Several techniques have been described in recent years for the preoperative marking of pulmonary nodules under radiological guidance to assist resection by video-assisted thoracic surgery (VATS).1 One of these techniques is computed tomography (CT)-guided percutaneous marking of pulmonary nodules using low-radiation I-125 seeds. The seeds emit gamma radiation, so they can be detected intraoperatively using a gamma detection probe.2,3
We report a complication, not previously described, that occurred with this technique during the marking procedure. This complication, which we have called the “tent-pole effect”, occurred when it was impossible to cross the visceral pleural surface with the trocar (loaded with the radioactive seed), so the seeds were erroneously released into the pleural space. Nevertheless, the nodules were successfully removed by VATS and the seeds were recovered from the pleural cavity during surgery. This complication is described below in two patients with pulmonary nodules.
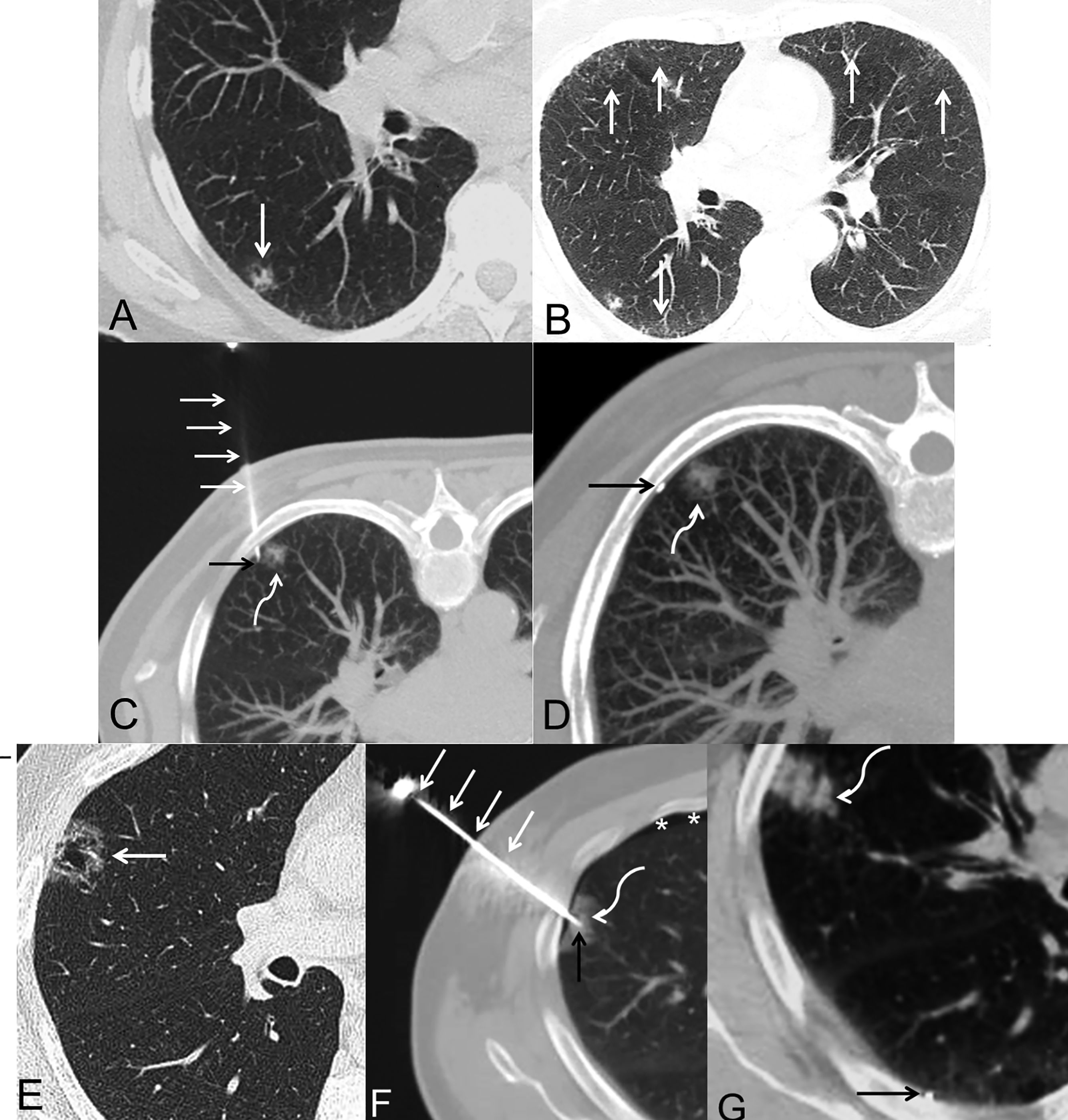
Patient 1 A 65-year-old woman, active smoker, with a mixed subpleural subsolid nodule in the right lower lobe (Fig. 1A). The patient had CT findings consistent with desquamative interstitial pneumonitis (Fig. 1B). Percutaneous marking of the pulmonary nodule was undertaken. Although it appeared during the marking procedure that the distal tip of the trocar was located in the pulmonary parenchyma (Fig. 1C), when the I-125 seed was released and the trocar was removed, the seed was observed in the pleural cavity (Fig. 1D). The patient underwent VATS surgery the following day, and a small hematoma was observed on the visceral pleural surface (caused by the puncture with the tip of the trocar) and an extended segmentectomy was performed.
Patients 1 (A–D) and 2 (E–G). All images correspond to axial CT slices of the chest (lung parenchyma window). A) Image showing a mixed subpleural subsolid nodule (arrow) in the right lower lobe. B) Image identifying several bilateral subpleural ground glass attenuation opacities (arrows) consistent with a pattern of desquamative interstitial pneumonitis. C) Image with the patient in prone position, showing the trocar (straight white arrows) penetrating the chest wall, the distal tip of the trocar apparently in an intrapulmonary location (black arrow), and the pulmonary nodule (curved white arrow). D) Image with patient prone after trocar removal identifying extrapulmonary location of I-125 seed (black arrow), and the pulmonary nodule (curved white arrow). E) Image showing a mixed subpleural subsolid nodule (arrow) in the right upper lobe. F) Image showing the trocar (straight white arrows) penetrating the chest wall, the distal tip of the trocar apparently in an intrapulmonary location (black arrow), and the pulmonary nodule (curved white arrow). Note the appearance of a small laminar pneumothorax (asterisks). D) Image after trocar removal identifying extrapulmonary location of the I-125 seed (black arrow) and subpleural hemorrhage (curved white arrow).
Patient 2 A 58-year-old male, former smoker, with a subpleural subsolid nodule and areas of cavitation in the right upper lobe (Fig. 1E). As in the previous case, the impression during the marking procedure was that the distal tip of the trocar was located within the pulmonary parenchyma (Fig. 1F), but when it was checked, the seed was observed in the pleural cavity (Fig. 1G). The patient underwent VATS surgery the following day, and a small hematoma was also identified in the visceral pleura that helped the surgeon safely and completely resect the pulmonary nodule (segmentectomy).
The definitive histological diagnosis in both patients was infiltrating adenocarcinoma (pT1b).
The demand for resection of pulmonary nodules is increasing due to the growing indication for pulmonary metastasectomies4 and improved detection of suspected nodules in lung cancer screening programs with low-dose CT of the chest.5 However, the small size or scant solid component of these nodules mean that they may be difficult for the chest surgeon to identify intraoperatively. In these cases, preoperative marking helps ensure complete and safe resection of pulmonary nodules.6 Multiple preoperative pulmonary marking techniques are available7; the main advantages of our technique lie in the reduced ability of the seed to mobilize after intrapulmonary release and the possibility of scheduling surgery days or weeks after the marking procedure.2
The procedure consists of percutaneous insertion of I-125 radioactive seeds via a trocar (18G in our center) from which the central stylet has been removed. Before inserting the trocar into the patient, the seed is introduced into the trocar and sealed with a small amount of bone wax to prevent the seed from coming out of the distal tip. Once the trocar is loaded, it is inserted into the patient through a small skin incision. After checking the correct position of the distal tip of the trocar within the pulmonary nodule to be resected, the stylet (which has a sharp tip) is then inserted through the trocar to push the seed and release it into the pulmonary parenchyma. Some complications associated with this marking technique have been described, including pneumothorax, pulmonary hemorrhage, and seed migration. However, the “tent-pole effect” complication has not been described previously. It occurs when the trocar fails to puncture the visceral pleura, in such a way that its distal tip pushes against or repels the visceral pleura (in a similar way to a tent pole) without perforating it. In CT images (during the marking procedure), an optical effect occurs in which it appears that the trocar has crossed the visceral pleura and that its distal tip is located within the lung, but in fact it has not perforated the visceral pleura. We believe that this complication may be due to several factors: 1) reduced perforating capacity of the beveled tip of the trocar (when introduced into the chest without the central stylet which acts as a needle with greater perforating capacity); 2) the “slippery” effect of the bone wax (on the visceral pleural surface) used to seal the trocar; 3) subpleural localization of the nodules, which offer some resistance to the trocar, making them difficult to penetrate; and 4) presence of subpleural interstitial lung disease in one of the patients (we believe that areas of subpleural inflammation might have made it difficult to puncture the visceral pleura). We also believe that this complication can be reduced by minimizing the amount of bone wax applied at the distal tip of the trocar and attempting to release the seed close to the deep margin (further away from the visceral pleura) of the pulmonary nodule (avoiding its release near the subpleural space). We also recommend that surgery be expedited if this complication occurs, as there is likely to be a small hematoma “tattooed” on the visceral pleural surface that may facilitate resection of the pulmonary nodule.
Despite this complication, the nodules of both patients were successfully removed by VATS and the I-125 seeds were recovered from the pleural cavity during surgery. In our opinion, the description of this unprecedented complication can improve the selection of patients and anticipate this setback in patients with the characteristics listed above.
Please cite this article as: Ajuria-Illarramendi O, Gorospe Sarasúa L, Fra-Fernández S, Rioja-Martín ME, Ureña-Vacas A, Mirambeaux-Villanova RM, et al. Efecto «tienda de campaña»: una complicación no descrita del marcaje percutáneo de nódulos pulmonares con semillas de I-125. Arch Bronconeumol. 2020. https://doi.org/10.1016/j.arbres.2020.06.018