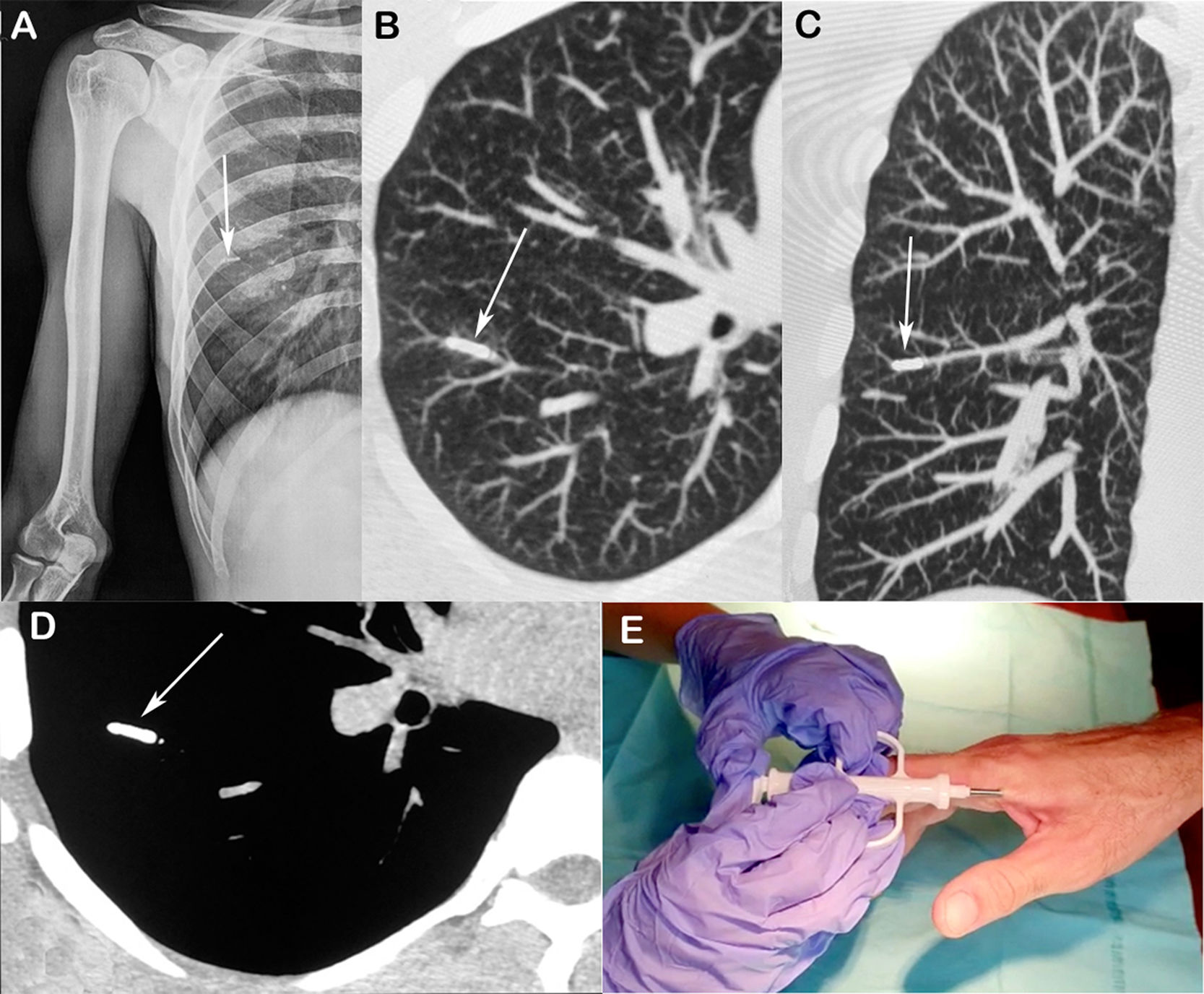
A 34-year-old man was referred to our department after a biochip implanted in his right hand stopped working. As he could not feel the device, the manufacturer instructed him to undergo simple radiography of the right upper limb. Radiographs revealed a small metallic foreign body in the right hemithorax. Chest CT showed the biochip lodged in a vascular branch of the right lower lobe of the lung (Fig. 1). The patient was diagnosed with pulmonary embolism caused by the migrated biochip. As he was asymptomatic and the device was located peripherally, no intervention other than periodic monitoring was recommended.
(A) Anteroposterior radiograph of the right humerus showing a small, dense linear projection in the right hemithorax (arrow). (B and C) Axial and coronal reconstructed images depicting the device lodged in a vascular branch of the right lower lobe of the lung (arrows). (D) Axial CT image (obtained with the mediastinal window setting) showing the small metallic device (arrow). (E) The biochip being implanted in the patient's hand.
Human biochips are small devices encased in glass, measuring approximately 12×1–2mm, covered by a material that prevents oxidation and, consequently, inflammation. The chip is usually implanted subdermally in the hand, injected under the skin using a hypodermic syringe, between the thumb and forefinger, an area with few nerve endings and blood vessels, considered practical and safe for this purpose. Although the literature on the subject is scarce, the probable mechanism of the embolism observed in our patient was the chip's inadvertent intravenous implantation. One possible way to avoid this complication would be the implantation being done by health professionals, such as doctors and nurses, or guided by ultrasonography.
Biochips use near-field communication (NFC), an emerging technology that is a subset of radiofrequency identification. NFC is short range and contactless; it is used for mobile phones and other devices, and permits the storage and updating of financial, medical, and demographic data. Potential medical applications include its use in glucose detectors, oxygen sensors, and blood pressure sensors.1,2 Clinicians should be aware of these small devices and include them among the causes of foreign-body pulmonary embolism.
Conflicts of interestThe authors declare that they have no conflicts of interest to express.