Silicosis is a chronic progressive disease caused by inhalation of crystalline silica. Most cases develop in underground mine workers and in subjects involved in the extraction of natural stone (slate and granite). In view of the progressive emergence of new cases of silicosis in artificial quartz conglomerate workers, we performed a study to analyze the characteristics of silicosis produced by this new agent in Spain.
MethodsThe study consisted of a series of 96 cases of silicosis diagnosed according to international criteria during the period 2010–2017. We analyzed clinical, radiological, pathological and functional characteristics.
ResultsMean age of participants was 45 years; 55% had simple silicosis and 45% had complicated silicosis. Ten patients were diagnosed with accelerated silicosis, with a mean age of 33 years. Mean time of exposure to conglomerates was 15 years, and 77% had not used appropriate protection measures. Half of the patients were asymptomatic and presented different classic forms on chest X-ray and chest high-resolution computed tomography, along with ground-glass images. No lung function changes were recorded.
ConclusionsSilicosis in artificial quartz conglomerate workers occurs in a young, actively employed population, a considerable percentage of whom present an accelerated form. They have few symptoms and no functional limitations. Protection measures are scarce. It is important to characterize these features to provide early diagnosis and implement the necessary preventive measures.
La silicosis es una enfermedad crónica progresiva producida por la inhalación de sílice cristalina. La mayoría de los casos aparecen en trabajadores de minería de interior y extracción de piedra natural (pizarra, granito). Ante la progresiva aparición de nuevos casos de silicosis en trabajadores con conglomerados artificiales de cuarzo (CAC), se planteó un estudio que tuvo como objetivo analizar las características de la silicosis producida por un nuevo agente en España.
MétodosEl estudio consistió en una serie de 96 casos diagnosticados de silicosis según criterios internacionales durante el periodo comprendido entre 2010 y 2017. Se analizaron las características clínicas, radiológicas, funcionales y patológicas.
ResultadosLa edad media fue de 45 años, el 55% con silicosis simple y el 45% con silicosis complicada. En 10 pacientes se diagnosticó silicosis acelerada, con una media de 33 años de edad. El tiempo medio de exposición a los conglomerados fue de 15 años y en un 77% no se utilizaban medidas de protección adecuadas. La mitad de los pacientes estaban asintomáticos y presentaban diferentes formas clásicas en la radiografía de tórax y tomografía computarizada de alta resolución de tórax, así como imágenes de vidrio deslustrado. No se observaron alteraciones en la función pulmonar.
ConclusionesLa silicosis en los trabajadores con CAC se observa en personas jóvenes, en activo, en un considerable porcentaje de forma acelerada, con escasos síntomas y sin alteración funcional. Las medidas de protección son escasas. Es importante conocer estas características para el diagnóstico precoz y las necesarias medidas preventivas.
Silicosis, a disease caused by inhalation of crystalline silica dust, was the most lethal and sustained occupational disease epidemic in the 20th century.1 This is a progressive disease that induces pulmonary fibrosis, causing disability and even death, and for which there is no treatment. For this reason, early detection and strict control of workplace conditions are essential to modify or mitigate the clinical course.2 Occupational exposure to inhalation of silica dust occurs in many industries3 but progressive improvements in working conditions and prevention programs have turned silicosis into a disease clearly on the decline.4,5 Despite this, however, cases of silicosis have recently appeared in other hitherto untouched sectors, such as those presented by workers handling artificial quartz conglomerates.6,7 These conglomerates are composed of high concentrations of crystalline silica which, when inappropriately handled, can form suspensions of silicon dioxide (SiO2) in respirable particles that penetrate to the pulmonary alveoli.
The data on the natural history of silicosis and the validity of the different diagnostic tools have mostly been obtained from the studies carried out in underground mines, granite and slate quarries, and foundries.8,9 To date, the only publications to appear on silicosis associated with the manipulation of quartz conglomerates have been series with a limited number of cases.10 The emergence of severe cases of silicosis among workers manipulating these conglomerates suggests that we need to improve our knowledge of the natural history of the disease in this group and identify their characteristics.11
The main objective of this study was to describe the epidemiological, clinical, functional, and radiological characteristics of silicosis in quartz conglomerate workers in Spain. The experience gained by our group in the diagnosis of pneumoconiosis in coal miners12 and natural stoneworkers13 allows us to apply this knowledge to the assessment of this new form of disease expression.
Subjects and MethodsStudy DesignThis was an observational, retrospective study conducted among patients referred to the section of Occupational Pulmonology in the Lung Area of the Hospital Universitario Central, Asturias, between January 2010 and December 2017, who were employed in the handling of artificial quartz conglomerates. Although the collection of data for analysis was retrospective, the study process was fully protocolized from the start, with regard to clinical and occupational history, and functional and radiological examinations.
All patients were workers who handled artificial quartz conglomerates (AQC) and were engaged in the installation of these products in the construction sector. They came from different geographical areas of Spain and were referred to our hospital, as the national reference center, by their primary care physicians, company doctors, insurance companies, disability assessment units, or other respiratory medicine departments, for the purpose of evaluating the presence of silicosis.
The only criteria for inclusion in the study were demonstrated occupational exposure to quartz conglomerates and a diagnosis of silicosis confirmed after January 2010. The diagnosis of silicosis was based on an occupational history of exposure to crystalline silica, associated with radiologic studies with characteristic findings (standard chest X-ray with a profusion≥1/1 according to the ILO classification14) and exclusion of other possible entities.15 The study included subjects over 18 years of age, with no upper limit. We obtained the approval of the Research Ethics Committee of the Principality of Asturias (198/216).
Data CollectionA data collection protocol was designed that included: date of birth, smoking habit, anthropometric characteristics, specific occupational activity, years of exposure (start date and end date), use of preventive measures, and medical history. Respiratory symptoms, especially dyspnea measured by the modified Medical Research Council (MRC) scale, were specifically recorded.16 A complete physical examination was also performed.
A posteroanterior chest X-ray was read according to the ILO system for classification of radiographs.13 The classification proposed by Kusaka et al. was used to interpret the high-resolution computed tomography (HRCT) of the chest.17 This classification scores the shape and profusion of opacities on a scale of 0–3 for the left and right hemithorax, and on 3 thoracic levels: upper, middle and lower, with a possible total of 0–18 points. The presence and intensity of emphysema and the ground glass pattern were also recorded using a similar scale. The readings were made by agreement between 2 experienced expert assessors (a pulmonologist [CMG] and a radiologist [APG]), familiar with this type of interpretation, in order to minimize subjectivity. The lung function study included the stepwise evaluation of forced spirometry, determination of static volumes, and CO diffusion testing, performed according to the usual guidelines.18 The quantitative variables are reported as mean values and standard deviation (SD), and total number and percentage, as appropriate. The “R” v 3.5 program was used for statistical comparisons (means, SD, t-test); R Core Team (2018) (R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/). Significance was set at P<0.05.
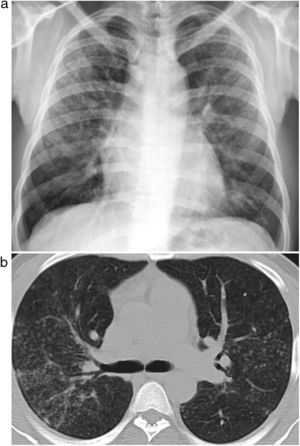
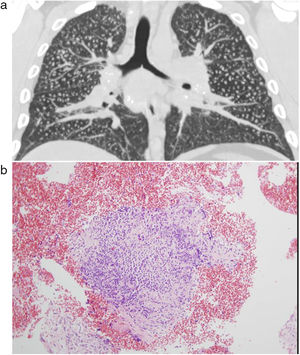
ResultsWe recruited 96 patients who met the inclusion criteria, all of whom were men with a mean age of 44 years (SD 8), ranging between 27 and 59 years. Patient provenance is shown in Table 1. Clinical presentation was distributed into 53 cases (55%) of simple silicosis and 43 (45%) of complicated silicosis. Ten patients met the criteria for accelerated silicosis. The average time of exposure to quartz conglomerates was 15 years, ranging from 5 to 34 years. In total, 77% of workers handled other rocks concurrently, mainly granite, and the average duration of total exposure to any material with silica content was 20 (SD 8) years. Eighty percent of the patients were still actively employed and exposed to the occupational risk at the time of diagnosis. A total of 77% of cases reported inadequate technical prevention measures and 74% did not use personal protective equipment. Patients with accelerated silicosis had an average age of 33 (SD 6) years, ranging from 27 to 44 years. Seven of these patients (70%) fulfilled the criteria for complicated silicosis, and 4 cases (40%) showed areas of ground glass opacities associated with interstitial nodules (Fig. 1).
Provenance of Cases by Autonomous Community.
| Autonomous Community | No. (%) |
|---|---|
| Andalusia | 15 (15.6) |
| Asturias | 11 (11.4) |
| Cantabria | 12 (12.5) |
| Castile-Leon | 7 (7.2) |
| Catalonia | 4 (4.1) |
| Galicia | 17 (17.7) |
| Murcia | 4 (4.1) |
| Basque Country | 22 (22.9) |
| Valencia | 4 (4.1) |
No.: number of cases; %: percentage of the total.
Forty patients were never smokers (42%), 29 were former smokers (30%), and 27 were active smokers (28%). Accumulated tobacco exposure among the former smokers was 19 (SD 14) pack-years and 15 (SD 7) pack-years among active smokers. Half of the patients were asymptomatic with a normal physical examination. The other half was divided into a minimum degree of dyspnea on exertion in 42 cases (MRC scale I) and a moderate degree in 6 patients (MRC scale II). Twenty-three percent of patients reported cough, and none of the cases fulfilled criteria for “chronic bronchitis”. Lung function studies performed are listed in Table 2 and showed values largely within the reference ranges.
Lung Function at Time of Diagnosis.
| Variable (%), Mean and SD | Total Sample | Accelerated Silicosis | Chronic Silicosis |
|---|---|---|---|
| FVC | 92.5 (13.6) | 91.3 (14.1) | 92.7 (13.6) |
| FEV1 | 93.1 (13.8) | 89.8 (10.8) | 93.5 (14.1) |
| TLC | 90.9 (13.1) | 78.0 (7.6) | 92.5 (12.8) |
| DLCO | 88.9 (16.5) | 79.4 (9.1) | 91.3 (17.2) |
Values are given as mean and SD.
No statistically significant differences were observed between the groups of accelerated and chronic silicosis.
DLCO: diffusing capacity of the lung for CO; FEV1: forced expiratory volume in 1 second; FVC: forced vital capacity; SD: standard deviation; TLC: total lung capacity.
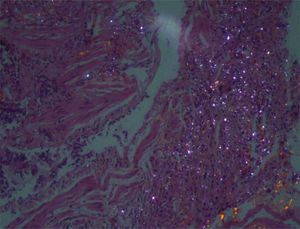
Tables 3 and 4 show the radiological readings of the chest X-ray and chest HRCT. In 21 cases, we had to resort to a histological study to achieve greater diagnostic certainty. The presence of nodules characteristic of silicosis was observed in 17 (81%), granulomas coexisted in the parenchyma and lymph nodes in 3 patients, and 3 cases showed an interstitial pattern with characteristics highly suggestive of usual interstitial pneumonia.
Chest X-ray Readings According to ILO 2011 Classification.
| Shape and Size of Small Opacities | No. (%) |
|---|---|
| Round | 93 (96.9) |
| p, p-q | 45 (48.4), 12 (12.9) |
| q, q-r | 26 (28.0), 7 (7.5) |
| r | 3 (3.2) |
| Irregular s/t | 7 (7.3) |
| Category of profusion of small opacities | |
| 1 | 53 (55.2) |
| 2 | 41 (42.7) |
| 3 | 2 (2.1) |
| Progressive massive fibrosis masses | |
| No | 77 (80.2) |
| A | 15 (15.6) |
| B | 4 (4.2) |
No.: total number of cases; %: percentage of the total.
High Resolution Computed Tomography Readings.
| Variable | |
|---|---|
| Shape and Size of Small Opacities | No. (%) |
| Round | 96 (100) |
| p, p-q | 34 (35.4), 14 (14.6) |
| q, q-r | 34 (35.4), 5 (5.2) |
| r | 2 (2.1) |
| Irregular s/t | 7 (7.3) |
| Grade of profusion of small opacitiesa | |
| Round | 9 (6–12) |
| Irregular | 9 (6–11) |
| Ground glass patternb | 29 (30.2)5.1 (3–6) |
| Emphysemab | 16 (16.7)3.8 (3–4) |
| Large opacities | |
| No | 54 (56.3) |
| A | 27 (28.1) |
| B | 14 (14.6) |
| C | 1 (1) |
| Lymphadenopathies | 88 (91.7) |
| Subpleural nodules | 75 (78.1) |
No.: total number of cases; %: percentage of the total.
This study analyzes the largest sample of patients with silicosis in AQC workers collected to date, and provides a more accurate overview of the characteristics of this disease, while increasing the visibility of this important occupational health problem. Overall, this type of silicosis affects a large number of very young, fully employed workers, with few symptoms but in advanced disease stages. The work environment, revolving around small businesses where these conglomerates and other types of material with crystalline silica content are handled with scant protection measures, and the wide geographic dispersion of this model throughout Spain, ring a warning bell about the significance of this new presentation of silicosis.
Implementation of the “Global Program for the Elimination of Silicosis” of the International Labor Organization and the World Health Organization led to the launch of prevention and control programs in different countries, which resulted in a reduction in the incidence of silicosis among workers in the more traditional sectors of silica exposure.19 No national registry is kept on this disease in Spain, but the Observatory of Occupational Diseases set up by the Social Security Department found that as of 2010 the number of annual cases of pneumoconiosis caused by coal dust had fallen almost to the point of disappearing, while the incidence of silicosis lies at between 79 and 118 cases annually.20 These cases occur more frequently in Galicia, Castile-Leon, and Extremadura, reflecting the relationship of this disease with the granite and slate mining industries of these communities, while patients in this study are employed in a manufacturing sector (National Classification of Economic Activities C2370: Stone cutting, carving, and finishing) which has no specific geographic concentration (Table 1). Thus, just when silicosis was in a phase of rapid decline, these new agents have appeared, leading to the intense and aggressive resurgence of the disease worldwide.21,22
Since our first study was published in 2010,23 several authors in different countries have reported the presence of this new form of silicosis. Some of the most notable contributions were made by Kramer et al.21 in Israel, in a group of 25 workers handling crystalline silica conglomerates who had been referred for assessment for lung transplantation. These patients had significant lung function involvement compared to our series, although only 2 had complicated silicosis. The same authors24 subsequently analyzed the effect of exposure to AQC, studying functional and inflammatory parameters in a group of 68 exposed workers compared to an unexposed control group. They noted the existence of a large number of neutrophils in induced sputum and a slight decrease in lung function among exposed individuals, providing evidence of underlying inflammation in the bronchial and alveolar regions. In Australia, Hoy et al.25 have also drawn attention to this entity in a group of 7 workers who handled these high crystalline silica content materials without protection, and in whom silicosis and a greater annual lung function decline was observed. In Italy, Paolucci et al.10 also published 3 cases with similar characteristics. Interestingly, there were no related cases reported among 161 patients diagnosed with silicosis between the 2000 and 2017 in the United Kingdom.26 Our workers handle quartz conglomerates concurrently with other stones, which may explain the failure to identify ACQ as the causative agent in the recent publication of 6 cases of silicosis in young stonemasons in Edinburgh.27
These conglomerates are composed of quartz sand, and in some cases incorporate cristobalite, in granule sizes always less than 4.5μ, cemented together with other components (glass, feldspar, dyes, etc.), using polyester or acrylic resins as a binding agent to achieve a solid, resistant product. The crystalline silica content of this type of “synthetic stone” can vary between 70% and 90%, depending on the color and type of finish, but it always contains high concentrations of SiO2, which releases very high amounts of respirable aerosol during cutting, which penetrate the pulmonary territory.
The absence of symptoms in most patients, even in cases of complicated silicosis, calls for the implementation of strict health surveillance programs in these workers and the introduction of specific initiatives, such as the Comprehensive Silicosis Program of Andalusia.28
Lung function in simple silicosis has been widely studied and the degree of impairment is generally low. There is general agreement on the existence of confounding factors associated with smoking and a slight predominance of obstructive bronchial disease, mainly emphysema. Gamble et al.,29 in a wide-ranging review, described a slight reduction in spirometric values and CO transfer associated with smoking and lack of physical fitness of patients, especially in the early stages of the disease. Lung function variables (forced vital capacity, forced expiratory volume in 1 second, diffusing capacity of the lung for CO) show more impairment in more advanced stages of the disease. Blanco Pérez et al.30 analyzed the exercise capacity of a group of patients with complicated silicosis using the 6-minute walk test, and found that it was useful for predicting hospitalization and mortality. Ophir et al.24 found moderate impairment and a statistically significant relationship between functional loss and the quantity of particles smaller than 5μ inhaled by workers, although they compared exposure histories without controlling for the presence of silicosis. In our cases, spirometric values, static volumes, and diffusion were preserved, and we were unable to detect any deterioration attributable to silicosis. Tobacco consumption among these workers is similar to that of the general population.31
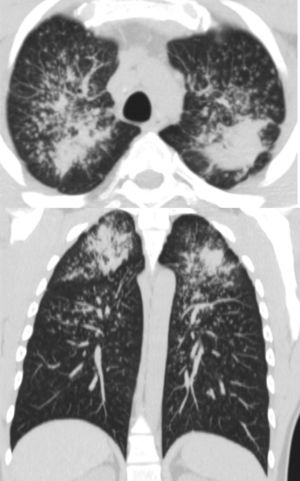
Chest HRCT is well known to increase sensitivity in the detection of progressive massive fibrosis (PMF).32 Nodular pattern findings, subpleural involvement and lymphadenopathies are similar to those of classic silicosis,33 although the presence of ground glass patterns of moderate extension in 30% of patients in our series should be noted, in addition to the existence of the usual nodules (Fig. 1). Several of the cases described by the Australian and Italian authors10,23 were significant for the presence of lymphocytosis in bronchoalveolar lavage, findings not described in classic silicosis. All this suggests a different form of the disease, probably more disseminated and aggressive than usual, which can develop more rapidly to an irreversible, fibrosing process. In our series, 10 patients met the criteria for accelerated silicosis.34 This group is too small to draw meaningful conclusions, but a profile is emerging of young people employed in cutting and polishing stone with increased use of conglomerates, who develop PMF (Fig. 2) and a tendency to lower lung function values. The histological and mineralogical study of samples obtained by transbronchial cryobiopsy35 helped exclude sarcoidosis in young people who showed a short latency period from the start of exposure (Fig. 3), and in other cases it revealed patterns of usual interstitial pneumonia associated with the deposit of silica particles (Fig. 4),36,37 which introduces therapeutic prospects not yet addressed in this disease.38
In conclusion, our study reports the presence of significantly severe silicosis in considerable numbers of young workers employed in small-to-medium sized businesses involved in the construction and modification of interiors (bathrooms, kitchens, etc.), which use these quartz conglomerates in unsafe working conditions without the appropriate protection measures. Moreover, silica dust has recently been classified as carcinogenic to humans,39,40 underlining the need to pay even greater attention to its potential pathogenicity. This new evidence requires us to update our knowledge, to broaden our respiratory medicine programs, and to increase surveillance in this type of occupational activity.
FundingThis study was funded by Roche-Farma, S.A., Spain, through the Integrated Research Agenda of the Spanish Society of Pulmonary and Thoracic Surgery (SEPAR) in Diffuse Interstitial Lung Diseases.
Conflict of InterestsThe authors state that they have no conflict of interests.
Please cite this article as: Martínez González C, Prieto González A, García Alfonso L, Fernández Fernández L, Moreda Bernardo A, Fernández Álvarez R, et al. Silicosis en trabajadores con conglomerados artificiales de cuarzo. Arch Bronconeumol. 2019;55:459–464.