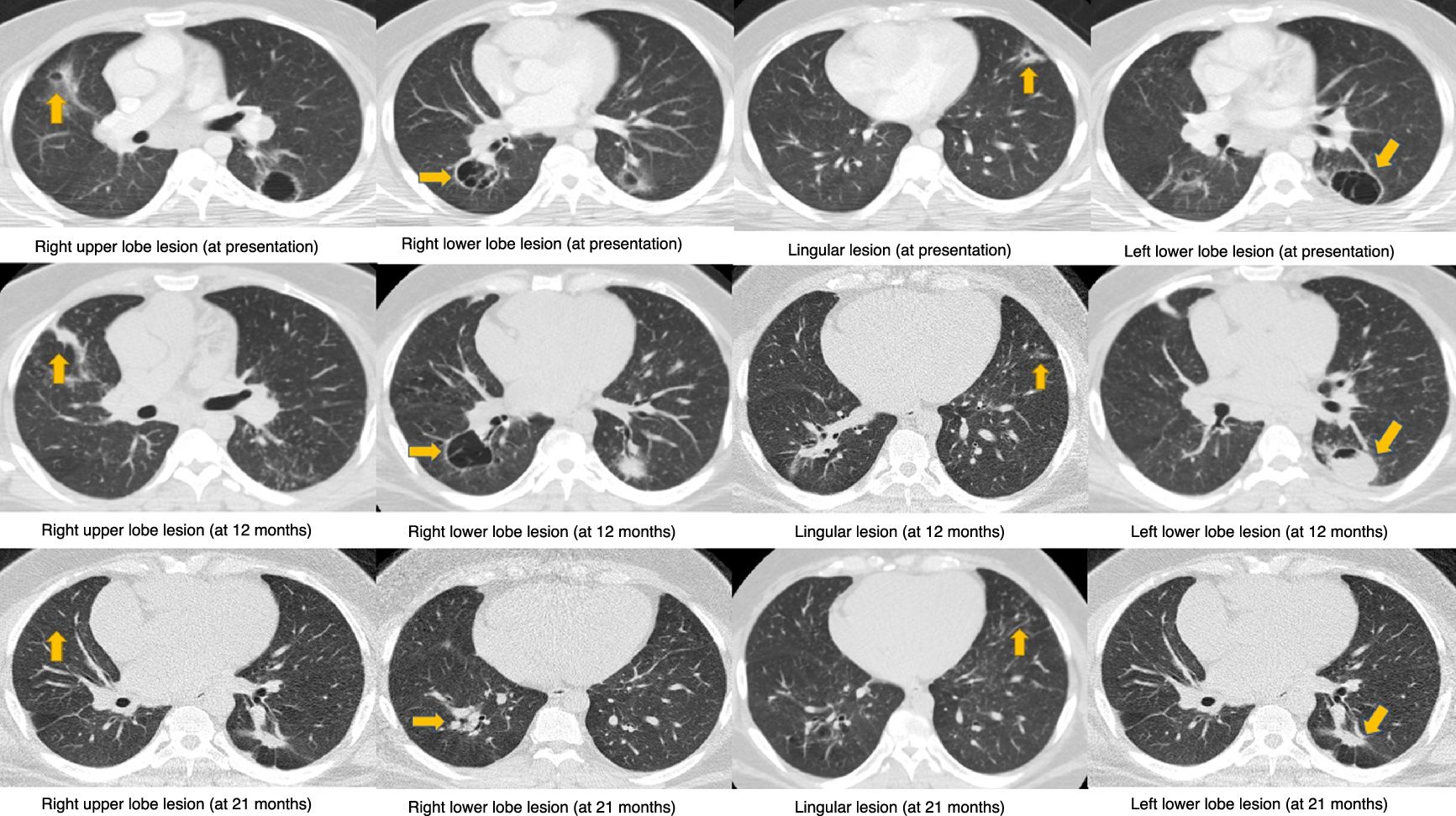
A 30-year-old male presented with a 6-month history of productive cough, dyspnea, hemoptysis, night sweats and 100-pound weight loss. Physical exam and initial blood work-up were non-revealing. CT scan of the chest revealed bilateral cavities (Fig. 1, first row). Differential diagnoses included malignancy, infections and inflammatory disorders. However, bacterial and mycobacterial stains and cultures were negative. Histoplasma and Blastomyces antigens, ANA, c-ANCA, p-ANCA and HIV serologies were also negative. Bronchoscopy revealed cystic lesions communicating with the airways. Bronchoalveolar fluid cultures were negative for bacteria and fungi. Transbronchial biopsies revealed noncaseating granulomas. Diagnosis of primary cavitary sarcoidosis was established and the patient started on prednisone and methotrexate. Sustained clinical improvement was noted only after six months of treatment. Lung cavitary lesions were noted to have significantly improved at 12 months (Fig. 1, second row) and almost completely resolved at 21 months (Fig. 1, third row). Primary cavitary sarcoidosis accounts for less than 0.6% of all sarcoidosis cases.1 Lower lobe predominance of the lung cavities, absence of other radiographic abnormalities such as nodularity, lymphadenopathy and calcification, and the presence of severe constitutional symptoms, set our case apart from previously published reports of primary cavitary sarcoidosis.2
Previous Presentation: This case was previously presented by the authors at the annual CHEST conference, Los Angles, 2016.