Pneumonectomy may be needed in exceptional cases in patients with early stage NSCLC, especially in stage IB. The aim of this study was to evaluate whether overall survival in stage IB (T2aN0M0) NSCLC patients is worse after pneumonectomy.
MethodsRetrospective study of a series of pathological IB (pIB) patients who underwent either lobectomy or pneumonectomy between 2000 and 2011. The dependent variable was all-cause death. Operative mortality was excluded. The relationship between the age, FEV1%, Charlson index and performance of pneumonectomy variables and the dependent variable were analyzed using a Cox regression. Overall survival for both groups of patients was then plotted in Kaplan–Meier graphs and compared using the log-rank test.
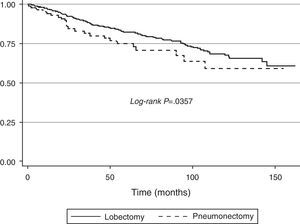
ResultsA total of 407 cases were analyzed (373 lobectomies and 34 pneumonectomies). According to Cox regression, age, FEV1% and pneumonectomy were associated with poorer survival (P<.05). Age-adjusted survival and FEV1% showed diminished survival in patients who underwent pneumonectomy (log-rank, P=.0357).
ConclusionsIn stage pIB NSCLC patients, pneumonectomy is associated with poorer survival compared to lobectomy.
La neumonectomía puede ser necesaria de forma excepcional en pacientes con cáncer de pulmón no microcítico (CPNM) en estadios precoces, algo más frecuentemente en el estadio IB. En este estudio se pretende evaluar si la neumonectomía se asocia con peor supervivencia global en pacientes con CPNM en estadios patológico IB (T2aN0M0).
MétodoEstudio retrospectivo sobre una población de pacientes con carcinoma de pulmón pIB sometidos a lobectomía pulmonar o neumonectomía entre 2000 y 2011. La variable dependiente es la muerte del paciente por cualquier causa, excluida la mortalidad operatoria. Mediante regresión de Cox se analizó la relación de las variables: edad del paciente, FEV1%, índice de Charlson y neumonectomía sobre la variable dependiente. Se elaboró un gráfico de Kaplan Meier en el que se representó la supervivencia de los pacientes con lobectomía o neumonectomía y se compararon las 2 funciones mediante la prueba log-rank.
ResultadosSe han analizado 407casos (373 lobectomías y 34 neumonectomías). En la regresión de Cox, la edad, el FEV1% y la neumonectomía se asociaron con una peor supervivencia (p<0,05). La función de supervivencia ajustada para edad y FEV1% demuestra menor supervivencia en los casos intervenidos mediante neumonectomía (log-rank p=0,0357).
ConclusionesEn los pacientes con estadio patológico IB la neumonectomía se asocia a una menor supervivencia comparada con la lobectomía.
According to the 7th edition of the TNM classification of lung cancer, stage IB includes tumors 3–5cm in diameter, with bronchial involvement 2cm or more distal to the carina, partial pulmonary atelectasis or invasion of the visceral pleura.1 The surgical approach, therefore, in many tumors classified at this stage will vary, depending on the operating field and the skill of the attending surgeon. In an earlier publication,2 we reported that 30-day mortality is a poor indicator of pneumonectomy risk, since death due to reasons other than cancer is much greater 6 months after the intervention than at 30 days. The hypothesis of this study is that, when all-cause mortality is taken into account, pneumonectomy in stage IB patients is associated with poorer survival.
MethodStudy PopulationA retrospective review was performed of patients undergoing pulmonary lobectomy or pneumonectomy for pathological stage IB (pIB) lung cancer in our hospital between January 2000 and December 2011. Information was retrieved from a prospective, computerized double entry database. To ensure maximum homogeneity, patients who had received induction chemotherapy were excluded, even if their definitive staging was pT1-2aN0M0, since in most cases indication for induction chemotherapy was based on a clinical classification of N2. Stage pIB patients who received adjuvant chemotherapy were included in the study, irrespective of the indication for chemotherapy.
Patient Screening CriteriaBefore surgery, all patients underwent the same tests: physical examination, complete blood count and serum biochemistry, electrocardiogram, chest X-ray, computed tomography (CT) of the chest and abdomen, and bronchoscopy. PET-CT was performed in all patients included since 2007. Invasive mediastinal staging (by mediastinoscopy or endobronchial ultrasound since 2009) was performed if mediastinal lymphadenopathies >1cm were seen on CT and if the mediastinal PET-CT was positive. All patients performed lung function tests; from 2009 onwards DLCO was routinely included.3 Cardiac risk was evaluated according to criteria previously published by our group.4 Patients with any neurological signs or symptoms on clinical examination underwent head CT, although this was not routinely ordered. Patients were classified for this study according to the TNM classification, 7th edition.1 Age was not a contraindication for patients with an indication for pneumonectomy who met screening criteria after individual discussion of the case by a multidisciplinary committee.
Perioperative Treatment and Follow-upThe surgical approach in all cases was muscle-sparing posterior thoracotomy, or either video-assisted or non-video-assisted axillary thoracotomy. The same group of anesthetists and thoracic surgeons were responsible for all anesthetic and surgical procedures, respectively. Systematic mediastinal lymphadenectomy was performed in all cases, based on current clinical guidelines.5 Antibiotic prophylaxis consisted of a single dose of 1500mg cefuroxime that could be repeated after 6h if surgery was prolonged. Patients were extubated before they left the operating room, and after a few hours in the reanimation unit were transferred to the thoracic surgery ward. Bupivacaine and fentanyl were administered as postoperative analgesia via a thoracic epidural catheter for the first 3 days. After catheter withdrawal, analgesia consisted of oral non-steroidal anti-inflammatories and paracetamol.
A single face-to-face visit was performed 1 month after surgery, and all other follow-up contact was made in the form of telephone calls to the patient or family members. If contact with the patient was lost, the date of death was retrieved from hospital records or treating physicians in the corresponding hospital.
Variables AnalyzedIndependent variables included were type of resection (pneumonectomy or other), patient age, preoperative FEV1%, and Charlson index.6 The latter was not recorded prospectively; instead, it was calculated retrospectively from variables recorded in the database that provided all the necessary variables. DLCO was only recorded routinely after 2009,3 so it was not included in the analysis. The dependent variable was all-cause death, excluding postoperative death (death within the first 30 days or any time before hospital discharge after the procedure).
Data AnalysisA Cox's regression model with bootstrap resampling with 100 replicates was used to examine associations between independent variables and survival. Age- and FEV1%-adjusted survival functions were constructed for patients undergoing pneumonectomy or lobectomy, and a log-rank test was performed to estimate the P-value of the differences between both functions. Data were analyzed using Stata/IC 13 software (StataCorp, Texas, USA).
ResultsA total of 407 patients (373 lobectomies and 34 pneumonectomies) were included in the study. Four patients died during surgery (0.98%; 1 pneumonectomy and 3 lobectomies).
At the time of starting this study, 212 patients had died; 195 (47.9%) remained alive. Causes of death were as follows: lung cancer, 112 cases; other cancer, 10; lung problems, 14; heart problems, 11; stroke, 6; other diseases, 12. In 47 cases (11.5%), cause of death was unknown.
Continuous variables are described in Table 1. Patients undergoing pneumonectomy were slightly younger than the lobectomized patients.
Cox's regression analysis (Table 2) shows that age, FEV1%, and undergoing pneumonectomy are associated with poorer survival. Age-adjusted survival function and FEV1% are shown in Fig. 1. P-Value in the log-rank test was .0357.
Perioperative mortality risk (death within 30 days of surgery) in pneumonectomy is still as high as 7%, almost 3-fold the risk of lobectomy.7 As we reported in a previous study,2 mortality of patients undergoing pneumonectomy even increases over time, and can reach 25% within 6 months of surgery in patients undergoing right pneumonectomy. This increase in mortality in our series was not associated with underlying cancer or bronchopleural fistula, but rather with a greater incidence of cardiorespiratory complications in pneumonectomized patients.
Despite these data, pneumonectomy is sometimes necessary in patients with stage IB non-small cell lung cancer (NSCLC), either because the surgeon lacks the technical skill to carry out parenchymal-sparing techniques, or because of the anatomical site of the tumor.
In the first situation, the number of pneumonectomies carried out in a surgical unit decreases as surgeons acquire expertise in bronchoplastic and angioplastic techniques.8 With regard to anatomical site, if proximal infiltration of the hilar structures or general extension across the lung fissure is observed, parenchymal-sparing techniques may be impossible. Even if lung fissure extension is not generalized and visceral pleural invasion is limited to a single point, several authors maintain that prognosis can be poorer in these patients.9–12 Some suggest that patients with T1 or T2 tumors with visceral pleural involvement crossing the interlobar fissure be classified as T3, or at least stage IIB (which comes down to the same), since survival is reduced by 10%–15% compared to patients with disease confined to a single lobe.12 The high number of patients undergoing pneumonectomy in the series published by Okada et al.10 and Demir et al.11 make their results difficult to interpret, since the intervention in itself may act as a confounding factor when determining survival. Nevertheless, the study by Joshi et al.,12 that includes only patients undergoing lobectomy plus wedge resection or bilobectomy, also reports poorer survival, typical of that between stages I and II, in patients with stage I NSCLC with interlobar extension. Taken together, the results of these studies suggest that both factors–fissure extension and pneumonectomy–play a fundamental role in the survival of these patients.
Unfortunately, fissure or hilar extension as a reason for indicating pneumonectomy was not included among our study variables; neither were the surgeon's technical reasons for performing lobectomy or pneumonectomy, nor the side in which pneumonectomy was performed. The influence of adjuvant treatments on survival was not analyzed. With regard to surgical risk factors, DLCO was only recorded in our series after 2009,3 so it could not be included as an independent variable in the regression model. Moreover, in 2002, an intensive postoperative respiratory physiotherapy protocol was introduced, leading to a significant reduction of respiratory complications.13 We did not adjust for this factor, which may have affected the study results.
Another limitation of this study is that the dependent variable is all-cause death; no differences were made between non-surgical causes, causes related with long-term complications derived from surgery and cancer-related causes. In our previous study,2 we found that oncological causes and bronchopleural fistula did not increase long-term mortality, while cardiorespiratory complications did. However, as we did not have the exact causes of the death of all of our patients in this series, these factors cannot be analyzed. Neither do we have data on the disease-free interval of patients with death due to tumor progression, and the information at our disposal was mostly obtained from telephone interviews. While, in our experience,14 this method is comparable to face-to-face patient interviews, it is impossible to guarantee the veracity of the information gathered.
To conclude, these data confirm that in pathological stage IB NSCLC patients, not only older age and lower FEV1% are associated with poorer survival after lung resection surgery, but prognosis is also compromised by pneumonectomy. Although it continues to be an effective intervention in the treatment of NSCLC in selected cases, care must be taken when indicating this procedure, taking account the individual surgical risk of each patient and the other treatment options available.
Conflict of InterestThe authors state that they have no conflict of interest.
Please cite this article as: Rodríguez M, Gómez Hernández MT, Novoa NM, Aranda JL, Jiménez MF, Varela G. La neumonectomía ofrece menor supervivencia a los pacientes con carcinoma de pulmón en estadio patológico IB. Arch Bronconeumol. 2015;51:223–226.