Pseudochylothorax is a very uncommon type of pleural effusion characterized by a high cholesterol content, and usually occurs in chronic effusions with pleural thickening.1 The most common causes are tuberculous effusion, sequelae from therapeutic pneumothorax, and rheumatoid pleurisy, although it has been seen in other clinical situations.1,2 While pleural effusion is a relatively common finding in rheumatoid arthritis, only around 20 cases of pseudochylothorax have been reported in these patients, so it is difficult to determine the real prevalence of this process.3
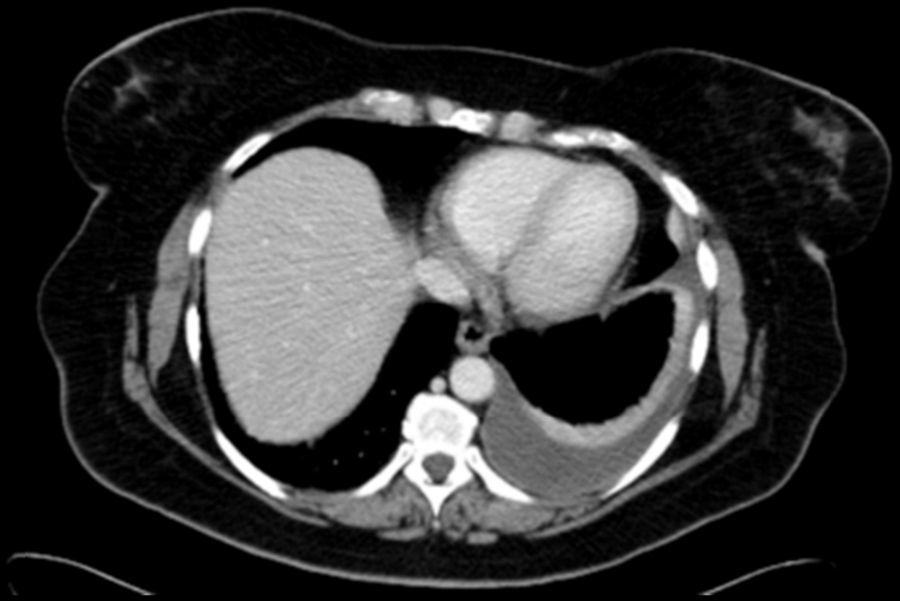
Cholesterol in the pleural space was thought to be due to erythrocyte and neutrophil degradation within a thickened pleura, but it seems more likely to originate from serum lipoproteins than from cell lysis.1 Pleural thickening with fibrotic scar tissue preventing fluid absorption was considered a key element in the etiopathogenesis of pseudochylothorax.1 However, in recent years, some cases of pseudochylothorax have been reported in patients with rheumatoid arthritis who have not shown pleural thickening, bringing the generally accepted pathogenic mechanism into question.4,5 We have diagnosed a new case of pseudochylothorax in a patient with rheumatoid arthritis who did not present pleural thickening. A 53-year-old woman, smoker (25 pack-years) with no previous respiratory symptoms, was referred to the respiratory medicine specialist after a small pleural effusion with no associated symptoms was detected on the study performed before an intervention for abdominal hernia. A chest radiograph obtained 7 months previously from the same patient did not show pleural effusion. She had been diagnosed with rheumatoid arthritis 2 years previously and was receiving treatment with corticosteroids, methotrexate and certolizumab. On chest CT (Fig. 1) pleural effusion was observed with no signs of pleural thickening. A thoracocentesis was performed, yielding a sterile, opalescent fluid with no malignant cells, pH 7.03, glucose <20mg/dl, proteins 7g/dl, LDH 14,691U/l, ADA 137U/l, rheumatoid factor <9U/ml, triglycerides 17mg/dl and cholesterol 255mg/dl (in serum 186mg/dl).
Our case showed characteristics of pleural effusion due to rheumatoid arthritis (very low pH and glucose and high LDL levels) and pseudochylothorax (low triglycerides and high cholesterol concentration in pleural fluid), and adds to the few previous observations of pseudochylothorax associated with rheumatoid arthritis in the absence of pleural thickening. This finding suggests that pathogenic mechanisms must exist for the formation of this type of pleural effusion other than the chronic process of fluid within a fibrotic pleura,4 and confirms that the absence of pleural thickening does not rule out pseudochylothorax. Pseudochylothorax, if asymptomatic, does not require any specific treatment. However, when it occurs in association with rheumatoid arthritis, cases have been described in which intensive treatment of the underlying disease leads to control or resolution of the pseudochylothorax.
Our thanks to Eduardo García Pachón, without whom we could not have produced this paper.
Please cite this article as: Molina LZ, Redondo GM, Borbolla AM. Seudoquilotórax sin engrosamiento pleural asociado a artritis reumatoide. Arch Bronconeumol. 2016;52:533–534.