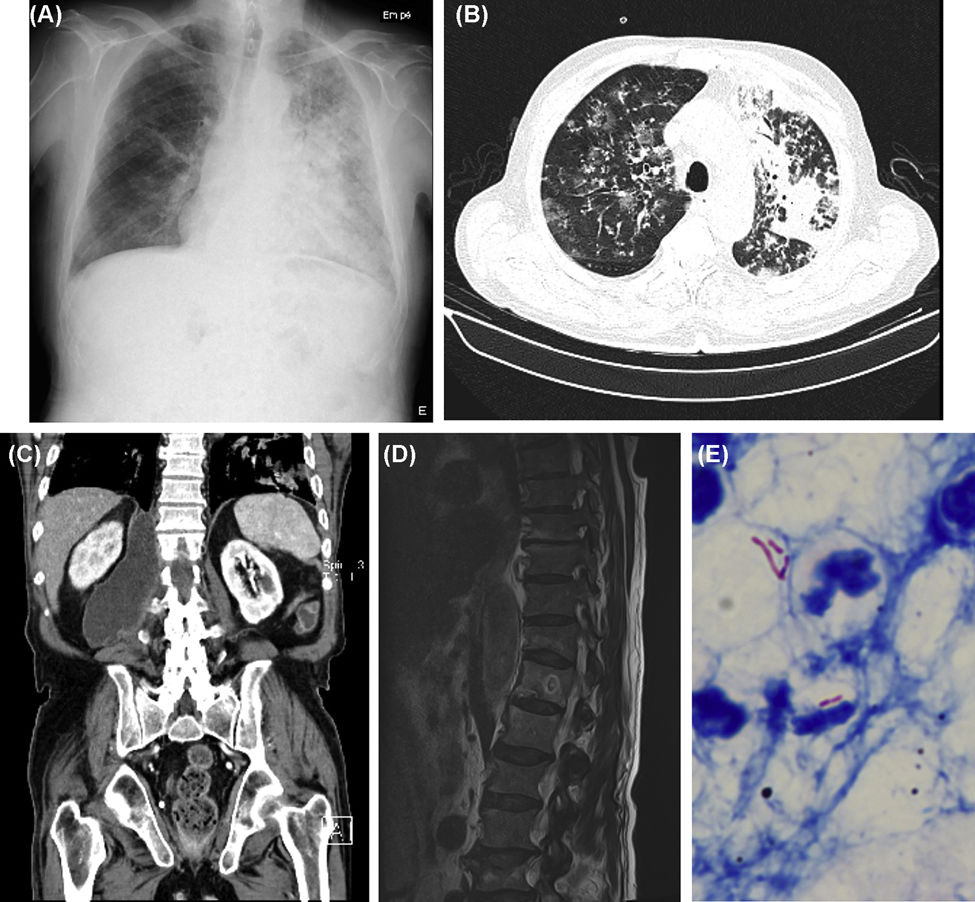
A 81-year-old male presenting with dyspnea, respiratory failure, chest radiography and thoracic CT abnormalities (Fig. 1A and B) was diagnosed with pulmonary TB after mycobacteriological sputum examination. Therapy with Isoniazid, Rifampin, Pyrazinamide and Ethambutol was initiated. During hospitalization, right lower limb (RLL) edema developed, leading to the hypothesis of lymphatic compression or deep vein thrombosis. Abdominal, pelvic and RLL CT were performed, with identification of right psoas abscess extending to L5 (Fig. 1C). Dorsolumbar spine MRI showed osteolytic and blastic lesions of D12 with cortical disruption, paravertebral soft tissue mass and enlargement of psoas muscle (Fig. 1D). The abscess was drained; sample smear showed acid-fast bacilli (Fig. 1E) and culture examination identified Mycobacterium tuberculosis, confirming bone involvement by TB with extension to the psoas muscle. Therapy was maintained for 12 months. Follow-up spine X-ray showed good evolution. Skeletal TB accounts for 1–3% of all TB cases and 10–35% of extrapulmonary TB, spinal involvement being the most common.1,2 However, only up to 5% of spinal TB patients develop psoas abscesses during disease course.1 Although identification of Mycobacterium tuberculosis in spinal lesions remains essential for definitive diagnosis, previous documentation from an extraspinal site is sufficient to establish the diagnosis in the proper clinical setting. Orthoses are usually necessary for prevention of further spinal damage. Surgery is required in selected cases: large abscess, severe deformities, neurological deficit or poor response to medical treatment.1 Being a rare form of extrapulmonary TB with nonspecific presentation, high clinical suspicion is needed in order to reduce diagnostic delay and prevent increased morbidity.
(A) Chest X-ray (posteroanterior [PA]): Right reticulomicronodular pattern and left lung cephalocaudal infiltrates; (B) Chest CT (axial plan [AP]): Bilateral micronodular opacities, right ground-glass opacities and extensive left consolidation areas; (C) Abdomen CT (coronal plan [CP]): Right retroperitoneal and retrocrural collection measuring 9×5.5cm, with inferior extension to L5 and bone destruction of the right lateral slope of D12; (D) Dorsolumbar spine MRI (sagittal plan [SP]): Signal heterogeneity suggestive of lytic and blastic lesions of D12 with cortical disruption, paravertebral soft tissue mass and enlargement of the psoas muscle; (E) Acid Fast Bacilli in the fluid drained from the psoas abscess, Ziehl-Neelsen.
The authors declare not having, real or perceived, direct or indirect conflicts of interest that relate to this article.


![(A) Chest X-ray (posteroanterior [PA]): Right reticulomicronodular pattern and left lung cephalocaudal infiltrates; (B) Chest CT (axial plan [AP]): Bilateral micronodular opacities, right ground-glass opacities and extensive left consolidation areas; (C) Abdomen CT (coronal plan [CP]): Right retroperitoneal and retrocrural collection measuring 9×5.5cm, with inferior extension to L5 and bone destruction of the right lateral slope of D12; (D) Dorsolumbar spine MRI (sagittal plan [SP]): Signal heterogeneity suggestive of lytic and blastic lesions of D12 with cortical disruption, paravertebral soft tissue mass and enlargement of the psoas muscle; (E) Acid Fast Bacilli in the fluid drained from the psoas abscess, Ziehl-Neelsen. (A) Chest X-ray (posteroanterior [PA]): Right reticulomicronodular pattern and left lung cephalocaudal infiltrates; (B) Chest CT (axial plan [AP]): Bilateral micronodular opacities, right ground-glass opacities and extensive left consolidation areas; (C) Abdomen CT (coronal plan [CP]): Right retroperitoneal and retrocrural collection measuring 9×5.5cm, with inferior extension to L5 and bone destruction of the right lateral slope of D12; (D) Dorsolumbar spine MRI (sagittal plan [SP]): Signal heterogeneity suggestive of lytic and blastic lesions of D12 with cortical disruption, paravertebral soft tissue mass and enlargement of the psoas muscle; (E) Acid Fast Bacilli in the fluid drained from the psoas abscess, Ziehl-Neelsen.](https://static.elsevier.es/multimedia/15792129/0000005700000005/v1_202104290903/S1579212921001294/v1_202104290903/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w98FxLWLw1xoW2PaQDYY7RZU=)







