Hemoptysis has a broad differential and optimal treatment depends on identifying cause and location of bleeding. Even after an extensive work-up, including chest radiography, computed tomography, bronchoscopy, pulmonary angiography, upper gastrointestinal endoscopy and an array of serological tests, the cause of hemoptysis remains evasive in 20–30% of cases.1
An 18-year-old, non-smoker and obese (BMI – 38kg/m2) male presented with intermittent hemoptysis for six weeks, 5 episodes with each episode had approximately 5–10ml of blood. The episodes were accompanied by cough, no vomiting was reported. He had no history of breathlessness, wheeze, chest pain, palpitations, bleeding from any other site or easy bruisability of gums or skin. There were no complaints of joint pain, Raynaud's phenomenon, skin rash, photosensitivity, dryness of eyes or mouth. There was no past history of similar complaints, tuberculosis or contact with a tuberculosis patient. There was no history of loss of weight or appetite or family history of similar complaints. After multiple hospital visits and three admissions there was no resolution of his symptoms.
On examination, there were no other lesions or rashes, including telangiectasias, petechiae, or varicosities. Rest of the examination was normal. The list of investigational workup and their reports was normal (Table 1). Patient was then handed over a sputum container with instructions to wait in the hospital and inform immediately in case he had a hemoptysis episode. The patient returned 25min later with blood-tinged fluid in the container. Also, one of the finger ends had bleeding and rest other nail corners were normal and the patient said he put the finger in his mouth to stop bleeding. The sample was sent for investigations like sputum for acid fast bacilli stain and culture. Next day, patient again showed five images of blood near the sink. However, each photograph had a different colour and type of sink. On searching for hemoptysis images on the Internet, we found pictures exactly similar to the patient's images. The clinical course led us to a suspicion of factitious hemoptysis. He was referred for a formal psychiatry evaluation where it was confirmed that the patient's grandfather had recently passed away, whom he was greatly fond of. He was now seeking the attention of his father by presenting himself as being sick. Thus diagnosis of factitious hemoptysis, due to factitious disorder (FD) (previously known as Münchausen syndrome) was made.
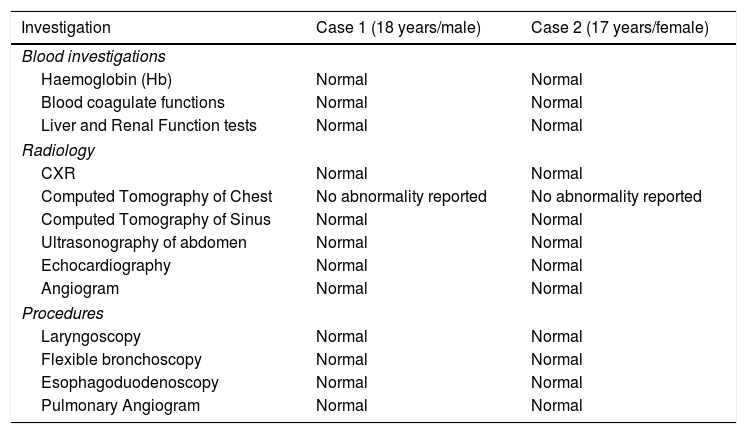
The investigation profile of both cases.
| Investigation | Case 1 (18 years/male) | Case 2 (17 years/female) |
|---|---|---|
| Blood investigations | ||
| Haemoglobin (Hb) | Normal | Normal |
| Blood coagulate functions | Normal | Normal |
| Liver and Renal Function tests | Normal | Normal |
| Radiology | ||
| CXR | Normal | Normal |
| Computed Tomography of Chest | No abnormality reported | No abnormality reported |
| Computed Tomography of Sinus | Normal | Normal |
| Ultrasonography of abdomen | Normal | Normal |
| Echocardiography | Normal | Normal |
| Angiogram | Normal | Normal |
| Procedures | ||
| Laryngoscopy | Normal | Normal |
| Flexible bronchoscopy | Normal | Normal |
| Esophagoduodenoscopy | Normal | Normal |
| Pulmonary Angiogram | Normal | Normal |
We had another case of a 17-year-old female, presented with a history of intermittent hemoptysis for four weeks, 3 episodes with each episode had approximately 10–15ml of blood. The episodes were preceded by cough, no vomiting was reported. The patient had no history of breathlessness, wheeze, chest pain, bleeding from any other site, easy bruisability of the gums or skin or menstural complaints. There were no symptoms suggestive of connective tissue disease. There was no past history of similar complaints, previous diagnosis of pulmonary tuberculosis or contact with anyone with tuberculosis. There was no associated loss of weight or appetite or family history of similar complaints. Patient had multiple hospital visits and investigations with no respite in symptoms.
On examination, there were few healed cut marks in the right forearm and the right index finger had loss of nail bed while the other nail beds were normal. There were no other lesions, rashes, telangiectases, petechiae, or varicosities. All investigations were normal (Table 1). The patient was given a sputum container and asked to immediately visit the hospital in case she has hemoptysis. The patient returned the next day with blood-tinged fluid in the container Her vitals were normal and oral examination was normal. The clinical course led us to suspicion of factitious hemoptysis. The patient was referred for a psychiatry evaluation where she reported suicidal tendencies and a need to seek her father's attention. Thus, the diagnosis of FD (Munchausen syndrome by proxy) was established.
The current case series present two patients presenting with hemoptysis, in whom the cause remained elusive despite extensive investigations. Both the cases were successfully diagnosed and managed as factitious disorder (FD).
FD is characterised by falsified general medical or psychiatric symptoms imposed on self2 which is rarely reported and often under-diagnosed. Patients deliberately disguise, simulate, or cause symptoms of an illness and/or injury to themselves. FD imposed on self (Munchausen syndrome) is distinguished from FD imposed on another (Munchausen syndrome by proxy).3 Early investigation of a possible FD can prevent patient self-harm as well as complications arising from unnecessary investigations and empirical treatments.
A systematic review of 455 cases4 reported mean age of presentation as 34.2 years with female preponderance (66.2%). Common presentations were simulated asthmatic episodes, followed by hemoptysis, acute respiratory failure (acute respiratory distress, inhalational pulmonary talcosis), cystic fibrosis, signs of collagen vascular disease, and pneumothorax. One patient was even reported to be difficult to wean from ventilator. A broad keyword search of literature published in English between January 1, 1950 and May 1, 2019 was conducted in Pubmed database was searched using the terms, factit*, munchausen*, artefacta* and artefactua*. The records with terms ‘by proxy’ or ‘imposed upon another’ were not automatically filtered out in order to ensure inclusion of case series reporting both FD and FD imposed upon another. The exclusion criteria were animal studies and clinical trials. A total of 2081 records, were retrieved for abstract review after removal of 436 duplicate. A total of 29 studies were selected for inclusion after full-text review. The bibliographies of eligible studies, review papers and the results of a GoogleScholar search utilising terms identical to the keyword search. These supplementary search processes yielded a further 5 eligible studies. Thus a total of 34 studies were included for review (Supplementary table). The most common cause of this bleeding results from self-inflicted trauma in the oral cavity. The other simulation method includes venesection and injecting their own blood in their mouth, aspirated with a syringe, either from a peripheral vein of their forearm or from a central venous catheter. The use of mixture of iodine and soap solution, as well as replacement of cherry juice in a sputum cup has been reported. Sometimes, the cause of bleeding remains obscure as patients left the hospital when they were confronted with suspicion.
Dimsdale et al. reported FD as a long-term and persistent problem related to disease perception and identity.5 It may be associated with inexplicable and/or unexpected symptoms. The diagnosis of FD can be considered by meeting the following four criteria – a pattern of presentation to others as ill or impaired; the behaviour is evident even in the absence of obvious external rewards;, the behaviour is not due to a delusional belief system or acute psychosis; and the behaviour is not better accounted for by another mental disorder.6 The cases described in this report presented with continuous hemoptysis and no obvious reward mechanism present. Yue et al. recently proposed the diagnostic algorithm for approach to a patient with unexplained hemoptysis.7 The present report concludes to avoid over investigation and identification of psychiatric risk factors in this patient population with thorough history taking.