A 80-year-old male, smoker, presented with chronic complaints of dyspnoea, anorexia and asthenia. Lung sounds were absent on the lower two-thirds of the right hemithorax.
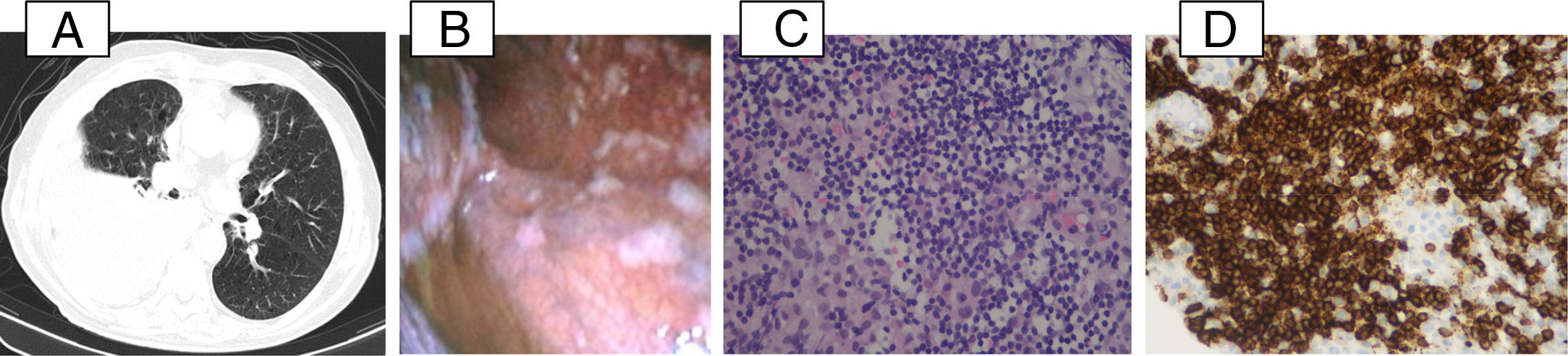
Chest computed tomography (CT) (Fig. 1A) confirmed the presence of extensive right pleural effusion, without mediastinal or hilar lymphadenopathies.
(A) Chest CT (axial plan (AP)): extensive right pleural effusion conditioning almost complete atelectasis of the middle and lower lobes. No mediastinal or hilar pulmonary lymphadenopathies were found. (B) Medical thoracoscopy: pericentrimetric macular lesions with multifocal distribution and stony consistency. (C) Small to intermedium lymphocytes with nuclear irregularity, admixed with mesothelial cells, H&E 400×. (D) Diffuse expression of CD20 in the neoplastic cells, 400×.
Thoracentesis revealed an exudative pleural effusion with absence of malignant cells.
Medical thoracoscopy allowed the visualization and biopsy of multifocal parietal pleural based pericentimetric macular lesions (Fig. 1B). Histopathological examination revealed small and intermediate cells (Fig. 1C), with eosinophilic cytoplasm and mild nuclear irregularity with occasional nucleoli, expressing CD20 (Fig. 1D), Bcl2, Bcl6, PAX5 and CD70a, CD10, MUM1 and p53; there was no expression of CD5 and TTF1; MIB-1 proliferative index was 50%. There was also mesothelial cells hyperplasia, with eosinophils.1,2
Neck, abdomen and bone positron emission CT showed no abnormalities.
A final diagnosis of primary pleural lymphoma (PPL) was made and chemotherapy was started. PPL is a rare cause of pleural effusion and its endoscopic appearance has seldom been fully characterized (both as multifocal nodular lesions and diffuse unspecified pleural involvement).3,4 The clinical manifestations are unspecific and large biopsy samples are the key to the diagnosis, allowing for extensive immunohistochemical analysis.