Tuberculosis remains a major health problem and cause of death from infection worldwide. Musculoskeletal involvement occurs in only 3% of patients.1 Primary skeletal muscle involvement without coexisting active skeletal or extraskeletal tuberculosis is extremely rare.2 We report the case of an immunocompetent patient with tuberculous pyomyositis of the primary dorsal muscles.
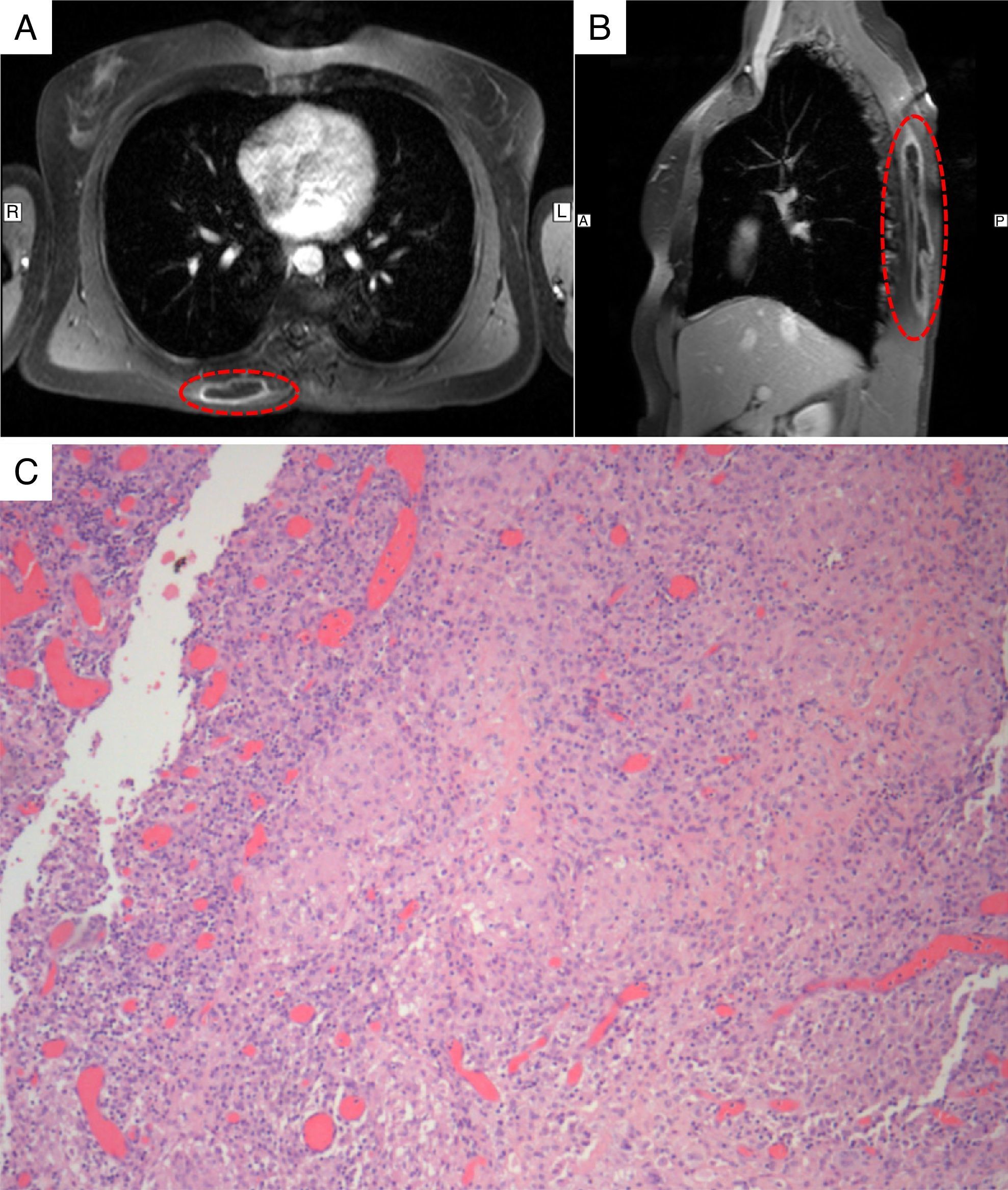
A 38-year-old female immigrant from Cape Verde, living in Portugal (Lisbon), with an unremarkable medical history, presented with pain and progressively increasing swelling in the right dorsal region over the previous two months. She denied any perceived trauma. Pain continued to intensify, despite treatment with analgesics, and she began to lose weight and sweat excessively at night. Musculoskeletal examination revealed a firm, non-fluctuant, painful swelling on the right lower dorsal region. An ultrasound showed a predominantly solid, space-occupying lesion, considered to be of muscular origin. Chest computed tomography was inconclusive. Magnetic resonance imaging (MRI) showed an extensive space-occupying lesion in the muscles of the back, highly suggestive of abscess or tumoral lesion (Fig. 1A and B), with no evidence of bone involvement. Biopsies were inconclusive, suggesting lipoma, so the lesion was finally removed, about 14 months after initial evaluation. Histology revealed extensive mixed inflammatory infiltrate and areas with epithelioid non-necrotising granulomas (Fig. 1C). Resected tissue culture revealed Mycobacterium tuberculosis complex, showing susceptibility to all first-line drugs. Serology for HIV was negative. Tuberculosis treatment was introduced and maintained for 6 months, resulting in progressive clinical improvement. On follow-up, the patient remains asymptomatic.
Axial (A) and sagittal (B) T1-weighted magnetic resonance imaging of the chest, revealing an extensive space-occupying lesion in the back muscles, with contrast enhancement of the wall. (C) Histopathological examination revealing an extensive mixed inflammatory infiltrate with numerous histiocytes and areas with epithelioid non-necrotising granulomas.
Primary muscular tuberculosis is an extremely rare condition, mostly affecting individuals with altered immune status, especially patients with acquired immunodeficiency syndrome.3 In a recent retrospective study, only 20 cases of muscular tuberculosis were reported during 2000–2010.4 The rare occurrence of skeletal muscle tuberculosis has been associated with several characteristics of this highly differentiated tissue, such as high lactic acid content, high vascularity and blood flow, and the absence of reticuloendothelial and lymphatic tissue inhibiting mycobacterial growth. The pathogenesis is still uncertain. It may result from the hematogenous dissemination of pulmonary tubercular lesions, contiguous infection from an underlying structure or, in the absence of active foci of tuberculosis elsewhere, direct traumatic inoculation. In this patient, no clinical or radiological evidence of other structural involvement or traumatic episode suggested direct inoculation. However, this patient was an immigrant from Cape Verde, a country with a high tuberculosis burden. Furthermore, tuberculosis remains an important public health problem in some areas of Portugal, mainly in Lisbon were she resides. The clinical presentation is non-specific and may mimic other diseases, leading to misdiagnosis or delay in a diagnosis that warrants a high index of suspicion. In most cases, diagnosis is made months to years after the onset of symptoms: in our patient more than a year elapsed. The gold standard for diagnosis is histology, with mandatory microbiological confirmation from the aspirated/surgical material. Medical treatment is the first-line option although surgical intervention may be useful as an adjuvant treatment. The 6-month regimen is recommended.5
Although extremely rare, tuberculosis of the primary skeletal muscle should be considered in the differential diagnosis of painful back muscle swelling, particularly in patients living in or coming from tuberculosis endemic areas.
Please cite this article as: Dabó H, Mineiro A, Carmelino J, Carvalho A, Gomes C. Tuberculosis de musculatura esquelética primaria en una paciente inmunocompetente. Arch Bronconeumol. 2016;52:340–341.