Spirometry is a keystone in the diagnosis and follow-up of respiratory diseases, and must be used at all levels of healthcare.1 Nevertheless, one of the main drawbacks of this test is that results depend directly on the quality of the maneuver carried out by the patient and correct interpretation by the medical professional.
In the healthcare district of Lleida, a long-term effort has been made to provide spirometers and training to all primary care (PC) professionals.
We present the primary conclusions of a quality audit of spirometries performed in Lleida. The parameters of the maneuver and acceptability of the curves were evaluated using the Miller standardization as reference.2 Each parameter was scored as correct or incorrect by consensus of participants.
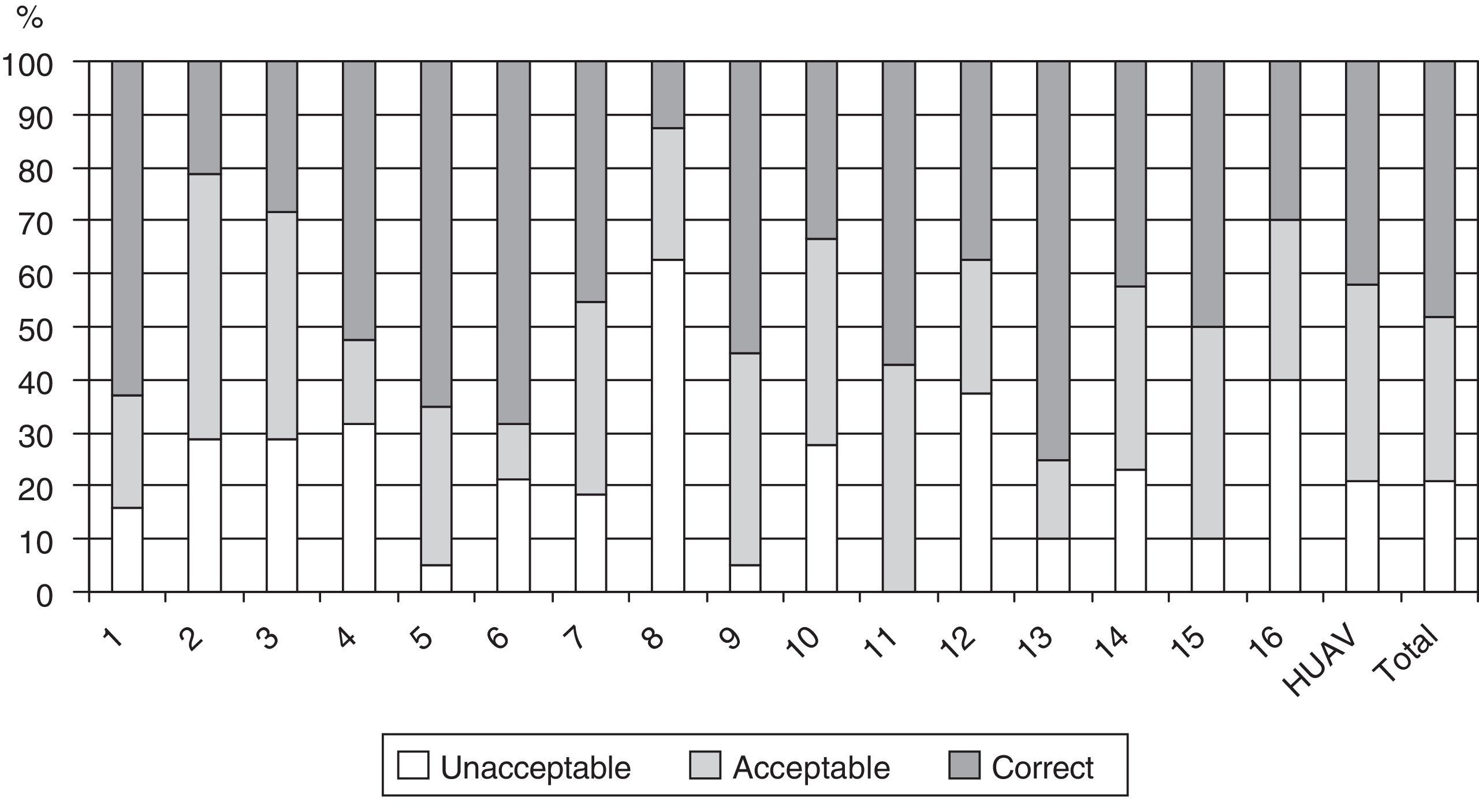
A total of 273 spirometries were included in the study (4.8% of all those performed in 2012) from 16 PC centers (73% of the primary healthcare areas in the province of Lleida). The mean age of patients undergoing spirometry was 57.1 years (SD: 16.3) and 172 (63%) were male. No statistical differences were observed in age or gender distribution between the centers. Bronchodilator testing was performed on 242 patients (88.6% of the study population). A total of 57 (20.9%) of the spirometries were classified as unacceptable, 84 (30.8%) were acceptable and 132 (48.4%) were correct. Accordingly, 216 (79%) were considered clinically acceptable/correct and 57 (20.9%) were not.
No significant differences were found between the proportion of acceptable/correct and unacceptable spirometries performed at the reference hospital and the PC centers overall. However, significant variability was found when individual centers were compared (unacceptability ranging from 5% to 62.5%) (Fig. 1).
A very high percentage of PC centers that had and used a spirometer took part in the study.3 However, these devices may be used less than that in other borderline areas, since the rate of spirometries/100 inhabitants/year in the Lleida healthcare region is 1.01, lower than the mean rate in Catalonia (1.32).4
The audit was performed by consensus of participants; therefore, the number of spirometries audited varied greatly and there may have been cases of interindividual variability that were not controlled, a factor that could limit extrapolation of the results of this study.
Further studies are needed with a sample size appropriate to the activity recorded and based on a design that allows any changes after intervention to be measured. Moreover, wide variability in quality was detected between the different PC centers, suggesting that individual improvements need to be made. A continuous coordinated effort is required to ensure that technical resources are used efficiently once all centers have been suitably equipped.
Conflict of InterestsThe authors declare that they have no conflict of interests.
Our thanks to Dr Joan Clotet, Dr Núria Nadal, Dr Araceli Fuentes, Dr M. Cruz Urgeles, Dr Iñigo Lorente and Dr Cristina Esquinas.
Please cite this article as: Lara B, Paredes E, Barbé F. Auditoría de calidad de las espirometrías realizadas en atención primaria de la región sanitaria de Lleida: Espir-Audit. Arch Bronconeumol. 2014;50:413–414.