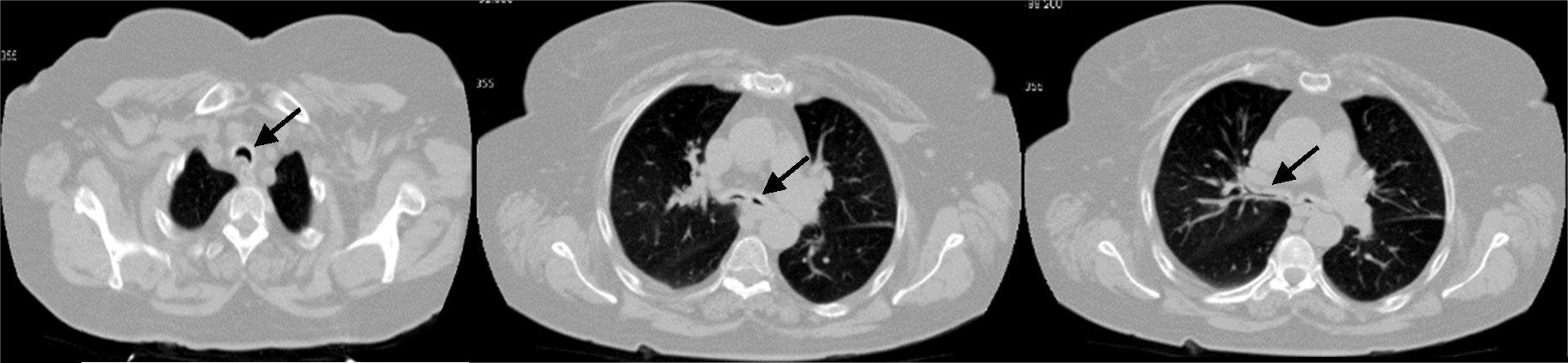
A 68-year-old female with a diagnosis of childhood asthma, was referred to the pulmonologist for recurrent episodes of acute severe dyspnoea and wheezing for the last three years. These were treated as asthma, with inhaled bronchodilators and corticosteroids, but without significant clinical improvement. She performed lung function tests, which showed a moderate bronchial obstruction, with limited response to bronchodilation. Chest CT revealed tracheal and bronchial wall thickening and luminal narrowing (Fig. 1). This tracheobronchial stenosis was also observed in bronchoscopy. In the subsequent year of follow up, she developed red eye episodes, polyarthritis, recurrent ear pain and saddle nose deformity. Autoimmunity was negative, but sedimentation rate was elevated (26mm). Relapsing polychondritis was then diagnosed, according to the criteria developed by McAdams et al.1 The patient started treatment with oral corticosteroids and methotrexate, with good clinical response. No specific treatment for tracheobronchial stenosis has yet been required. We highlight the clinical challenge of this diagnosis, due to insidious manifestations of the disease, and raise awareness of tracheobronchial involvement in relapsing polychondritis, which in some cases can lead to critical airway stenosis.2
Journal Information
Vol. 53. Issue 8.
Pages 453 (August 2017)
Vol. 53. Issue 8.
Pages 453 (August 2017)
Clinical Image
Full text access
Relapsing Polychondritis With Airway Involvement: A Clinical Challenge
Policondritis recidivante y compromiso de las vías aéreas: un desafío diagnóstico
Visits
6366
Marta Sousa
, João Silva, Bárbara Rodrigues
Corresponding author
Centro Hospitalar Tondela-Viseu, Viseu, Portugal
Article information
Full Text
References
[1]
L.P. McAdam, M.A. O’Hanlan, R. Bluestone, C.M. Pearson.
Relapsing polychondritis: prospective study of 23 patients and a review of the literature.
Medicine (Baltimore), 55 (1976), pp. 193-215
[2]
C. Gorard, S. Kadri.
Critical airway involvement in relapsing polychondritis.
BMJ Case Rep, (2014), pp. 2014
Copyright © 2017. SEPAR