Systemic arterialization of the lung without pulmonary sequestration is a rare congenital condition characterized by the presence of an aberrant arterial branch originated from the aorta. This artery supplies a lung with normal parenchyma and bronchial anatomy. Clinically, haemoptysis represents the main clinical manifestation. Few cases have been reported so far and therapeutic management is not standardized. Embolization is a non-invasive treatment with increasing indications.
A thirty-year-old woman was referred to our centre after two episodes of haemoptysis. She was allergic to penicillin with unremarkable comorbidities. No prior treatment except oral contraception. No other bleedings or haemostatic dyscrasias were documented.
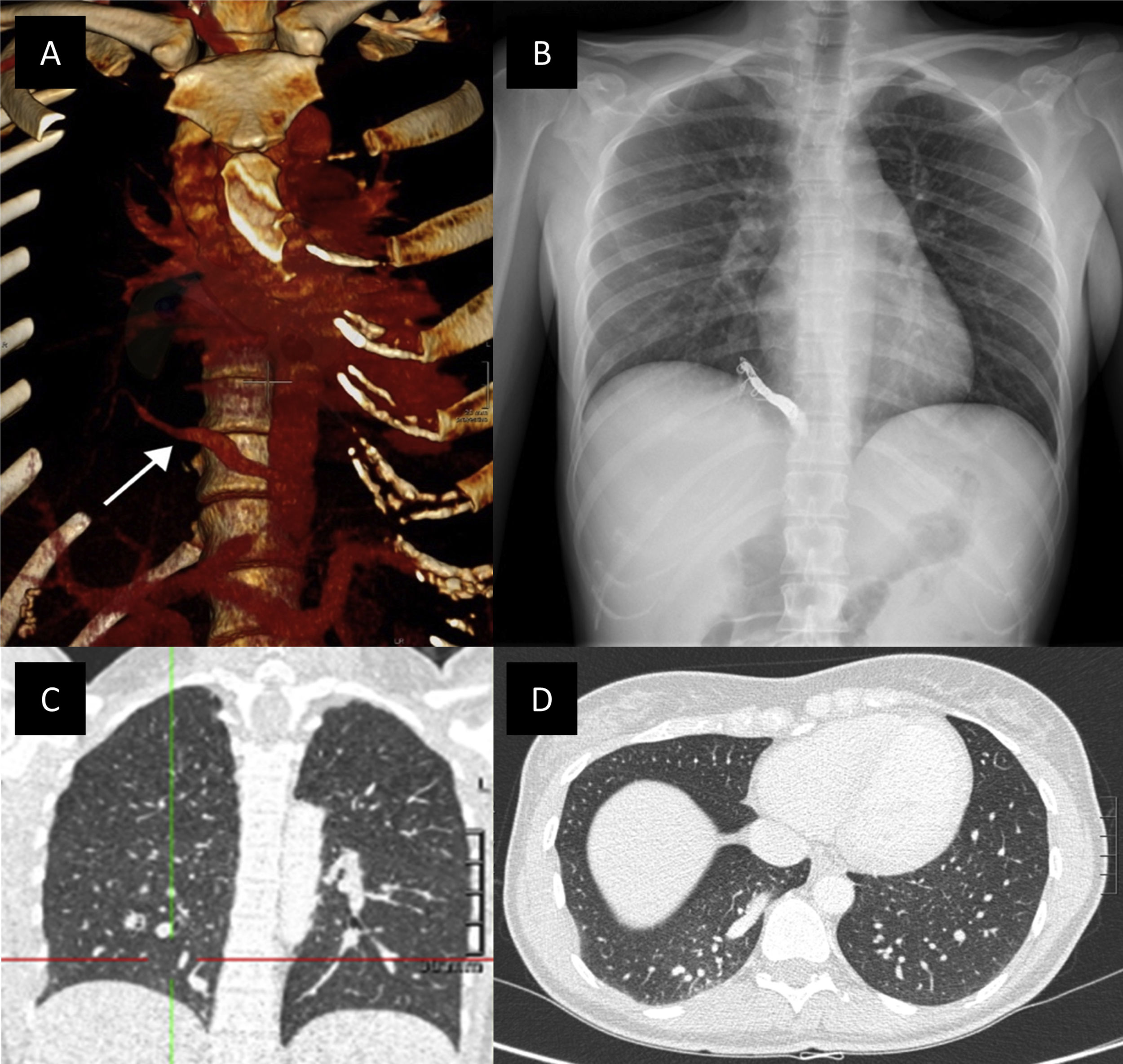
The first episode happened one year prior with limited symptoms after conservative treatment in another institution. Chest X-ray, blood and functional lung tests were unremarkable. Eventually, a thoracic computed tomography (CT) angiography showed an anomalous systemic artery arising from the abdominal aorta (Fig. 1A). The artery irrigated the posterior-basal segment of right lower lobe (RLL) with no other alterations in pulmonary parenchyma. Pulmonary and cardiac shunts were ruled out.
(A) Reconstruction of thoracic CT. Anomalous systemic artery arising from the abdominal aorta (white arrow). (B) 3-Month-follow-up with chest X-ray show the coils in the anomalous artery in the RLL. (C and D) Anomalous systemic artery arising from the abdominal aorta supplying a normal lung parenchyma.
Treatment by endovascular approach was decided after a multidisciplinary approach with pulmonologists, thoracic and vascular surgeons, and interventional radiologists. The arteriography confirmed the previous findings and normal venous drainage. Finally, endovascular embolization of the anomalous artery was performed using coils and Glubran® with no immediate complications.
Soon after the procedure, the patient presented fever and pleuritic pain due to a mild right pleural effusion and a small area of pulmonary infarct, managed with conventional analgesia. A 3-month-follow-up CT-angiography (Fig. 1B and C) showed the coils in the anomalous occluded artery with no other remarkable findings. The patient currently remains asymptomatic.
Pulmonary sequestration represents a mass of abnormal, not functional pulmonary tissue supplied by an anomalous systemic artery. Its main feature is its independence from the tracheobronchial tree.1 The term “sequestration” was introduced by Pryce2 to describe congenital abnormalities characterized by anomalous systemic arterial supply to the lung, related with atresia or hypoplasia of the pulmonary artery. Since then, the spectrum of bronchopulmonary vascular malformations has grown widely, especially with the “sequestration spectrum” concept, in order to include malformations that do not fulfil the original sequestration definition.1 Additionally, the term “pulmonary malinosculation” gathered all congenital lung abnormalities with anomalous communication between blood vessels or other tubular structures.3
The presence of normal lung parenchyma and bronchial supply is the main difference between systemic arterialization of the lung without pulmonary sequestration and true sequestration.4 The former is rare, with few cases reported,4–6 and consists of an aberrant systemic arterial branch arising from the thoracic descending aorta or the abdominal or celiac axis. Usually, the artery coming from the abdominal aorta supplies the RLL, whereas the thoracic origin often supplies the left lower lobe,5 the most commonly involved segment.7
In our case, the anomalous artery supplied a non-sequestered region in the RLL without other congenital abnormalities. The aetiology of this condition is unknown. Persistence of an embryonic connection between the aorta and the pulmonary parenchyma remains the main hypothesis.8 Most patients are asymptomatic,9 although recurrent pulmonary infection and haemoptysis are possible clinical manifestations.5 One explanation for the intermittent haemoptysis, present in our case, is the alveolar haemorrhage secondary to the high vascular pressure in the abnormally perfused segments.6
The treatment is generally recommended even in asymptomatic patients in order to prevent possible fatal haemoptysis. The therapeutic approach is not fully standardized although the most widespread consensual treatment in sequestration currently is surgical resection.10 Surgical approach includes lobectomy, systemic artery-to-pulmonary artery anastomosis and endovascular occlusion of the aberrant systemic artery.11 Less invasive approach with embolization has also been described in few cases.6,11,12 Multiple substances may be used to perform embolization. We decided to use an embolic liquid agent combined with coils. The embolic liquid agent reduces the risk of rebleeding13,14 although distal embolization and tissue necrosis might be higher.15 Coils allow proximal occlusion and collateral flow. In our case, the calibre of the artery and the large irrigated territory may justify the lung infarction independently of the Glubran use. The patient presented a mild post-embolization syndrome (PES), the most common side effect of embolization. PES is characterized by fever, nausea and pain, usually within the first 72h after the procedure.
In conclusion, our case emphasizes the fact that the embolization is a safe and feasible alternative to surgery, proving to be a procedure with few complications and clinically successful. Further studies are now warranted to study the benefit over surgery in patients with anomalous vascularization of the lung.
Ethical statementThis work was conducted at Hospital de la Santa Creu i Sant Pau with approval from the ethic committee of our Hospital.
FundingNo funding was received for this research.
Conflicts of interestThe authors declare no conflicts of interest.