To determine the prevalence of occupational asthma (OA) and work-exacerbated asthma (WEA) among asthmatic patients diagnosed in Primary Health Care (PHC). To analyze the impact at PHC level caused by under-diagnosis and inappropriate referral of OA.
Patients and methodsA descriptive, cross-sectional multicenter study in patients aged between 16 and 64years diagnosed with asthma, according to their medical record; all were working or had worked, and were assigned to one of 16 PHC centers in a healthcare district. Based on the responses to the questionnaire completed at the study visit, which included a thorough review of the subject's entire working history, patients were classified into three categories by an expert in occupational asthma: OA, WEA or common asthma (CA).
ResultsThree hundred and sixty-eight patients completed the questionnaire. The prevalence of OA was 18.2% (25% in men and 14.6% in women, P=.046) and 54 patients (14.7%) were classified as WEA. The proportion of patients with work-related asthma (WRA) was therefore 32.9%. Asthmatic patients with WRA took more sick leave than CA patients (P<.001).
ConclusionsA high prevalence of WRA was found, mostly treated in PHC. Under-diagnosis of WRA is widespread in PHC.
Conocer la prevalencia de asma ocupacional (AO) y de asma exacerbada en el trabajo (AET) entre los pacientes diagnosticados de asma en la atención primaria (AP) de salud. Conocer el impacto en AP debido al infradiagnóstico y la no derivación del AO a la mutua laboral.
Pacientes y métodoEstudio descriptivo, transversal y multicéntrico, realizado en pacientes entre 16 y 64años diagnosticados de asma en la historia clínica, que estuvieran trabajando o hubieran trabajado, y asignados a cualquiera de los 16 equipos de AP de un sector sanitario. Basándose en las respuestas del cuestionario cumplimentado en la visita del estudio, que contenía una revisión exhaustiva de todas las etapas laborales del sujeto, un experto en asma laboral clasificaba a los asmáticos en 3 categorías: AO, AET o asma común (AC).
ResultadosDe los 368 pacientes que cumplimentaron el cuestionario se obtuvo una prevalencia de AO del 18,2% (25% en hombres y 14,6% en mujeres, p = 0,046) y 54 pacientes (14,7%) fueron clasificados como AET; así, el total de pacientes con asma relacionada con el trabajo (ART) resultó ser el 32,9%. Los pacientes con ART realizaron más bajas laborales que los pacientes con AC (p < 0,001).
ConclusionesSe obtiene una elevada prevalencia de ART atendida por la AP. Hay una baja sospecha por parte de la AP de ART.
Work-related asthma (WRT)1–3 is a term that covers all types of asthma associated with the occupational environment. It includes both occupational asthma (OA), officially classified as work-related disease that is caused by exposure and conditions fully attributable to the working environment,1,4,5 and work-exacerbated asthma (WEA), which occurs when pre-existing or concurrent asthma is aggravated by workplace exposure.6
Epidemiological and clinical evidence suggests that asthma may be induced by exposure to multiple inhaled agents in the working environment – over 400, according to current estimations.2,7–9
OA is the most common occupational respiratory disease in industrialized countries.10,11 Although most studies12,13 report a WRA prevalence of between 5% and 25%, more recent reviews14,15 estimate that the mean risk attributable to working conditions is around 15%–16%. Moreover, the mean prevalence of WEA among adults with asthma is estimated to be 21%.6 Since asthma affects between 5% and 10% of adults in Europe (the estimated prevalence in Spain is 5%),16,17 WRA is a serious public health problem with significant socioeconomic implications.13,18,19
One major occupational health problem in Spain is that OA is frequently not detected and diagnosed as such in the specialized departments of the occupational healthcare system, consisting of company healthcare provisions and the MATEPSS (the work-related accidents and occupational diseases insurance section of the Spanish social security system). Instead it is diagnosed and treated as a common non-work-related disease within the primary health care (PHC) system.20,21 This results in either a delay in diagnosis of WRA, or a complete failure to diagnosis the condition as work-related. This situation causes serious harm: affected workers continue to be exposed to the causative agent and their condition deteriorates, chronicity sets in and they lose their capacity for work. Other workers, too, may suffer from the same exposure while performing similar tasks, since the company fails to implement preventive measures for avoiding new cases. To minimize both delay in diagnosis and long-term decline due to WRA, primary care physicians, when diagnosing asthma in adults, must always consider the possibility that the disease may be work-related.22
Although some estimations of the healthcare costs of work-related asthma have been made,18 no studies have been conducted in our setting that quantify, based on the number of patients seen, the true burden of this shift of patients and costs toward PHC. We know that the problem exists but we are unaware of its real magnitude.
The purpose of this study was to estimate the prevalence of WRA (both OA and WEA) in patients diagnosed with asthma, and to determine the real impact on PHC caused by underdiagnosis and failure to refer cases of OA to occupational insurance companies. We aimed to determine the prevalence of patients with OA treated in PHC (who should have been seen in the MATEPSS), and to calculate the burden in terms of both costs and workload. This knowledge is essential for adopting corrective measures and achieving the final objective: to improve the healthcare and occupational prognosis of patients with OA and WEA, and to improve risk prevention in the workplace, thereby reducing the incidence of new cases.
MethodsThis was a descriptive, cross-sectional, multicenter study, conducted in the territorial framework of a healthcare district with 16 PHC teams and a population distributed among semi-rural and urban areas. According to the 2009 municipal register, the total population of the area is 384718 inhabitants, all of whom are entitled to public healthcare and have been assigned to a PHC center, according to their place of residence.
Study SubjectsThe study population comprised patients between 16 and 64 years of age with a diagnosis of asthma (ICD J45) in their electronic medical record (EMR). All subjects had their own social security number, indicating that they were working or had worked, and were assigned to one of the 81 family doctors in the region who had agreed to participate in the study.
Exclusion Criteria- •
Individuals younger than 25 years diagnosed with asthma before the age of 15 years who had not received medication for asthma in the previous 2 years.
- •
Individuals with any other respiratory disease that did not meet the diagnostic criteria for asthma.
- •
Individuals requiring palliative care.
- •
Individuals included in a home care program.
- •
Individuals with communication difficulties (cognitive or sensory impairment, language barrier).
- •
Individuals who refused to participate in the study.
- •
Individuals who could not be contacted after 3 phone calls to their home at different times of the day.
Assuming an alpha risk of 0.05 for a 3% level of accuracy in a two-tailed comparison for an estimated 10% of OA patients among all asthma patients, a randomized sample of 385 asthma patients will be required. This calculation was made using the GRANMO sample size calculator, version 7. Asthma patients were selected by simple randomized sampling from EMRs available in the PHC centers.
VariablesDependent variable:
- •
Diagnosis of asthma: OA, WEA, common asthma (CA).
Independent variables:
- •
Sociodemographic variables: sex, age and country of birth.
- •
Smoking-related variables: never smoker, smoker, former smoker, and pack-years.
- •
Variables related with exposure to non-occupational triggers: pharmacological treatments, pets, seasonal symptoms.
Variables related with working life:
- •
Current employment status.
- •
Employment status at onset of asthma symptoms.
- •
Employment history.
- •
Asthma symptoms.
- •
Economic factors impacting PHC: sick leave due to asthma, number of visits to PHC physician, number of inhaled drug containers used per respiratory disease and expenditure in euros for the inhaled drugs used per respiratory disease. Medication use was estimated from the collection from the pharmacy of drugs prescribed by the physician.
The study project was presented to the 16 PHC centers by members of the study team, and 81 family doctors from a total of 102 agreed to participate. In May 2009, this group of 81 co-investigators (CI) met and received specific training in asthma. A member of the study team was assigned to each doctor for consultation purposes throughout the study. Patients were recruited between July 2009 and February 2010 from a randomized list (supplied by the central computer department) of subjects who met the entry criteria and were assigned to one of the 81 participating CIs. Each CI used the inclusion and exclusion criteria to screen patients, following the list consecutively until the required sample size was achieved. As already mentioned, patients with a diagnosis of asthma in their EMR were included in the study. Each CI reviewed the EMRs of his/her own patients, and confirmed the diagnosis of asthma using clinical criteria (predominantly nocturnal cough, dyspnea during attacks or on effort, wheezing that worsens in certain situations, improvement of symptoms with bronchodilators and/or inhaled corticosteroids) and lung function criteria (spirometry, variability in peak expiratory flow, methacoline test). Doubts were discussed with the assigned study team member. Patients were given an appointment at the health center, and, if they agreed to participate in the study, signed the informed consent form. The patients were then interviewed using a structured questionnaire that contained a comprehensive review of the subject's full employment history. A list of occupations and activities related with OA was provided, along with the main chemical agents and/or products causing OA. In order to avoid bias, this questionnaire was administered by a single, trained member of staff, specifically employed to perform this task in all health centers. The Spanish or Catalan language was used, as appropriate.
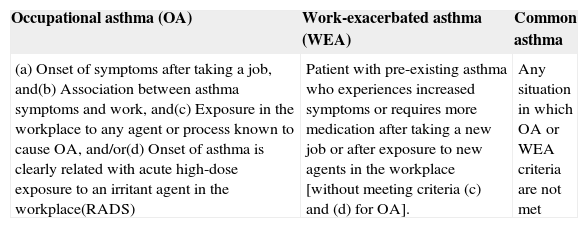
A member of the study team experienced in work-related asthma was responsible for classifying asthma patients into 3 categories: OA, WEA and CA. In view of the epidemiological objective of this study, asthma patients were classified as OA, WEA or CA, based on the correlation between the timing of clinical symptoms, the working environment, and exposure suffered by the patients, as described in the criteria of the American College of Chest Physicians.23
Classification criteria:
| Occupational asthma (OA) | Work-exacerbated asthma (WEA) | Common asthma |
|---|---|---|
| (a) Onset of symptoms after taking a job, and(b) Association between asthma symptoms and work, and(c) Exposure in the workplace to any agent or process known to cause OA, and/or(d) Onset of asthma is clearly related with acute high-dose exposure to an irritant agent in the workplace(RADS) | Patient with pre-existing asthma who experiences increased symptoms or requires more medication after taking a new job or after exposure to new agents in the workplace [without meeting criteria (c) and (d) for OA]. | Any situation in which OA or WEA criteria are not met |
RADS: reactive airways dysfunction syndrome.
All cases of OA must meet 3 criteria: (a) and (b) plus (c) or (d).
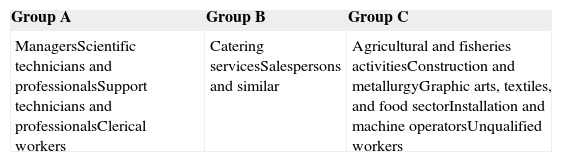
The Catalan Classification of Occupations 1994 (CCO-94), the Catalan version of the National Classification of Occupations 1994 (CNO-94), was used for coding the occupations recorded in the questionnaire. In view of the wide range of jobs, these activities were pooled into 3 large groups (A–C), according to the type of work and the possibility and similarity of exposure to allergens.
| Group A | Group B | Group C |
|---|---|---|
| ManagersScientific technicians and professionalsSupport technicians and professionalsClerical workers | Catering servicesSalespersons and similar | Agricultural and fisheries activitiesConstruction and metallurgyGraphic arts, textiles, and food sectorInstallation and machine operatorsUnqualified workers |
Retrospective data on sick leave were obtained from the EMR of the study subjects, confirming that this was due to asthma, as well as the number of medical visits during 2009. Use of medications was also retrospectively collected for the same period from pharmacy department records.
Statistical AnalysisThe database used was specifically designed for the study, and data quality was closely scrutinized. The prevalence of OA was determined by calculating the percentage of patients with OA compared to the total number of asthma patients in the sample. The prevalence of WRA was the sum of this percentage and the percentage of patients with WEA. Univariate descriptive statistics were performed on all variables collected: frequency and percentage for qualitative variables, and mean and standard deviation for quantitative variables, since these showed a normal distribution. Normality was confirmed numerically using the Skewness and Kurtosis test (sktest). The prevalence of the different types of asthma (CA, WEA and OA) was compared according to patient characteristics, and proportions were compared using the Chi-squared test for qualitative variables and analysis of variance (ANOVA) for quantitative variables. Finally, a polynomial multivariate logistic regression model was fitted to evaluate the association between the asthma diagnosis and the characteristics of the study patients. All statistical tests were performed with a 2-tailed 95% confidence level, using the Stata/SE Version 12.1 statistical package (StataCorp, Collage Station, TX, USA).
LimitationsSince the procedure used for selecting patients may have led to dubious or erroneous asthma diagnoses, diagnostic criteria were reviewed for all study subjects who were classified in their medical records as asthmatic. If the diagnosis was not confirmed, the subject was excluded from the sample, or, in case of doubt, the medical record was reviewed and any necessary additional testing was performed. If the participating physician was still unsure, he/she consulted the study team before including the patient in the study. This was an epidemiological study, but the collection of data on the diagnosis of OA from the patients’ medical records must still be recognized as a limitation.24
ResultsAt total of 2505 patients with a diagnosis of asthma were identified from a population of 102131 subjects aged between 16 and 64 years. The recorded asthma prevalence in this study population was 2.5%.
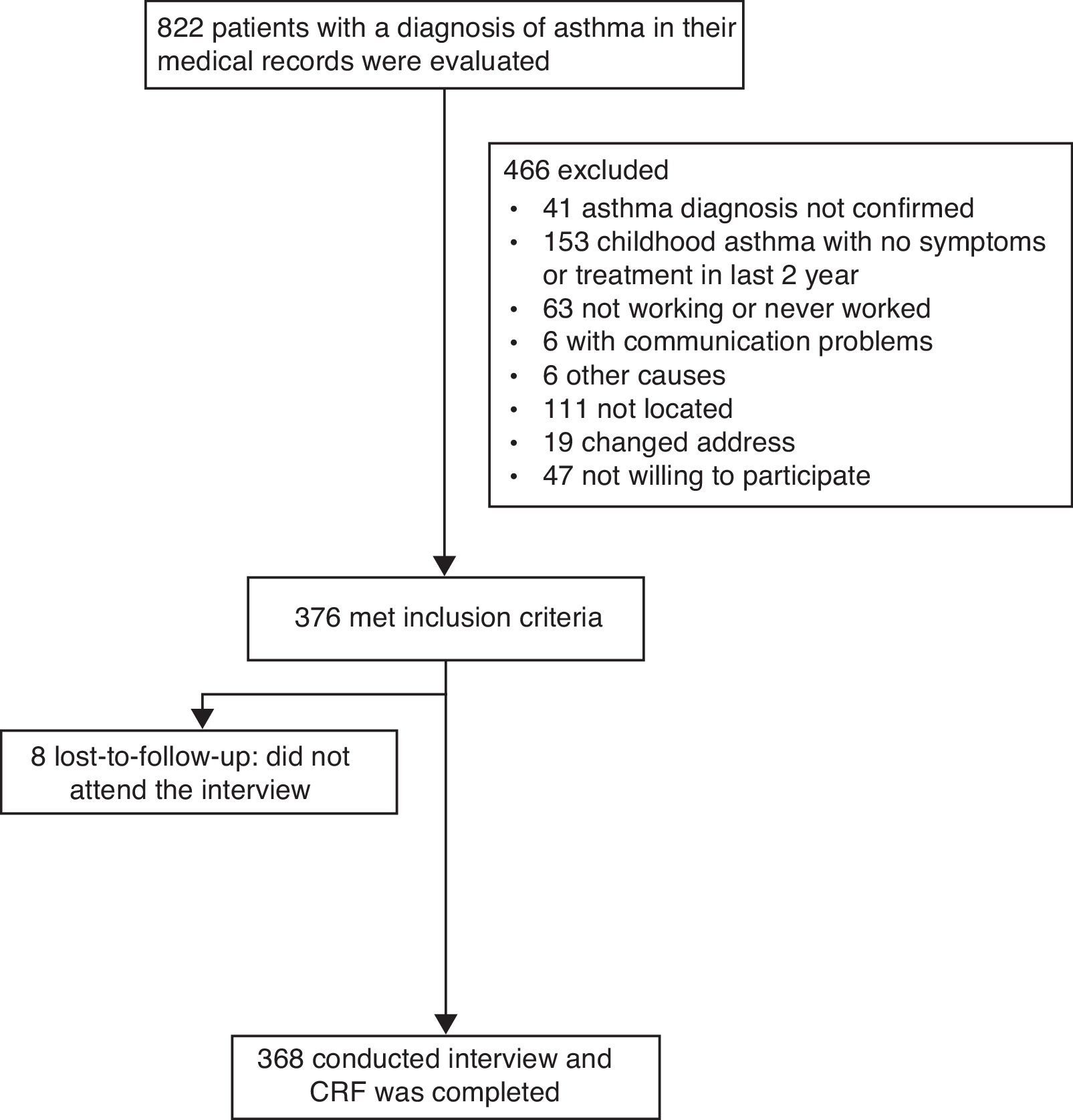
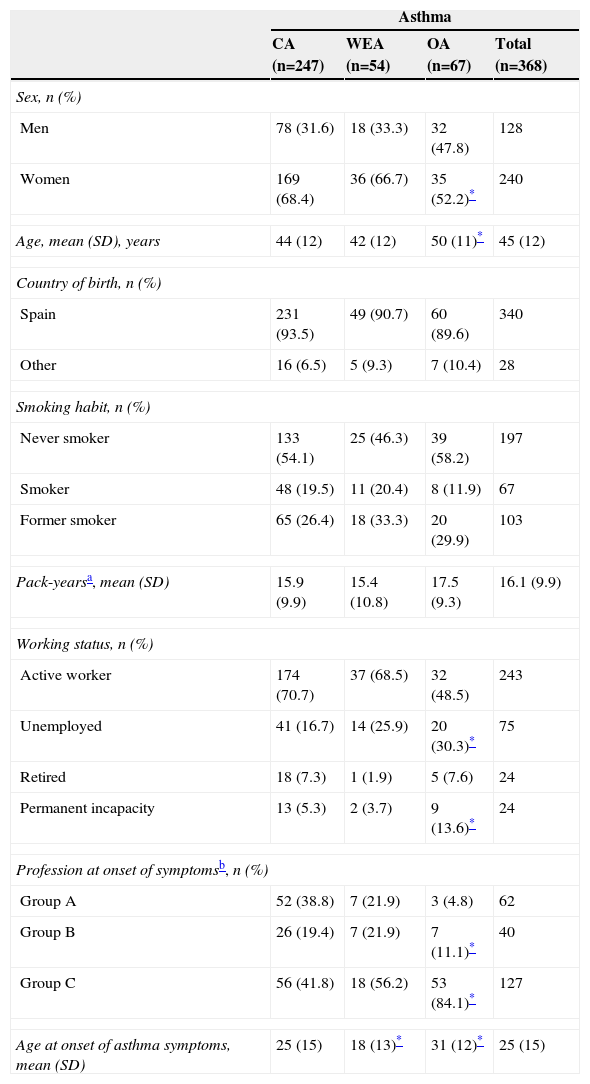
The medical records of 822 asthma patients were reviewed to include a total of 368 in the study (Fig. 1). Table 1 shows the characteristics of these patients, according to their asthma diagnosis. A total of 67 were diagnosed with OA, corresponding to a prevalence of 18.2%, with respect to the total number of study patients aged between 16 and 64 years. Prevalence was greater in men than in women (P=.046). If the 54 patients with WEA are included, the overall prevalence of work-related asthma was 32.9%. Only 2 of the 368 cases reviewed had been referred to occupational insurance facilities due to clearly suspected OA.
Characteristics of Study Subjects According to Their Asthma Diagnosis.
| Asthma | ||||
|---|---|---|---|---|
| CA (n=247) | WEA (n=54) | OA (n=67) | Total (n=368) | |
| Sex, n (%) | ||||
| Men | 78 (31.6) | 18 (33.3) | 32 (47.8) | 128 |
| Women | 169 (68.4) | 36 (66.7) | 35 (52.2)* | 240 |
| Age, mean (SD), years | 44 (12) | 42 (12) | 50 (11)* | 45 (12) |
| Country of birth, n (%) | ||||
| Spain | 231 (93.5) | 49 (90.7) | 60 (89.6) | 340 |
| Other | 16 (6.5) | 5 (9.3) | 7 (10.4) | 28 |
| Smoking habit, n (%) | ||||
| Never smoker | 133 (54.1) | 25 (46.3) | 39 (58.2) | 197 |
| Smoker | 48 (19.5) | 11 (20.4) | 8 (11.9) | 67 |
| Former smoker | 65 (26.4) | 18 (33.3) | 20 (29.9) | 103 |
| Pack-yearsa, mean (SD) | 15.9 (9.9) | 15.4 (10.8) | 17.5 (9.3) | 16.1 (9.9) |
| Working status, n (%) | ||||
| Active worker | 174 (70.7) | 37 (68.5) | 32 (48.5) | 243 |
| Unemployed | 41 (16.7) | 14 (25.9) | 20 (30.3)* | 75 |
| Retired | 18 (7.3) | 1 (1.9) | 5 (7.6) | 24 |
| Permanent incapacity | 13 (5.3) | 2 (3.7) | 9 (13.6)* | 24 |
| Profession at onset of symptomsb, n (%) | ||||
| Group A | 52 (38.8) | 7 (21.9) | 3 (4.8) | 62 |
| Group B | 26 (19.4) | 7 (21.9) | 7 (11.1)* | 40 |
| Group C | 56 (41.8) | 18 (56.2) | 53 (84.1)* | 127 |
| Age at onset of asthma symptoms, mean (SD) | 25 (15) | 18 (13)* | 31 (12)* | 25 (15) |
CA: common asthma; OA: occupational asthma; SD: standard deviation; WEA: work-exacerbated asthma.
P<.05 when compared with the reference category using the Chi-squared test for qualitative variables and when compared with CA using analysis of variance (ANOVA) for quantitative variables.
Catalan Occupational Classification (CCO-94): Group A (managers, scientific technicians and professionals, support technicians and professionals, clerical workers); Group B (catering services, salespersons, and similar); Group C (agricultural and fisheries activities, construction and metallurgy, graphic arts, textiles and food sector, installation and machine operators, unqualified workers).
Patients with OA were significantly older than the other asthma patients (P<.001), and were also significantly older at onset of symptoms (P<.001) (Table 1). Prevalence of OA in unemployed subjects or those considered to have permanent incapacity was higher than in asthma patients in active employment (P=.013). The prevalence of OA in patients in occupational groups B or C at onset of symptoms was also higher than in group A subjects (P<.001) (Table 1). After performing the multivariate analysis, the characteristics that were eventually significantly associated with a higher prevalence of OA were symptom onset at an older age, and employment in group B or C occupations at the time of symptom onset.
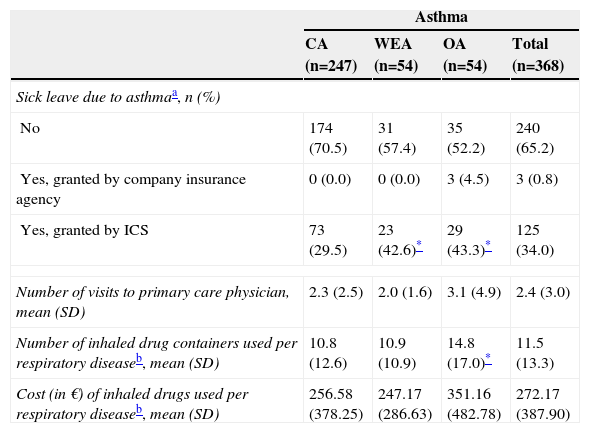
Table 2 shows the use of resources generated over 1 year by study patients, according to their asthma diagnosis. Patients with work-related asthma (OA and WEA) took more sick leave for common illness granted by doctors from the PHC system than those with CA (P<.001). In 1 year, patients with OA made a mean of 3.1 visits to their PHC physician, and used 14.8 containers of inhaled drugs (P=.048), at a cost of €351.16. These figures were higher for OA patients than for those with CA and WEA, but the differences were not statistically significant. With regard to hospital admissions and visits to the emergency department due to asthma, only 2 patients with OA were hospitalized during 2009.
Use of Resources During the Period of One Year Generated by Study Subjects According to Asthma Diagnosis.
| Asthma | ||||
|---|---|---|---|---|
| CA (n=247) | WEA (n=54) | OA (n=54) | Total (n=368) | |
| Sick leave due to asthmaa, n (%) | ||||
| No | 174 (70.5) | 31 (57.4) | 35 (52.2) | 240 (65.2) |
| Yes, granted by company insurance agency | 0 (0.0) | 0 (0.0) | 3 (4.5) | 3 (0.8) |
| Yes, granted by ICS | 73 (29.5) | 23 (42.6)* | 29 (43.3)* | 125 (34.0) |
| Number of visits to primary care physician, mean (SD) | 2.3 (2.5) | 2.0 (1.6) | 3.1 (4.9) | 2.4 (3.0) |
| Number of inhaled drug containers used per respiratory diseaseb, mean (SD) | 10.8 (12.6) | 10.9 (10.9) | 14.8 (17.0)* | 11.5 (13.3) |
| Cost (in €) of inhaled drugs used per respiratory diseaseb, mean (SD) | 256.58 (378.25) | 247.17 (286.63) | 351.16 (482.78) | 272.17 (387.90) |
CA: common asthma; ICS: Catalan Institute of Health; OA: occupational asthma; SD: standard deviation; WEA: work-exacerbated asthma.
Of the 67 patients with OA, 11 (16.4%) had been seen on at least 1 occasion for asthma in the MATEPSS, and of these, 5 had been seen on 2 or more occasions in their occupational insurance company. The remaining patients were always treated in the PHC system. Furthermore, 62 (16.8%) patients did not require inhaled medication (12 with OA [17.9% of OA patients], 8 with WEA [14.8% of those with WEA] and 42 with CA [17.0% of those with CA]), although these differences were not statistically significant.
DiscussionThe results suggest that in 32.9% of asthma patients treated in the PHC system, there is a relationship between their disease and their working environment. In 18.2%, the asthma was caused by conditions in the workplace itself, while in 14.7%, it was exacerbated in the workplace.
Variability in study methods and definitions mean that the prevalence of WRA is not well defined in general, and our results are comparable to those of other reviews, both European and American, that reported wide ranges of between 5% and 25%.12–15 The significance of this study is that it was conducted in the primary care setting of the public health service. Classification of patients into 3 categories (OA, WEA and CA) by a specialist physician using data collected in a questionnaire is not exempt from problems, but we believe that it is a method fit for the purposes of this study. This methodology may underestimate cases of OA, and may not be helpful in assessing the prevalence of WRA.25 Nonetheless, additional testing (such as sensitization or specific bronchial hyperreactivity testing), while necessary in individual diagnosis due to the medical and/or legal implications of the disease, does not provide any relevant supplementary information26 in population studies.
The low prevalence (2.5%) of asthma observed in our study is because of under-reporting of the disease, both due to the problem of under-reporting itself, and because the study was performed in the early years after switching from paper medical records to the EMR, and transfer of diagnoses was not automatic.
While the total number of women with asthma is higher than that of men, a greater percentage of men have OA. This discrepancy cannot be explained simply by differences in exposure to allergens.27,28 Some studies have reported a higher risk of OA in women employed as domestic cleaners.29 This parameter is not so discernible in our study, probably because cleaners are unofficially employed and so do not have their own social security number, a requisite for inclusion in this study. As asthma in this population cannot be legally classified as OA, many women are diagnosed as having CA when they really have OA.
Patients with OA are older than those with WEA and CA. In OA, asthma is triggered by working conditions, and a period of sensitization is needed before the disease manifests.30 In contrast, CA and WEA are triggered by factors encountered before the work-related exposure. Onset of symptoms in patients with WEA occurs at a very young age, suggesting that aggravation of childhood or pre-existing asthma due to work exposure occurs rapidly. A total of 27% of patients whose asthma was diagnosed after the age of 30 years were diagnosed with OA. This would suggest that when asthma is diagnosed in adults, the possibility that the disease may be work-related must be explored.
With regard to the patients’ country of origin, it is interesting to note that immigrants are not overrepresented among cases of OA or, especially, WEA, despite them having jobs that might involve a greater risk of exposure to more allergenic substances with fewer protective measures. However, conclusions cannot be drawn, due to the small numbers in our sample. No differences were observed between smoking habit and the different types of asthma.
Unemployment and incapacity for work in patients with OA are significantly higher than in other groups. It seems very likely that the disease affects sufferers’ possibilities of finding work and being declared with permanent incapacity for work by Employment Institute inspectors. This fact shows how the course of asthma can be particularly incapacitating for OA patients. Moreover, if the patient's disease is not recognized as occupational, their financial situation can be severely affected. Patients with OA and WEA have more episodes of temporary incapacity for work due to asthma (only 4.5% of these were granted by the occupational insurance agencies) than patients with CA. This is another indication of the poor progress of WRA patients caused by continuous exposure to the allergens that trigger or exacerbate their asthma.
Data on medication use show that, although the proportion of CA and OA patients who do not need asthma medication (estimated from pharmacy use) is similar, the number of containers used by OA subjects is significantly higher. Expenditure on medication use by patients with OA is higher than in those with CA. The number of visits to PHC is also higher in OA, although the difference is not statistically significant. Curiously, the behavior of WEA subjects is similar to that of those with CA.
In short, OA patients use more healthcare resources than other patients with asthma. In fact, according to legal provisions (Legislative Royal Decree 1/1994, 20 June 1994, approving the Consolidated General Social Security Act), patients with OA should be referred to and treated by the occupational healthcare system, which is not the case.
ConclusionsThis study underscores the high prevalence of WRA treated in PHC centers. The healthcare burden is high, and treatment in the PHC system does not contribute to any improvement in the health of these patients, since the working conditions that trigger or aggravate their disease remain unchanged.
It must also be emphasized that OA is rarely suspected in the PHC system: the possibility of OA was considered in only 2 of the 368 cases reviewed. These findings are consistent with those from other studies.31 OA should be considered more often as a diagnosis in all adults with symptoms indicative of asthma. Information on current and previous working environments should be included in the patient's medical record.
Our proposal, also suggested in other European studies,32,33 is to implement protocols encouraging the suspicion and detection of WRA in primary care, as well as better detection and follow-up by occupational insurance agencies. This would increase the diagnostic rate and improve the disease course and prognosis of patients with OA, and appropriate preventive measures could be introduced to help reduce the incidence of new cases. We must all work toward greater communication and collaboration between the public healthcare system and the occupational healthcare system (MATEPSS), in order to improve the diagnosis, treatment, and outcome of patients with this disease.
Ethical ResponsibilitiesThis study was approved by the Clinical Research Ethics Committee of the Instituto de Investigación en Atención Primaria (IDIAP) Jordi Gol (Barcelona).
The investigators complied with current Good Clinical Practice guidelines and respected the requirements of the Declaration of Helsinki (1975). Accordingly, a 7-digit code was used to anonymize the patients: the first 2 digits identified the study site, the next 2 digits identified the medic who made the evaluation, and the final 3 digits reflected the order of inclusion of the patient in the study. During the first visit, the healthcare professional provided the patient with an information sheet and requested their voluntary participation, and the informed consent form was signed.
FundingThis study was made possible by a grant from the Instituto de Investigación en Atención Primaria (IDIAP) Jordi Gol (Barcelona), conceded in 2008.
Conflict of InterestThe authors state that they had no conflict of interests.
Our thanks to the physicians who collaborated in the study: Maria Calvo, Laura Montes, Escolàstica Ruiz, Agustí Utgés, Enric Zamorano (EAP Alt Mogent); Isabel Grau, Carles Monsó, Montserrat Castellet (EAP Caldes de Montbui); Ginesa Acosta, Susana Galvez, Ramon Ortega, Alejandro Serracant, Isabel Torras (EAP Cardedeu); Jordi Martí, Rafael Martinez, Joan Mogas, Lydia Roig, Fina Romanyà, Ana Turnes (EAP La Garriga); Irene Garcia, Felipe M. Hernandez, M. Teresa Rodellar (EAP Canovellas); Glòria Anton, Montserrat Arumí, José Casermeiro, Leonor Castillo, Miquel Presas, Regina Malfeito, Ramon Velayos (EAP Les Franqueses); Amada Aguyé, M. José Armenteros, Mercedes Freire, Valentina Herrero, Margarita Lorenzo, Carolina Moragues, Mireia Prat, Jordi Ralla, Mireia Rosás (EAP Granollers Centre); Josep Espinasa, Anna Estefanell, Montse Gil, Sandra Masuet, Judith Gonzalez, Anna Pérez, Josep M. Viaplana (EAP St. Miquel); Melani Ardite, Alejandro J. Bilardi, Dídac Forés, Xavi Martínez, Santiago Perez (EAP La Llagosta); Ignacio Olivares, Marta Pastor, Carmen Pereira (EAP Mollet Est); Mercè Ariasol, Angel Garcia, Neus Jou, Elisabeth Navarro, Consol Sanchez (EAP Mollet Oest); Eduard Carrion, Julian Ortega, Ana Pérez (EAP Montmeló-Montornés); Carmen Cerrillo, Lola Cobos (EAP Parets); Pere Antoja, M. Luz Ramiro (EAP Sant Fost); Anna Albi, Milagros Herrero, Èlia Jorba Casellas (EAP St. Celoni); Genís Iglesias, Sabina Molina, Anna Parera, David Miramanda, Rafael Velasco, Marga Vilageliu (EAP Vall del Tenes).
We would especially like to thank Dr. Joan Pujol for his collaboration in the design and follow-up of the study, and Pati Luque for her meticulous and efficient management of the interviews, the data and certificates. Thanks also to Laia Jaquet for her dedication in conducting this study.
Please cite this article as: Vila-Rigat R, Panadès Valls R, Hernandez Huet E, Sivecas Maristany J, Blanché Prat X, Muñoz-Ortiz L, et al. Prevalencia de asma relacionada con el trabajo y su impacto en atención primaria de salud. Arch Bronconeumol. 2015;51:449–455.