The bronchial involvement of diffuse large B-cell lymphoma (DLBCL) is an exceptional finding. Histological diagnosis is done with lung tissue samples. In these cases, the need for immunohistochemistry studies in order to establish the diagnosis requires obtaining tissue samples of adequate size and quality. Sometimes, endoscopic explorations may be repeated to obtain further biopsies.
We present the first documented case of recurrent endobronchial DLBCL that was diagnosed from a bronchial biopsy taken with a cryoprobe.
La localización endobronquial del linfoma difuso de células grandes tipo B (LDCGB) es infrecuente. El diagnóstico histológico se realiza mediante la obtención de muestras de tejido pulmonar. En estos casos, la necesidad de realizar estudios inmunohistoquímicos para establecer el diagnóstico requiere la obtención de muestras de un tamaño y calidad adecuados, lo que, en ocasiones, implica la repetición de la exploración endoscópica y la realización de biopsias adicionales.
Presentamos el primer caso de un paciente diagnosticado de recidiva de LDCGB endobronquial mediante biopsia bronquial realizada con criosonda.
Diffuse large B-cell lymphoma (DLBCL) is a histologically aggressive non-Hodgkin's lymphoma (NHL). Pulmonary localisation of these lymphomas is rare, and constitutes less than 1% of cases.1–3 Moreover, endobronchial involvement is an exceptional finding which, due to its therapeutic and prognostic implications, requires tissue samples to be obtained that are of sufficient quality and size to perform a complete histological and immunohistochemical study. We present the case of a patient with recurrent endobronchial DLBCL who, after having several bronchial biopsies with conventional biopsy forceps, was finally diagnosed by bronchial biopsy using a cryoprobe.
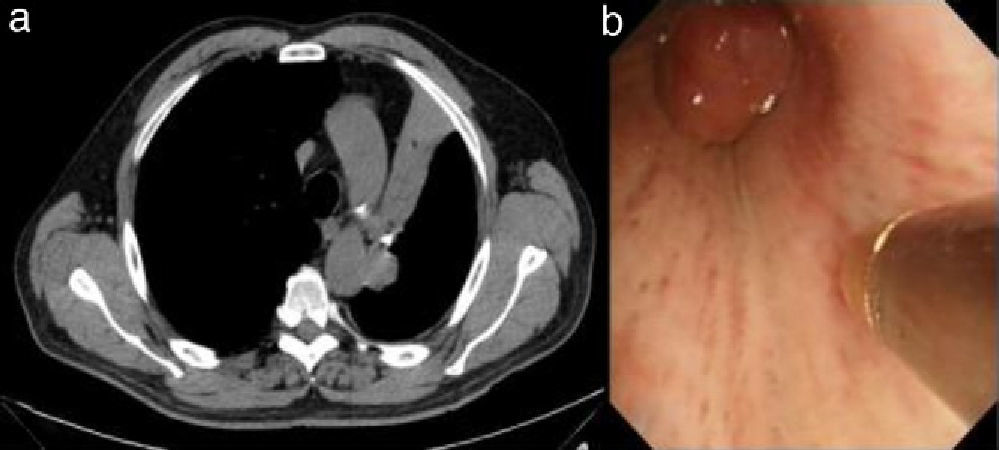
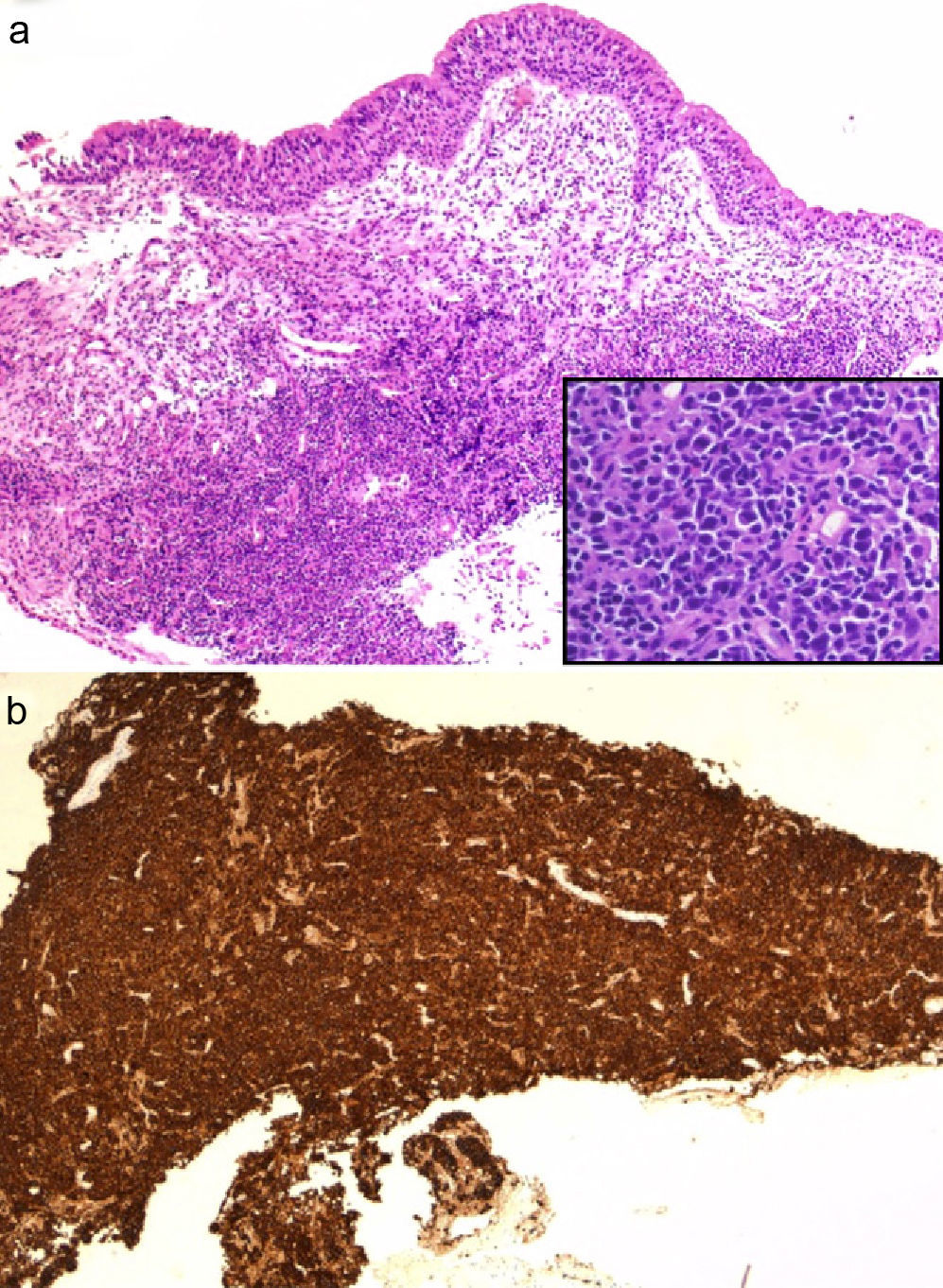
Clinical ObservationA 75-year-old male with a history of hypertension for which he was on medical treatment, allergic to iodinated contrast, presented in January 2004 with fever and abdominal pain. Physical examination revealed tenderness in the left hypochondrium. Computed tomography (CT) of the abdomen showed splenomegaly with multiple hypodense nodular lesions and infradiaphragmatic adenopathies in the mesenteric-celiac region and perivascular space of the abdominal aorta. A splenectomy was performed; spleen histology was indicative of DLBCL. The patient was treated with the immunochemotherapy regimen R-CHOP (rituximab, cyclophosphamide, adriamycin, vincristine and prednisone), achieving complete response. In June 2010, he presented with left pleuritic pain and moderate-effort dyspnoea. Physical examination revealed hypophonesis in the left pulmonary field. A chest CT scan was performed, showing stenosis of the left main bronchus and ipsilateral hilar adenopathies leading to left upper lobe collapse (Fig. 1a). Due to a suspected lung neoplasm, bronchoscopy was performed, which showed the presence of an endobronchial mass with a smooth surface obstructing the entry to the left upper lobe. Bronchial biopsy was carried out, but the material obtained was insufficient to establish a definitive diagnosis. A second biopsy obtained material that was suspicious for malignant cells but the sample size did not enable immunohistochemical techniques to be applied; it was therefore decided to perform a bronchial biopsy using a cryoprobe (Fig. 1b), obtaining a larger fresh sample of the lesion. Histological examination showed diffuse infiltration of the corium by a lymphoid proliferation of large atypical cells with numerous mitoses, with no infiltration of the bronchial epithelium (Fig. 2a). Immunohistochemical techniques showed a CD20-positive neoplastic cell population (Fig. 2b), with co-expression of bcl-6 and CD10, and a proliferative index (ki-67) of 70%. In accordance with these findings, the patient was diagnosed with recurrent DLBCL. Second line treatment was initiated with R-ESHAP (rituximab, etoposide, methylprednisolone, cisplatin and cytarabine), achieving a second complete remission. The patient is currently awaiting an autologous haematopoietic stem cell transplant.
The term non-Hodgkin's lymphoma (NHL) describes various neoplasms of lymphoid origin that constitute a heterogeneous group of diseases defined by morphological, immunophenotypic and genetic aspects. Primary pulmonary DLBCL represents 11%–19% of all primary pulmonary lymphomas4–6 and between 0.5% and 1% of malignant pulmonary neoplasms, although its incidence may be underdiagnosed due to its rapid spread to the mediastinum and extrathoracic sites.7 However, the incidence of recurrence in an endobronchial site in DLBCL is unknown.
The suspected diagnosis must be established in patients with a history of non-Hodgkin's lymphoma who present endobronchial masses and/or lobar or pulmonary atelectases on the chest X-ray or CT scan, and raises the differential diagnosis with lung neoplasia (mainly). Histological diagnosis is made by obtaining samples of lung tissue, either bronchial or transbronchial biopsies. However, on many occasions, given the high degree of cell atypia found, biopsies performed using conventional methods do not allow a definitive diagnosis to be established, and fresh biopsies of the area or from new sites must be carried out, as occurred in the case presented by Martínez et al.8 In this case report, we introduce a new method for performing bronchial biopsies using cryoprobes. Cryotherapy is traditionally a procedure applied in bronchoscopy; its main indication is the treatment and excision of endobronchial lesions, especially in cases of bronchial obstruction.9,10 The contact of the probe with the tissue has high freezing power which, due to the characteristics of the probe, is stable to traction. Previous studies which have evaluated the histological material from bronchial biopsies obtained by cryoprobes in cases of endobronchial tumours have found that the samples were larger than those taken with conventional forceps, and that they preserved the histology, enabling immunohistochemical techniques to be successfully applied.11,12 Similarly, our group has evaluated transbronchial pulmonary biopsies using this technique, obtaining tissue samples that were larger and of better quality than using conventional forceps.13
In the case presented, bronchial biopsies of the lesion were performed on two occasions using conventional forceps, but the samples obtained in both cases were insufficient to establish a specific histological diagnosis. Furthermore, this case involves several aspects that make it particularly interesting: from a diagnostic point of view, the low frequency of this disease and the rare presentation are noteworthy, as it is a recurrence of an endobronchial DLBCL in a patient previously diagnosed with extranodal DLBCL (splenic) and treated by chemotherapy and splenectomy with complete remission for years and, the diagnostic technique used to perform the histological study which enabled (as well as the application of immunohistochemical techniques) the integrity of the bronchial epithelium to be visualised (Fig. 2), ruling out other more common diagnoses such as mucosa-associated lymphoid tissue (MALT) lymphoma.
Thus, when the need arises to apply complex immunohistochemical methods for the diagnosis of endobronchial lesions, we should consider the use of other bronchoscopic techniques that enable tissue samples of better size and quality to be obtained in order to improve the diagnostic yield and avoid repetition of complementary examinations.
Please cite this article as: Pajares V, et al. Recidiva endobronquial de linfoma difuso de células grandes B. Diagnóstico con criosonda. Arch Bronconeumol. 2013;49:210–2.