NECPAL is a tool for identification of patients with advanced chronic disease in need of palliative care. The main objective of the study is to know the prevalence of patients with palliative needs in an acute respiratory ward in a Spanish tertiary hospital using NECPAL. A second objective of the study is to know the annual mortality rate of these patients.
Materials and methodsCross sectional study and prospective monitoring of a cohort identified as palliative patients with the NECPAL tool for 12 months. Patient identification was performed in patients admitted to the respiratory ward of our hospital for longer than 3 days. We have assessed the annual vital status (deceased or not deceased) of patients and have recorded demographics, clinical and functional data, as well as the use of healthcare resources.
ResultsWe monitored a cohort of 363 patients. Of them, 87 patients (24.3%) (IC 95% 19–30) were identified as NECPAL positive. 60% of patients (n = 64) died within 12 months of their admission. There was no significant difference in the mortality ratio of oncologic versus non oncologic patients. In a multivariable analysis, mortality was associated with demand by patients or relatives for palliative care and with the presence of specific disease progression markers or indicators.
Conclusionsprevalence of patients with palliative needs in acute respiratory wards is high (one out of four patients). 60% of the patients identified as NECPAL positive in our cohort died in the first 12 months. Training of healthcare professionals as well as availability of appropriate resources are indispensable factors to improve care of this population.
El instrumento NECPAL es una herramienta para la identificación de personas en situación de enfermedad crónica avanzada con necesidades paliativas. El objetivo del estudio es conocer la prevalencia de pacientes con necesidades paliativas en un Servicio de Neumología de un hospital terciario mediante la herramienta NECPAL. Como objetivo secundario se plantea conocer la mortalidad al año de estos pacientes.
Material y métodosEstudio trasversal y seguimiento prospectivo de la cohorte de los pacientes identificados como paliativos con la herramienta NECPAL durante 12 meses. La identificación se realiza en pacientes ingresados > 3 días en una planta de Neumología. Hemos evaluado el estatus vital (fallecido o no fallecido) al año, así como datos demográficos clínicos, funcionales y uso de recursos sanitarios.
ResultadosSe analizaron 363 pacientes. De ellos, 87 (24,3%) (IC 95%, 19–30) fueron identificados como NECPAL positivos. En el seguimiento durante un año fallecieron 54 pacientes, un 60%. No hubo diferencias en mortalidad entre diagnósticos oncológicos y no oncológicos. En el análisis multivariante, la mortalidad se asoció a la demanda de paciente o familiares de atención paliativa y a la presencia de indicadores específicos de progresión de la enfermedad.
ConclusionesLa prevalencia de pacientes con necesidades paliativas en una planta de hospitalización de agudos de Neumología es alta (uno de cada cuatro pacientes). El 60% de los identificados como NECPAL positivos en nuestra serie fallece en los primeros 12 meses. Son necesarios formación y recursos para atender a estos pacientes.
In past 10 years, several guidelines for end-of-life care in patients with advanced respiratory disease have recommended offering chronic respiratory patients palliative care programs in earlier disease stages in parallel with treatments with curative intent, instead of delaying palliative care until death is imminent.1,2 However, difficulties in identifying candidate patients in the absence of criteria predicting short-term mortality, and breakdowns in coordination and communication between care levels mean that these proposals are not being adopted in routine clinical practice.
We have developed in our setting a palliative care plan aimed at providing quality palliative care to all individuals with oncological and non-oncological diseases in all care settings.3
Impaired quality of life, anxiety and depression, and the presence of incapacitating symptoms such as asthenia and dyspnea are just as prevalent in patients with advanced respiratory disease as in patients with cancer. However, 47%–60% of cancer patients receive palliative care, compared to only 1.5%–20% of patients with advanced respiratory disease, and time to inclusion in palliative care programs is longer in the latter group. Early identification and multidisciplinary management of patients with palliative needs offer clear benefits in terms of symptomatic control and quality of life.4–7
The first tool designed to identify patients in the community with advanced chronic conditions and palliative care needs was the Gold Standards Framework Prognostic Indicator Guidance (GSF-PIG) tool.8 The NECPAL (Palliative Needs) tool of the WHO Collaborating Center for Public Palliative Care Programs-Catalan Institute of Oncology (CCOMS-ICO)9,10 is an adaptation of the GSF-PIG that has been validated in Spain for the identification of individuals with advanced chronic disease and palliative care needs. This is a qualitative, multi-factorial, quantitative assessment that combines the perception of the treating physician (Surprise Question: “would you be surprised if the patient were to die in the next 12 months?”) with the patient’s or family’s preferences and objective indicators of disease severity and progression, comorbidity and use of services.
There is growing evidence that the NECPAL tool is useful for detecting individuals with advanced chronic diseases and palliative care needs. This tool has been tested in primary care to screen for patients with palliative needs, identifying an estimated prevalence of 1.5%.11 However, the few studies that have evaluated the prevalence of patients with palliative needs admitted to acute care hospitals have focused on the UK and Australia, whose health systems differ widely from ours.12–14
We therefore designed this study to determine the prevalence of patients with palliative needs in an acute respiratory medicine ward in a tertiary hospital, using the NECPAL tool. Our secondary objective was to estimate 1-year mortality in patients identified as NECPAL-positive (in need of palliative care) and to explore the factors associated with mortality, the characteristics of these patients, and the resources used.
MethodologyThis was a prospective, single-center, observational descriptive study with a 1-year follow-up.
Study population: We included all patients over 18 years of age admitted to the respiratory medicine unit of Hospital de Cruces (a tertiary acute care hospital) for more than 3 days on predetermined dates (1 day per month for 12 consecutive months between June 2017 and May 2018). Patients who had already been included or who refused to participate in the study were excluded.
The primary outcome variable in the cross-sectional study was the proportion of patients considered CCOMS-ICO NECPAL-positive, i.e., those in whom the answer to the first question “Would you be surprised if your patient were to die in the next 12 months?” was no, and who presented at least 1 other positive criterion.9
One-year mortality was assessed as a secondary outcome variable to calculate the predictive value of the tool. Demographic data and all variables collected with the NECPAL instrument were analyzed, including an assessment of dependence for activities of daily living (Barthel index), detection of emotional distress (DME scale), and dyspnea according to the modified MRC scale. Concomitant diseases (Charlson index), primary diagnosis at admission, and respiratory functional data (spirometry and blood gases) were also collected.
If the patient met the inclusion criteria, the NECPAL tool was completed by the treating clinician. If the patient was identified as needing palliative care, the patient or family members were followed up by telephone every 3 months, while routine clinical follow-up continued as normal. Electronic medical records were analyzed to determine the use of health resources in the following 12 months (number of admissions, days admitted, place of admission, and emergency visits), identification of the patient as palliative, use of prescribed opioids (except in the last 48 h of life), and record of psychological care in the medical history. A project-specific anonymized and encrypted database that met legal data protection requirements was created and approved by the hospital’s ethics committee.
Statistical analysisAccording to the sample size calculation based on an estimated prevalence of 27%,12 302 patients were required to achieve a 95% confidence level, assuming a precision of 5%. Continuous variables were expressed as mean (standard deviation) in case of normal distribution or median (interquartile range) otherwise. Qualitative variables were shown as frequencies (percentages). A bivariate analysis was conducted to identify predictors of mortality. Baseline sociodemographic and clinical factors of both groups were compared using the Student’s t-test for continuous variables that followed a normal distribution, or the Mann–Whitney U non-parametric test otherwise. The χ2-test was used for categorical variables.
Multivariate analysis was performed using Cox regression models, including variables that were significant as predictors in the bivariate analysis. Kaplan–Meier curves were constructed. Differences were considered statistically significant when p < 0.05. All analyses were performed using R statistical software (version 4.0.1 R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria.)
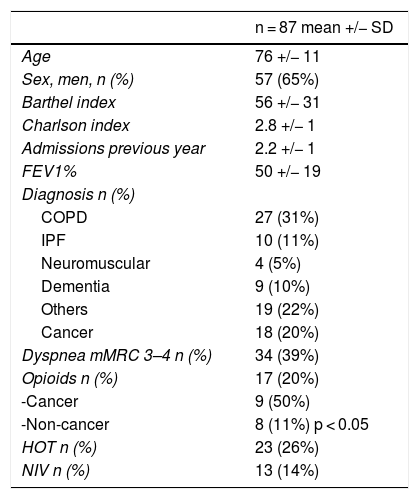
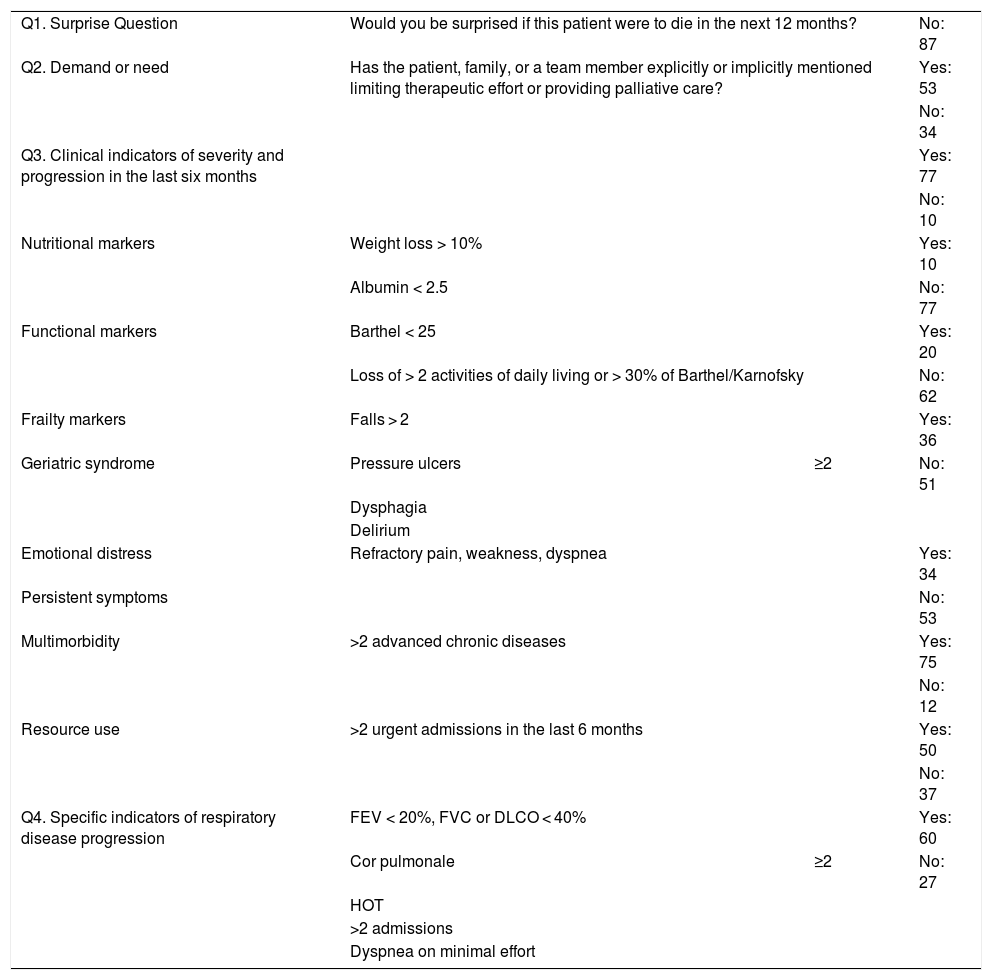
ResultsA total of 363 patients were included, of which 87 (24.3%, 95% CI: 19–30) were identified as NECPA-positive with palliative needs. Baseline patient characteristics are shown in Table 1. Table 2 shows the results of the variables collected with the NECPAL instrument.
Baseline data.
| n = 87 mean +/− SD | |
|---|---|
| Age | 76 +/− 11 |
| Sex, men, n (%) | 57 (65%) |
| Barthel index | 56 +/− 31 |
| Charlson index | 2.8 +/− 1 |
| Admissions previous year | 2.2 +/− 1 |
| FEV1% | 50 +/− 19 |
| Diagnosis n (%) | |
| COPD | 27 (31%) |
| IPF | 10 (11%) |
| Neuromuscular | 4 (5%) |
| Dementia | 9 (10%) |
| Others | 19 (22%) |
| Cancer | 18 (20%) |
| Dyspnea mMRC 3–4 n (%) | 34 (39%) |
| Opioids n (%) | 17 (20%) |
| -Cancer | 9 (50%) |
| -Non-cancer | 8 (11%) p < 0.05 |
| HOT n (%) | 23 (26%) |
| NIV n (%) | 13 (14%) |
COPD: chronic obstructive pulmonary disease.
FEV1% Forced expired volume in 1 s, % predicted.
HOT: home oxygen therapy.
IPF: idiopathic pulmonary fibrosis.
mMRC: Modified Medical Research Council dyspnea scale.
NIV: Non-invasive ventilation.
Results of variables collected using the NECPAL instrument version 2.0.
| Q1. Surprise Question | Would you be surprised if this patient were to die in the next 12 months? | No: 87 | |
| Q2. Demand or need | Has the patient, family, or a team member explicitly or implicitly mentioned limiting therapeutic effort or providing palliative care? | Yes: 53 | |
| No: 34 | |||
| Q3. Clinical indicators of severity and progression in the last six months | Yes: 77 | ||
| No: 10 | |||
| Nutritional markers | Weight loss > 10% | Yes: 10 | |
| Albumin < 2.5 | No: 77 | ||
| Functional markers | Barthel < 25 | Yes: 20 | |
| Loss of > 2 activities of daily living or > 30% of Barthel/Karnofsky | No: 62 | ||
| Frailty markers | Falls > 2 | Yes: 36 | |
| Geriatric syndrome | Pressure ulcers | ≥2 | No: 51 |
| Dysphagia | |||
| Delirium | |||
| Emotional distress | Refractory pain, weakness, dyspnea | Yes: 34 | |
| Persistent symptoms | No: 53 | ||
| Multimorbidity | >2 advanced chronic diseases | Yes: 75 | |
| No: 12 | |||
| Resource use | >2 urgent admissions in the last 6 months | Yes: 50 | |
| No: 37 | |||
| Q4. Specific indicators of respiratory disease progression | FEV < 20%, FVC or DLCO < 40% | Yes: 60 | |
| Cor pulmonale | ≥2 | No: 27 | |
| HOT | |||
| >2 admissions | |||
| Dyspnea on minimal effort | |||
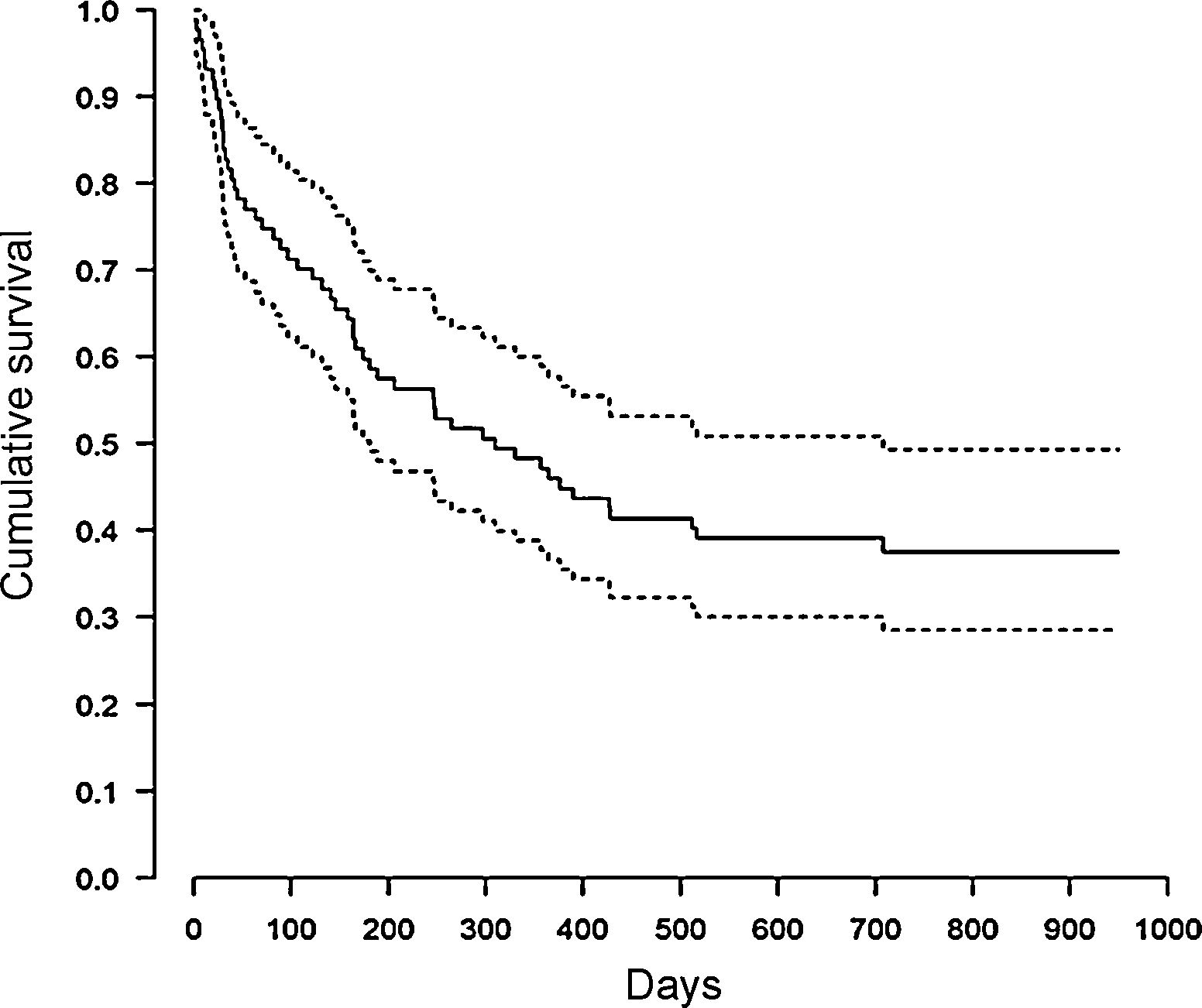
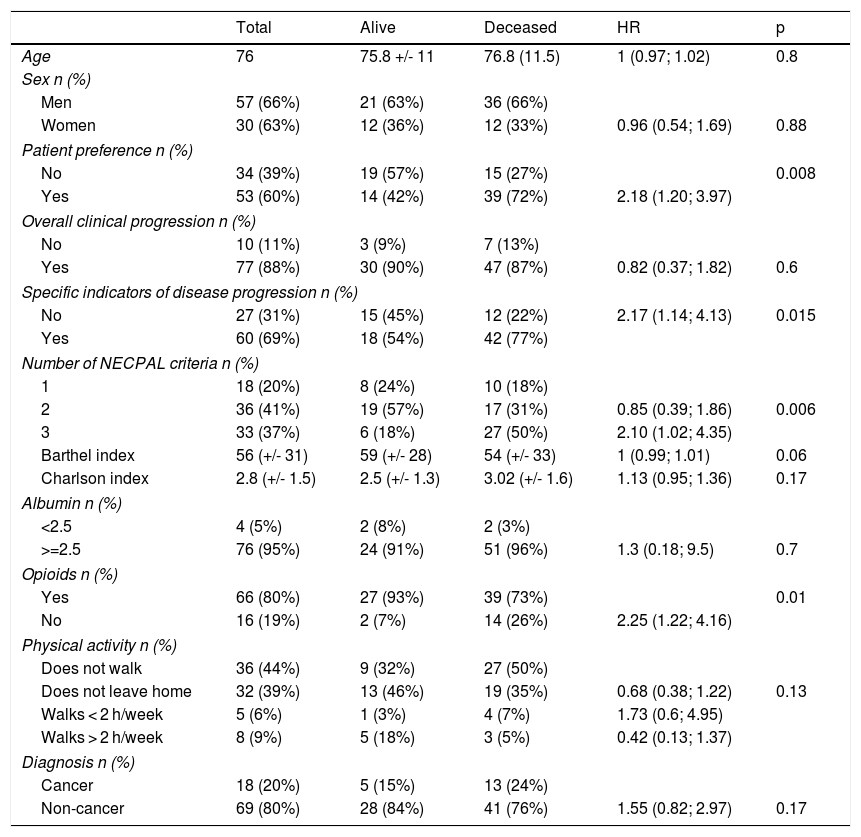
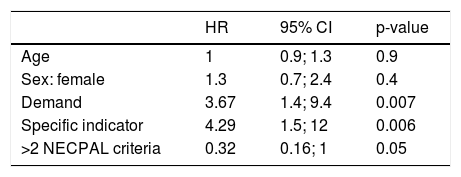
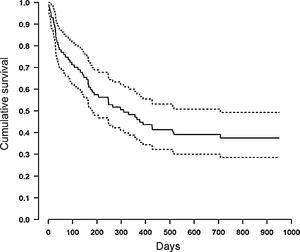
During the 12-month follow-up, 54 NECPAL-positive patients died (60%). Median survival was 10 months, 95% CI: 6–23 (Fig. 1). No patients were lost to follow-up. One-year mortality of NECPAL-negative patients was 11%. There were no differences in mortality between cancer and non-cancer patients. Table 3 shows the univariate analysis data. When the multivariate analysis was performed, a significant association was found between patient or family preference for palliative treatment and patient mortality, and also when the specific indicator for respiratory disease progression was positive (Table 4).
Univariate survival analysis for mortality. Hazard ratios (HR) and respective confidence intervals are displayed.
| Total | Alive | Deceased | HR | p | |
|---|---|---|---|---|---|
| Age | 76 | 75.8 +/- 11 | 76.8 (11.5) | 1 (0.97; 1.02) | 0.8 |
| Sex n (%) | |||||
| Men | 57 (66%) | 21 (63%) | 36 (66%) | ||
| Women | 30 (63%) | 12 (36%) | 12 (33%) | 0.96 (0.54; 1.69) | 0.88 |
| Patient preference n (%) | |||||
| No | 34 (39%) | 19 (57%) | 15 (27%) | 0.008 | |
| Yes | 53 (60%) | 14 (42%) | 39 (72%) | 2.18 (1.20; 3.97) | |
| Overall clinical progression n (%) | |||||
| No | 10 (11%) | 3 (9%) | 7 (13%) | ||
| Yes | 77 (88%) | 30 (90%) | 47 (87%) | 0.82 (0.37; 1.82) | 0.6 |
| Specific indicators of disease progression n (%) | |||||
| No | 27 (31%) | 15 (45%) | 12 (22%) | 2.17 (1.14; 4.13) | 0.015 |
| Yes | 60 (69%) | 18 (54%) | 42 (77%) | ||
| Number of NECPAL criteria n (%) | |||||
| 1 | 18 (20%) | 8 (24%) | 10 (18%) | ||
| 2 | 36 (41%) | 19 (57%) | 17 (31%) | 0.85 (0.39; 1.86) | 0.006 |
| 3 | 33 (37%) | 6 (18%) | 27 (50%) | 2.10 (1.02; 4.35) | |
| Barthel index | 56 (+/- 31) | 59 (+/- 28) | 54 (+/- 33) | 1 (0.99; 1.01) | 0.06 |
| Charlson index | 2.8 (+/- 1.5) | 2.5 (+/- 1.3) | 3.02 (+/- 1.6) | 1.13 (0.95; 1.36) | 0.17 |
| Albumin n (%) | |||||
| <2.5 | 4 (5%) | 2 (8%) | 2 (3%) | ||
| >=2.5 | 76 (95%) | 24 (91%) | 51 (96%) | 1.3 (0.18; 9.5) | 0.7 |
| Opioids n (%) | |||||
| Yes | 66 (80%) | 27 (93%) | 39 (73%) | 0.01 | |
| No | 16 (19%) | 2 (7%) | 14 (26%) | 2.25 (1.22; 4.16) | |
| Physical activity n (%) | |||||
| Does not walk | 36 (44%) | 9 (32%) | 27 (50%) | ||
| Does not leave home | 32 (39%) | 13 (46%) | 19 (35%) | 0.68 (0.38; 1.22) | 0.13 |
| Walks < 2 h/week | 5 (6%) | 1 (3%) | 4 (7%) | 1.73 (0.6; 4.95) | |
| Walks > 2 h/week | 8 (9%) | 5 (18%) | 3 (5%) | 0.42 (0.13; 1.37) | |
| Diagnosis n (%) | |||||
| Cancer | 18 (20%) | 5 (15%) | 13 (24%) | ||
| Non-cancer | 69 (80%) | 28 (84%) | 41 (76%) | 1.55 (0.82; 2.97) | 0.17 |
Regarding place of death, 25 patients (46%) died in acute care hospitals, 16 in medium-stay units (30%), and only 13 patients (24%) died at home or in a nursing home. At study baseline, only 5.7% of the patients had been coded as palliative in their medical history (5 patients); by the end of the 1-year follow-up, this percentage had risen to 34% (30 patients).
DiscussionThe proportion of patients with palliative needs identified with the NECPAL tool in our respiratory unit was 24%. Although no prevalence data in respiratory patients alone have been published to date, this rate is very similar to overall findings from acute care hospitals in other settings where disease types were not recorded. These studies reported results ranging between 19%–27% in New Zealand and Australia, and 36% in 2 hospitals in the United Kingdom.12–14
In other advanced single-organ, non-neoplastic diseases, the data vary more widely: for example, in the case of cirrhosis, up to 83% of patients admitted to a Portuguese acute care unit were classified as palliative,15 while in patients admitted with acute coronary syndrome, palliative needs were identified in between 8% and 23% of the study population.16,17 In Spain, a multicenter study of outpatients followed up in specialist heart failure clinics found that 32% of patients were NECPAL-positive.18
In our series, the most common primary diagnoses among patients with palliative needs were chronic obstructive pulmonary disease, followed by oncological disease. It should also be noted that the use of opioids is still higher in patients with cancer than other non-oncological diseases, despite their significant burden of symptoms, including dyspnea.19
The 1-year mortality rate (the primary study variable) among patients identified as palliative was 60%; this figure is similar to that of other cohorts of patients identified as palliative in acute hospitals,12,13 although the NECPAL tool was not designed to predict mortality. Mortality was similar in a small study of Spanish respiratory patients with palliative needs, identified using another method.20
In studies conducted in primary care, mortality in NECPAL-positive patients is significantly lower, at around 45%.10 A 1-year mortality rate of 21% was observed in patients with heart failure identified as palliative in a specialist outpatient clinic,18 probably because hospitalization itself indicates greater severity, highlighting the prognostic role of hospital admissions.
In a systematic review of 17 studies that analyzed the predictive value of the Surprise Question for mortality, the authors found it to be worse in non-cancer patients.21 However, in our study we found no differences in 1-year mortality among the various underlying diagnoses.
In the univariate analysis, opioid use and the presence of two or more NECPAL criteria were associated with higher mortality. However, in a multivariate analysis of mortality-related factors these variables carry less weight, and only patient or family preference for palliative care and the presence of a specific indicator of respiratory disease progression show a significant predictive value. This includes the presence of at least 2 of the following criteria: dyspnea on minimal exertion, FEV1 < 30% or DLCO < 40%, home oxygen therapy, associated heart failure, or more than 2 admissions in the previous year. We were surprised to find that other factors conventionally considered to be predictors of mortality, such as age or the Charlson index, did not emerge as significant.
The prognostic value of patient or family preference for palliative care suggests that this should be an important criterion to consider when initiating palliative care in a patient without discontinuing other treatments. This conclusion is in line with recent COPD reviews that show that none of the predicted mortality criteria proposed so far offer sufficient short- or medium-term validity, so the decision to initiate palliative care should be based on the existence of refractory symptoms and patient preference.22
The number of patients identified in their medical history as palliative, an important element in communication between levels of care, was very low in our series. Very few patients had been identified at baseline, although the data improved throughout the year of follow-up, with 34% being flagged by the end of study. Identifying a patient with palliative needs does not in any way mean that optimal treatment based on the evidence provided during admission should be discontinued, but rather that extra support should be offered to cover particular needs.
We believe that training and resources are needed to care for these patients.
A limitation of this study is that data were collected from a single hospital in a particular healthcare system, so generalization is difficult. To avoid screening biases, all patients admitted for more than 3 days were included on pre-determined days of the month throughout the year.
ConclusionsThe prevalence of patients with palliative needs in an acute respiratory ward is high (one in four patients), and of these, 60% die within 1 year. The assessment of hospitalized respiratory patients should include elements such as the Surprise Question, patient preferences, and specific criteria for respiratory disease progression.
Conflict of interestsThe authors state that they have no conflict of interests.
Please cite this article as: Tabernero Huguet E, Ortiz de Urbina Antia B, González Quero B, Garay Llorente E, Andia Iturrate J, Pérez Fernández S, et al. Prevalencia y mortalidad de pacientes con necesidades paliativas en una planta de Neumología. Estudio prospectivo. Arch Bronconeumol. 2021;57:345–350.