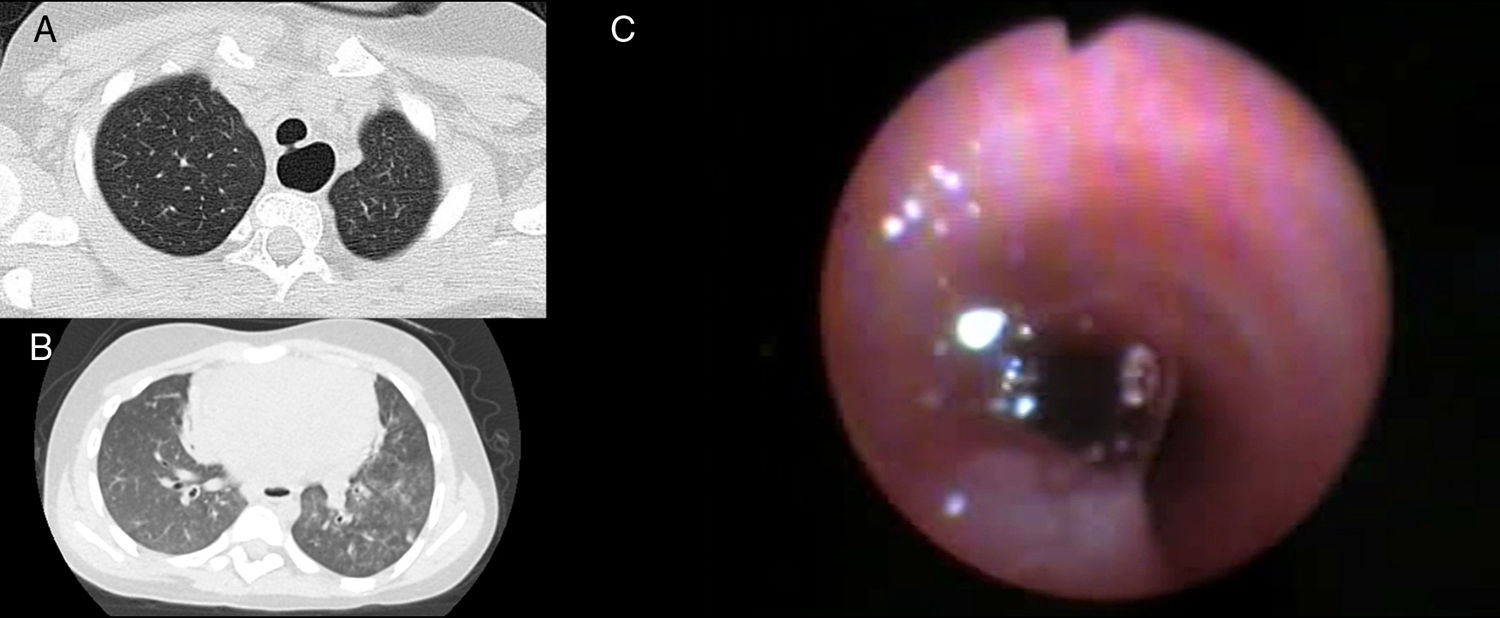
A 7-year-old patient with a history of dorsal hemivertebra, pes plano valgus, and bronchial hyperreactivity was referred for recurrent pneumonias in different sites from the age of 2. During the visit, she reported dysphagia to liquids and was febrile with subcrepitant rales in the left lung base. Neonatal screening for metabolic diseases, an immunity study, and α-1-antitrypsin levels were normal. HRCT revealed a continuity defect of the tracheal pars membranacea (Fig. 1A) and central acinar opacities consistent with microaspirations (Fig. 1B). On fiberoptic bronchoscopy, the patency of the tracheoesophageal fistula (TEF) was confirmed by bubbling and passage of methylene blue, instilled through the esophagus, into the trachea (Fig. 1C). Multiple minor bronchial abnormalities and 70% lipid-laden macrophages were detected in bronchoalveolar lavage. Surgical closure was performed by right cervicotomy with a good outcome.
TEF and esophageal atresia are the most common congenital abnormalities of the esophagus. H-type TEF is the least common (4%).1 Presentation outside the postnatal period consists of recurrent pneumonias in different sites.2 Treatment is surgical, depending on the location. The presence of TEF with dorsal hemivertebra and pes plano valgus may correspond to a mild variant of VACTERL association.
Please cite this article as: Piolatti-Luna A, Castillo-Corrullón S. Neumonías aspirativas de repetición en una niña de 7 años con fístula traqueoesofágica congénita no diagnosticada. Arch Bronconeumol. 2021;57:545.