At the onset of the COVID-19 pandemic, there was uncertainty about its impact on chronic respiratory patients. The known role of viruses in the exacerbations of diseases such as asthma or COPD and the difficulties associated with the clinical care of these diseases led to fears of an increase in admissions and exacerbation events. This situation forced a reorganization of healthcare for patients with long-term conditions.1 However, it soon became apparent that patients with asthma were not overrepresented in COVID-19 admissions, while patients with COPD had only a slightly increased risk of COVID-19-related admission.2,3 Furthermore, and unexpectedly, several reports suggested that a reduction in the exacerbations of both asthma and COPD occurred during the coronavirus pandemic.4–6 In patients with asthma there was a significant reduction in admissions for exacerbations during the pandemic, across all age groups, and different countries.7–9 In patients with COPD, a systematic review and meta-analysis5 concluded that the pooled rate ratio of hospital admissions for exacerbations during the pandemic period was 0.50 (95% CI 0.44–0.57).
To understand the pandemic's true impact on hospitalizations in Spain, we studied admissions for asthma and COPD in 2020, the first year of the COVID-19 pandemic. Admissions from each autonomous region were collected and compared with admissions for the same diseases in previous years.
We performed a retrospective, observational, ecological study using the Spanish National Hospital Discharge Database (Conjunto Mínimo Básico de Datos – CMBD–), which compiles public and private hospital data and covers almost 100% of admissions in Spain (https://www.sanidad.gob.es/estadEstudios/estadisticas/cmbd.htm; accessed 20.1.23). We analyzed data collected between 1 January 2016 and 31 December 2020 for subjects aged 15 and above in 17 autonomous regions and two autonomous cities (Table 1). Data on the Spanish population in this age group for each year of the study were obtained from the National Institute of Statistics (https://www.ine.es/index.htm).
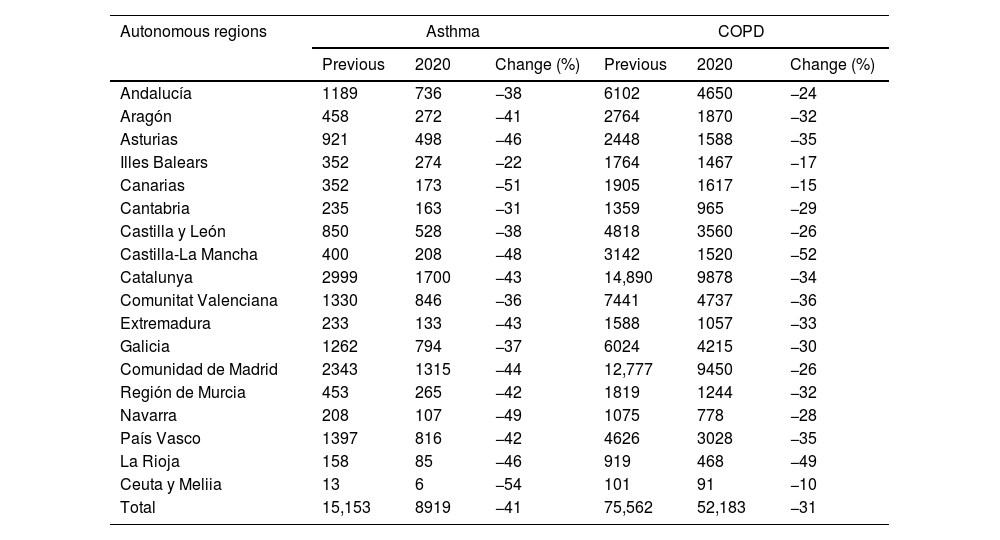
Comparison of hospital admission during 2016–2019 and 2020.
| Autonomous regions | Asthma | COPD | ||||
|---|---|---|---|---|---|---|
| Previous | 2020 | Change (%) | Previous | 2020 | Change (%) | |
| Andalucía | 1189 | 736 | −38 | 6102 | 4650 | −24 |
| Aragón | 458 | 272 | −41 | 2764 | 1870 | −32 |
| Asturias | 921 | 498 | −46 | 2448 | 1588 | −35 |
| Illes Balears | 352 | 274 | −22 | 1764 | 1467 | −17 |
| Canarias | 352 | 173 | −51 | 1905 | 1617 | −15 |
| Cantabria | 235 | 163 | −31 | 1359 | 965 | −29 |
| Castilla y León | 850 | 528 | −38 | 4818 | 3560 | −26 |
| Castilla-La Mancha | 400 | 208 | −48 | 3142 | 1520 | −52 |
| Catalunya | 2999 | 1700 | −43 | 14,890 | 9878 | −34 |
| Comunitat Valenciana | 1330 | 846 | −36 | 7441 | 4737 | −36 |
| Extremadura | 233 | 133 | −43 | 1588 | 1057 | −33 |
| Galicia | 1262 | 794 | −37 | 6024 | 4215 | −30 |
| Comunidad de Madrid | 2343 | 1315 | −44 | 12,777 | 9450 | −26 |
| Región de Murcia | 453 | 265 | −42 | 1819 | 1244 | −32 |
| Navarra | 208 | 107 | −49 | 1075 | 778 | −28 |
| País Vasco | 1397 | 816 | −42 | 4626 | 3028 | −35 |
| La Rioja | 158 | 85 | −46 | 919 | 468 | −49 |
| Ceuta y Meliia | 13 | 6 | −54 | 101 | 91 | −10 |
| Total | 15,153 | 8919 | −41 | 75,562 | 52,183 | −31 |
Number of admissions (previous: mean 2016–2019).
Cases were defined as hospital discharges where the main diagnosis was asthma or COPD according to the International Classification of Diseases (CIE-10-ES), which was used in the Spanish CMBD during the period analyzed. The study was approved by the local ethics committee. It was not necessary to obtain informed consent in accordance with Spanish legislation.
The rate of hospital admissions (per 100,000 inhabitants) for asthma and COPD in Spain between 2016 and 2020 was determined. The average number of admissions for each disease between 2016 and 2019 (4 years prior to the pandemic) was established and compared with the number of admissions in 2020.
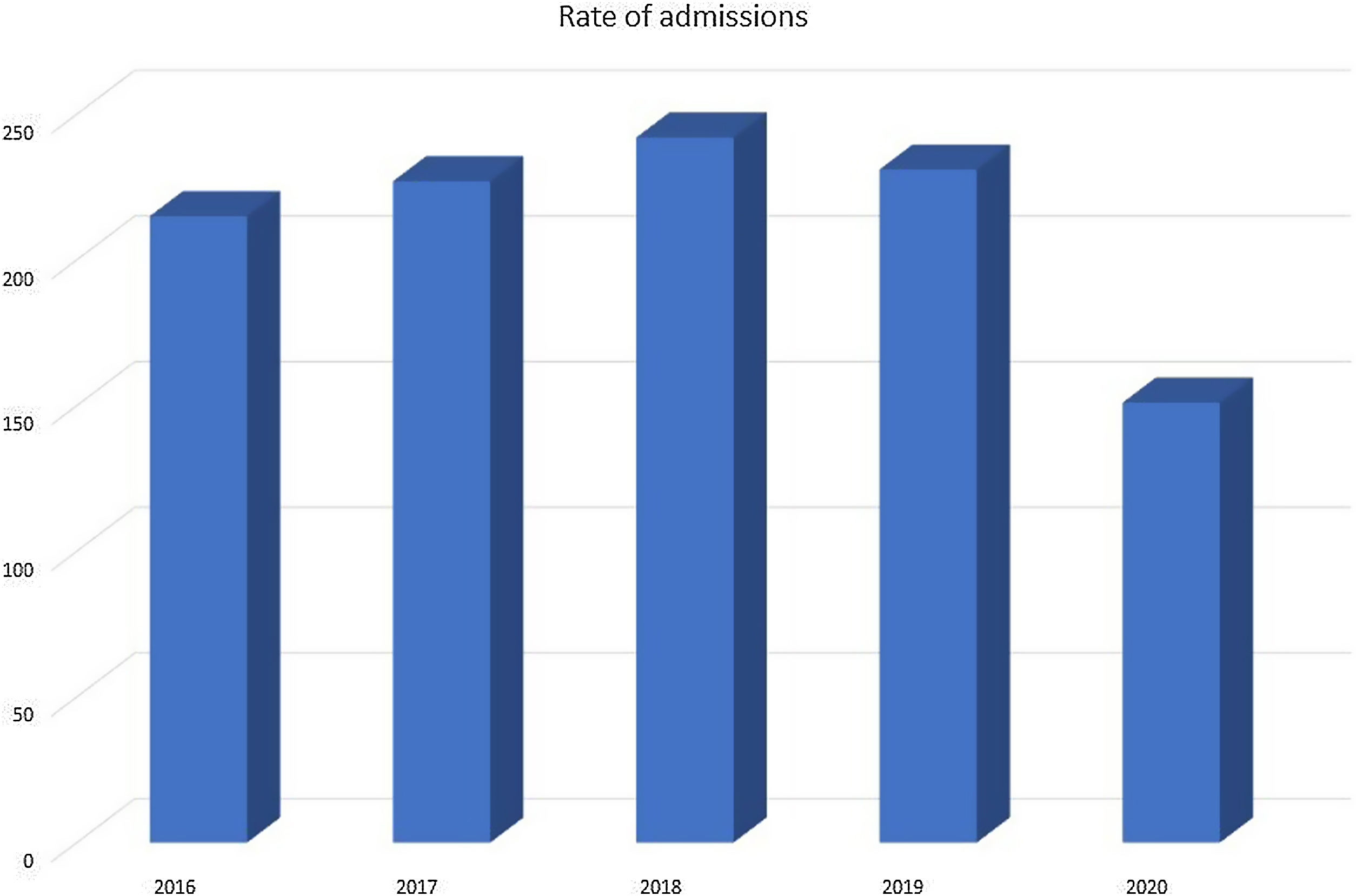
Fig. 1 shows the rates of hospital admissions per 100,000 inhabitants each year. In the years prior to the pandemic, this rate ranged between 215 and 242; in 2020, the rate dropped to 151. As detailed in Table 1, there was an average decrease of 41% in admissions for asthma and 31% in admissions due to COPD. In 2020 there was a 33% decrease in the absolute numbers of hospitalizations (n=29,613), with 6234 asthma-related admissions and 23,379 COPD-related admissions. This decrease was observed in all autonomous regions for both diseases, albeit with some differences that could be explained by the smaller populations in some of the regions, different disease prevalence or different health care characteristics.
Our study describes, for the first time, the significant impact of the onset of the COVID-19 pandemic on the reduction in asthma and COPD-related hospital admissions in Spain using complete nationwide data. It is important to note that the data analyzed in this study were for each full year and, therefore, include the months immediately prior to the pandemic. For this reason, the effect of the pandemic on the decline in hospital admissions is probably greater than reported in this study.
Other studies that analyzed large territories or national data from other countries across different periods have described similar findings. During the beginning of the pandemic there was a 45% relative reduction in COPD exacerbations in Denmark,10 43% in Slovenia,11 and 44% in Hong Kong (in the first three months of 2020).12 In the pandemic year, the decrease in admissions occurred across different degrees of disease severity, and the usual seasonal increase in COPD exacerbations and mortality did not occur.11
A decrease in asthma exacerbations following the onset of the pandemic was reported in patients with asthma in countries such as Denmark and the United Kingdom.7–9 Importantly, SARS-CoV2 infections in patients with asthma did not exacerbate the disease.13 In data from England, there was a decrease in asthma exacerbations in all quarters of 2020 (except the first) and 2021, between 39.7% and 63.2%.14 Similar reductions were observed in other nations of Great Britain during lockdowns.15
In addition to respiratory diseases, there was a notable decrease in admissions for other diseases. In Great Britain, a 34.2% decrease in admissions for illnesses other than COVID-19 (oncologic, cardiovascular, and respiratory processes) was reported, and this decrease was not limited to the first months of the pandemic.16
At the beginning of the pandemic. it was assumed that patients did not go to the hospital due to fear of contracting COVID-19.17 However, although lockdowns were associated with substantial reductions in both asthma and COPD admissions, no increase in mortality for these diseases was observed, as would be expected if patients had avoided hospitals due to this fear.15,18 In our previously reported experience analyzing COPD patients with multiple exacerbations, these patients did not avoid clinical care during the pandemic when they experienced symptoms.4 Furthermore, it is difficult to assume that patients with severe exacerbations of asthma or COPD are willing or able to engage in healthcare avoidance. Therefore, the reduction in hospital admissions is unlikely to be adequately explained by changes in health-seeking behavior or pandemic-related healthcare service disruption.14
Public health measures implemented during the COVID-19 pandemic involved social isolation and the use of face masks. These measures may have contributed to the reduction of circulating seasonal viruses. In addition, transport restrictions led to lower pollutant levels. Multiple studies have shown associations between high levels of air pollution and asthma exacerbations.19 There is now data that confirm the association between improved air pollution and reduced asthma exacerbations during the pandemic. Levels of NO2, which vehicular emissions are the primary source of, were significantly correlated with asthma admissions during the pandemic period.20 The decrease in hospital admissions could be attributed to a combination of factors, lower virus transmission, less exposure to environmental contamination, confinement with less physical activity, and potentially improved treatment adherence.4,18
Our findings aid in improving the understanding of the impact of the COVID-19 pandemic on obstructive pulmonary diseases. The number of hospital admissions for chronic obstructive respiratory diseases decreased by one-third during 2020. Although this occurred in the context of a global pandemic associated with serious health consequences, it may be possible to draw positive conclusions regarding the protection of these patients in non-pandemic periods. These patients should avoid contact with family members or other persons with suspicion of contagious diseases and the use of masks in certain circumstances. Furthermore, improving air quality to prevent exacerbations of asthma and COPD should be prioritized.
Author's contributionsMGN: Methodology, Formal analysis, Writing-review and editing.
EGP: Conceptualization, Methodology, Data curation, Formal analysis, Writing -original draft.
All authors have read and provided intellectual input to the manuscript.
All authors have approved the final version of the manuscript and take public responsibility of its content.
Ethical approvalThe study was approved by the local ethics committee.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestsThe authors state that they have no conflict of interests.