in each SU during the study period: 859–6,398; no. studies conducted annually by all SUs during the study period: 4,773–9,511). A total of 12,468 (24.3%) studies were performed on individuals ≥65 years of age, of which 8,092 were men (64.9%) and 4,376 were women (35.1%). Information relating to CPAP treatment was collected from 11 SUs (68.8%). These centres performed a total of 34,712 sleep studies with a similar value in the percentage of studies conducted in individuals ≥65 years of the total (9,401 [27.1%]). Of these 6,721 patients (71.5%) had an AHI ≥10, with 4,611 receiving CPAP (68.6%), of which 3,074 (70.5%) were men.
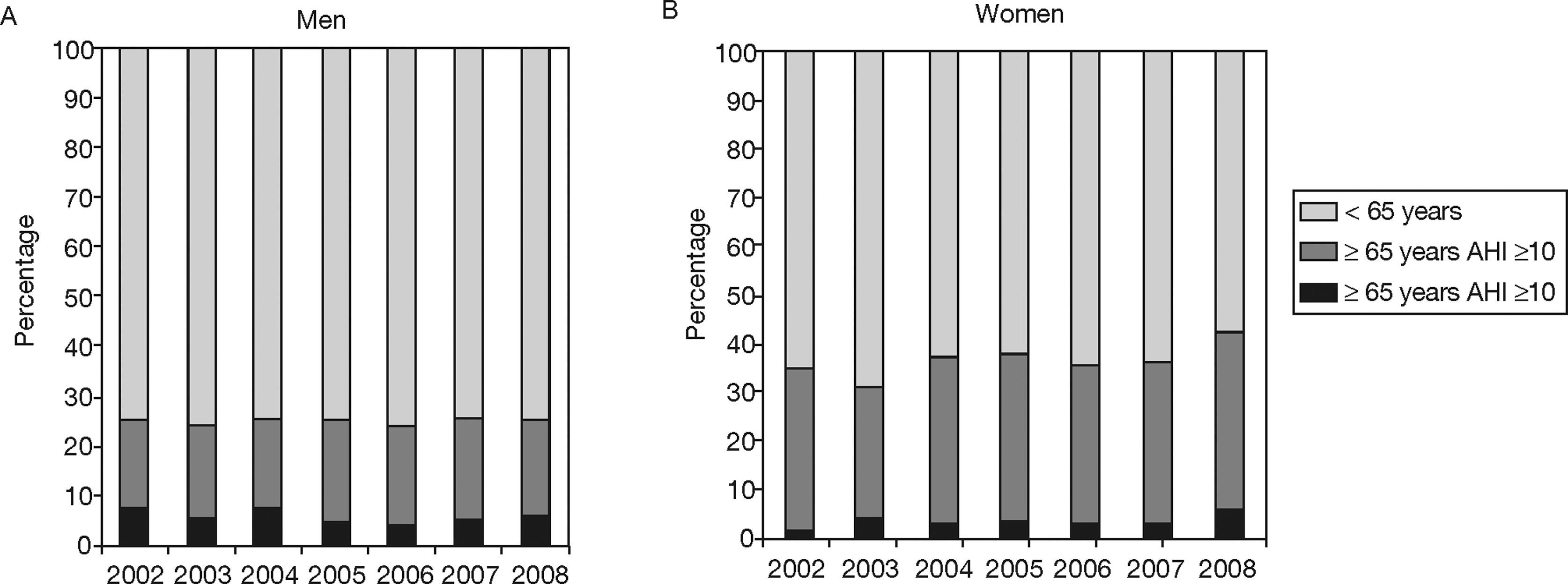
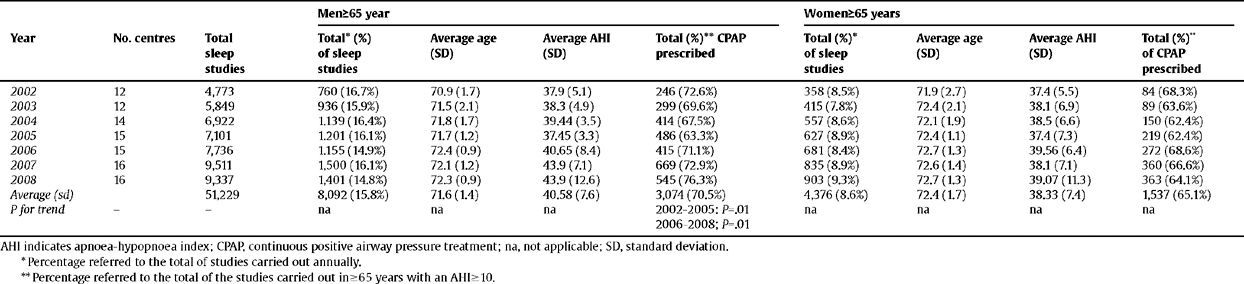
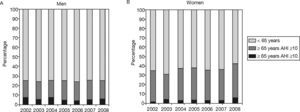
Table 1 shows the sleep tests performed, broken down by year, type, average age, mean AHI and CPAP treatment in patients ≥65 years. 70.5% of men and 65.1% of women diagnosed with SAHS (AHI ≥10) were treated with CPAP. No statistically significant differences during the study were found between ages or mean AHI of patients in any sex. Figure 2 shows the annual increase in the number of sleep studies performed in patients ≥65 years with respect to the total studies performed in patients of the same sex, and the percentage of those studies with SAHS criteria (AHI ≥10) in both men (Fig. 2A) and women (Fig. 2B). No significant differences were found over time or in the percentage of studies conducted or the percentage of patients with SAHS (AHI ≥10) in either sex.
Baseline data on the care of in individuals = 65 years in the sleep units included in the study according to age and sex of patients. Statistical trend over the years 2002–2008
| Men=65 year | Women=65 years | |||||||||
| Year | No. centres | Total sleep studies | Total* (%) of sleep studies | Average age (SD) | Average AHI (SD) | Total (%)** CPAP prescribed | Total (%)* of sleep studies | Average age (SD) | Average AHI (SD) | Total (%)** of CPAP prescribed |
| 2002 | 12 | 4,773 | 760 (16.7%) | 70.9 (1.7) | 37.9 (5.1) | 246 (72.6%) | 358 (8.5%) | 71.9 (2.7) | 37.4 (5.5) | 84 (68.3%) |
| 2003 | 12 | 5,849 | 936 (15.9%) | 71.5 (2.1) | 38.3 (4.9) | 299 (69.6%) | 415 (7.8%) | 72.4 (2.1) | 38.1 (6.9) | 89 (63.6%) |
| 2004 | 14 | 6,922 | 1.139 (16.4%) | 71.8 (1.7) | 39.44 (3.5) | 414 (67.5%) | 557 (8.6%) | 72.1 (1.9) | 38.5 (6.6) | 150 (62.4%) |
| 2005 | 15 | 7,101 | 1.201 (16.1%) | 71.7 (1.2) | 37.45 (3.3) | 486 (63.3%) | 627 (8.9%) | 72.4 (1.1) | 37.4 (7.3) | 219 (62.4%) |
| 2006 | 15 | 7,736 | 1.155 (14.9%) | 72.4 (0.9) | 40.65 (8.4) | 415 (71.1%) | 681 (8.4%) | 72.7 (1.3) | 39.56 (6.4) | 272 (68.6%) |
| 2007 | 16 | 9,511 | 1,500 (16.1%) | 72.1 (1.2) | 43.9 (7.1) | 669 (72.9%) | 835 (8.9%) | 72.6 (1.4) | 38.1 (7.1) | 360 (66.6%) |
| 2008 | 16 | 9,337 | 1,401 (14.8%) | 72.3 (0.9) | 43.9 (12.6) | 545 (76.3%) | 903 (9.3%) | 72.7 (1.3) | 39.07 (11.3) | 363 (64.1%) |
| Average (sd) | 51,229 | 8,092 (15.8%) | 71.6 (1.4) | 40.58 (7.6) | 3,074 (70.5%) | 4,376 (8.6%) | 72.4 (1.7) | 38.33 (7.4) | 1,537 (65.1%) | |
| P for trend | − | − | na | na | na | 2002–2005: P=.01 | na | na | na | na |
| 2006–2008; P=.01 |
AHI indicates apnoea-hypopnoea index; CPAP, continuous positive airway pressure treatment; na, not applicable; SD, standard deviation.
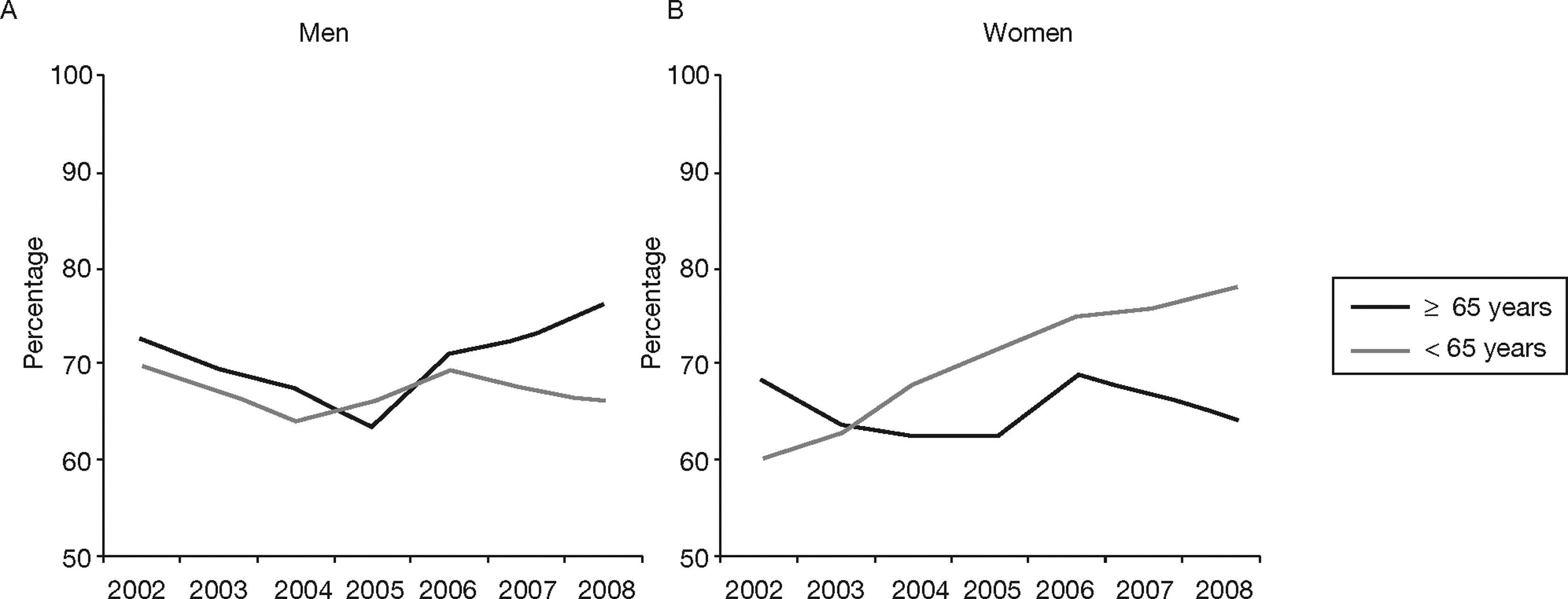
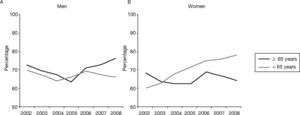
Figure 3 shows the percentage of prescribed CPAP in both sexes and by age group over the years in patients diagnosed with SAHS (AHI ≥10). In Figure 3A we can see a significant decrease (P= .01) from 2002 (72.6%) to 2005 (63.3%) in the percentage of prescribed CPAP in men ≥65 years, as well as a significant increase from this year (P=.01) to 2008 (76.3%). These differences, however, were not observed in men <65 years. In Figure 3B, there is a gradual and significant increase in the percentage of prescribed CPAP in women <65 years with SAHS (60.1% in 2002 to 78.5% in 2008), on the contrary this trend was not observed in women ≥65 years.
DiscussionAccording to the results of this study, with broad representation of SU in Spain and with information from a very large number of performed tests, one in four sleep studies with diagnostic intention due to suspected SAHS is performed in individuals ≥65 years, especially in men. The percentage of patients in this age group with SAHS (AHI ≥10), for which CPAP treatment is prescribed, is close to 70%, which was falling from 2002 to 2005 but climbed back up from then until 2008 in men.
SAHS in the elderly has a number of features that make it particularly problematic due to the limited availability of clinical and diagnostic tools specifically validated in the elderly,32 the controversial impact of this disease on prognosis23,24 and patient quality of life25,26 and the physiological increase in the number of SDB with age.8–16 While some authors claim that SAHS has a negative impact on older individuals, others such as Lavie et al. support the hypothesis that with age some individuals develop protection mechanisms that make intermittent hypoxia resistant to the adverse effects of SAHS in the cardiovascular system,33 which would at least partly explain the decrease in mortality in this age group compared with younger patients with SAHS.24 Despite this controversy, to date there have been no clinical trials on the effect of CPAP treatment in elderly patients that provide a definitive clarification of what should be the approach to take with these individuals.31 Therefore, currently the typical way professionals respond is based on experience and individual decisions, extrapolating existing knowledge from young subjects, but without solid scientific evidence to justify their decision. However, as shown by the results of this study, our care activity in patients ≥65 years with suspected SAHS in SU is intense, which leads to a paradoxical situation from the scientific point of view.
The data from this study confirm that one in four sleep studies for suspected SAHS diagnosis is performed in individuals ≥65 years, especially in men. Given therefore that at present approximately 21% of the population in Spain is ≥65 years, we can conclude that those ≥65 years are sent to SU in greater proportion than younger people. On the other hand, this percentage has not changed substantially in recent years, maintaining a very stable range (23.3 to 25.2%). This demonstrates the conviction of most SUs of the need to diagnose this group even though scientific evidence is very limited.
Contrary to what occurred with diagnostic sleep testing, in relation to treatment with CPAP in subjects ≥65 years of age, in recent years there have been changes. Although the average age of patients and the value of AHI have remained stable, the percentage of male patients with SAHS (AHI ≥ 10) who were treated with CPAP significantly decreased until 2005 (reaching its lowest point at 63.3%) and subsequently increased, also significantly until 2008 (to 76.3%). This increase was not observed in older women, but the trend, although not statistically significant, was similar to that of men until the year 2006 (a progressive decrease until 2005 with an increase in the percentage of prescriptions in the following year). There is no clear explanation, although it is possible that the publication of the Spanish SAHS Consensus in 2005,30 which stated that age itself is not a constraint to providing diagnostic techniques and necessary treatment for elderly individuals with suspected SAHS, was responsible for greater awareness among professionals. This could have resulted in a higher percentage of prescribed CPAP treatment in elderly individuals from that year.
This study focuses on a particular health care activity in individuals ≥65 years, but a mention should be made of the gradual increase in the percentage of prescribed CPAP in women <65 years (from 60% in 2002 to 75% in 2008). Although the number of studies conducted in women is less than in men, this upward trend appears robust.
The main objective of this study was to create a descriptive map of SU care over a seven-year period and reveal the paradoxical situation in the diagnosis and treatment of SAHS in the elderly. This study has proven that there is a terrible lack of scientific evidence for the social group which we attend to most frequently. Therefore it is not intended to be exhaustive in data collection. Having collected additional information on the percentage of patients studied at older ages (i.e., greater than 75 years), the type of studies, the degree of compliance with CPAP or other data, would have provided relevant information on the subject, however, there probably would have been a greater lack of response to the questionnaire from the SUs, as it would have taken them more time and effort. Another limitation of our study could be the lack of SU representation for all care activity in our country. However, figure 1 shows that the SU respondents were evenly distributed throughout the Spanish territory, with greater concentrations in large cities where there are logically more centres. Some SU, not having a computer database, did not collect information on some years (especially the early years of study) or collected some incomplete information, possibly causing data on the first years of study (2002–2004) to be less reliable. In any case, the number of diagnostic studies for which information was collected was very high, and the results obtained from the SU that reported data on CPAP treatment are similar in terms of demographic and diagnostic variables to the rest of the SUs, so we believe that it does not have a decisive influence on the study conclusions.
In conclusion, according to our results there is a clear discrepancy between the lack of practical scientific activity conducted on the impact of SAHS and its treatment in the elderly and the intense care that this group has received for several years, from the standpoint of both diagnosis and treatment. Studies are urgently needed with a maximum level of evidence to clarify the most basic questions that must be solved on this age group, especially concerning the extent of impact of SAHS and the effectiveness of treatment in the elderly. This is a more and more frequent patient group with an increasing quality of life, meaning that there are no longer any concrete arguments to not offer them the same diagnostic and therapeutic opportunities as younger individuals. For these reasons and while a greater degree of scientific evidence comes in, the Spanish SAHS Consensus (30) suggests that CPAP treatment should not be denied to an individual solely because of their age, and that other important aspects about the elderly patient should be evaluated individually and in a logical manner before making a final decision. We hope that soon this decision will no longer only be based on expert opinion.
The authors of this study wish to acknowledge the contributions of Monica Gonzalez (Hospital Marques de Valdecilla, Santander), JM Montserrat (Hospital Clínic-IDIBAPS, Barcelona), Carles Sanjuán (Hospital del Mar, Barcelona), Monica de la Peña (Hospital Son Dureta, Palma de Mallorca), Francisco Capote (Hospital Virgen del Rocío, Seville) and Ana Maria Fortuna (Hospital of the Santa Creu and Sant Pau, Barcelona).
Funding
None.
Conflict of interest
The authors affirm that they have no conflict of interest.