A rare complication of community-acquired pneumonia (CAP) is septic arthritis (SA). This infection is exceptional, and does not usually occur simultaneously with the acute process.1,2 It is most commonly caused by Streptococcus pneumoniae.1,3 The joints most often affected in these cases are the knee, the hip and the shoulder.1,3 Most SA are caused by Staphylococcus aureus and Streptococcus, and develop in patients with predisposing risk factors.1–6 We report a case of pneumonia due to S. aureus, accompanied simultaneously with a sternoclavicular septic arthritis (SSA) due to bacteremia in a young woman without known risk factors. This is the first report of this association in the literature.
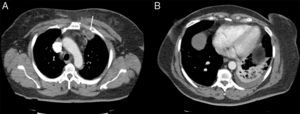
A 60-year-old woman, non-smoker, with no history of immunosuppression or risk factors for lung disease attended the emergency room with pleuritic pain and pain in the left shoulder, 38°C fever, cough without expectoration and intense pain in the mid-clavicular region and left shoulder. Chest radiograph revealed mild infiltrate in the left lower lobe. Signs of consolidation and egophony in the left lower field were detected on examination. A very painful non-fluctuating swelling with no signs of inflammation in the skin was observed in the upper left sternoclavicular region. Fiberoptic bronchoscopy was performed, revealing signs of inflammation, and samples were sent for pathology and microbiology studies. Blood cultures were negative. No valvular lesions or vegetations suggestive of endocarditis were observed on echocardiogram. Empirical treatment with ceftriaxone and levofloxacin was started, with little clinical response, while morphine was required for pain control. Chest computed tomography (CT) showed inflammatory changes in the left pectoral muscle and a pseudonodular image measuring 3.3×2.3cm in the space between the anterior portion of the first and second left costal arch, and pulmonary consolidation with pleural effusion in the left lower lobe (Fig. 1). Findings were confirmed on both ultrasonography of the neck and bone scintigraphy. Ultrasound-guided fine needle aspiration and biopsy was performed, from which S. aureus was isolated. The strain was resistant to ampicillin, and susceptible to erythromycin, gentamicin, clindamycin, ciprofloxacin, levofloxacin, and cotrimoxazole. The same microorganism was isolated from the bronchoscopy samples. During admission, intravenous ciprofloxacin and amoxicillin–clavulanic acid were administered, in line with susceptibility results, and improvement was observed in clinical symptoms, radiological signs, and acute phase reactants. Drainage was not required. Treatment continued on an outpatient basis for another 40 days, with complete resolution of the syndrome.
SSA is exceptional and accounts for only 1%–9%2,4 of SA, and generally occurs in patients with debilitating risk factors and immunosuppression.1–6 It is also unusual to see the simultaneous development of SA in the acute period of an episode of pneumonia, as it tends to occur later.1,2 In our patient, the SSA was attributed to the bacteremic pneumonia, as the same microorganism was isolated. S. aureus pneumonia in a patient without risk factors is in itself exceptional. The clinical picture of SSA, in contrast to our case, is generally insidious, and presents with fever, pain in the shoulder, and edema and erythema in the sternoclavicular joint.1,2,4–6 The most widely used diagnostic test is ultrasound, although CT can identify the degree of bone destruction, and scintigraphy is used to delimit the inflammatory area and guide the biopsy and aspiration procedure. The definitive diagnosis depends on isolation of the microorganism. This will indicate the appropriate antibiotic therapy, which should continue for at least 4 weeks in the absence of complications.1–3,5,6 Surgical treatment is recommended in case of extensive osteomyelitis, abscesses, empyema, or mediastinitis.1,4,5 In conclusion, pneumonia can unusually cause SA, and exceptionally SAA, and these entities may go unnoticed in the clinical context. As this process is potentially disabling and possibly fatal, etiologic diagnosis should not be delayed.
Please cite this article as: Molina V, Arlandis M, Vañes S, Chiner E. Neumonía por S. aureus y artritis séptica esternoclavicular, una complicación insólita. Arch Bronconeumol. 2018;54:168–169.