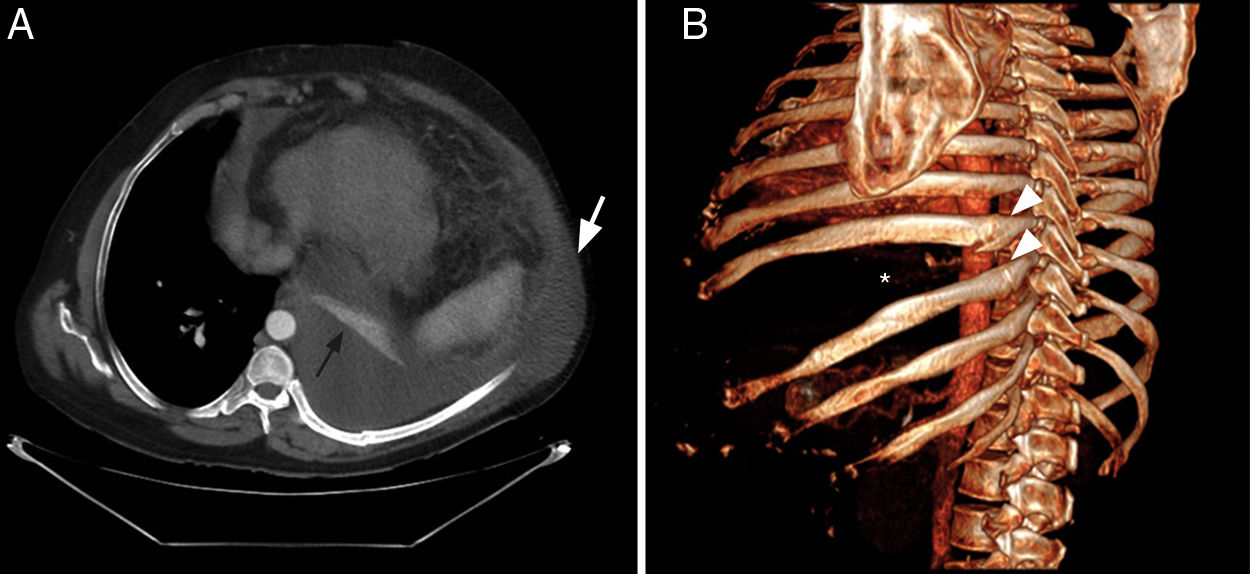
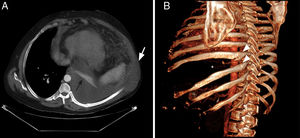
A 60-year-old patient with a history of liver cirrhosis and recurrent hydrothorax consulted for the sudden appearance of a chest wall mass after severe fit of coughing. A mass that oscillated with respiratory movements was visible in the left lateral and posterior chest wall. Ultrasound revealed signs of chronic liver disease, predominantly left-sided pleural effusion with fluid outside the chest cavity, and moderate ascites. Chest computed tomography (CT) showed a recent fracture of the 8th and 9th left rib with ipsilateral pleural effusion and herniation of the pleural effusion through the intercostal space, dissecting muscular planes, located in the subcutaneous cell tissue (Fig. 1A and B). The wall defect was repaired and the rib fractures were reduced with osteosynthesis material.
A) Chest CT (axial view) showing herniation of left pleural effusion to the adjacent subcutaneous region (white arrow). Note complete atelectasis of the left lower lobe (black arrow). B) Three-dimensional CT reconstruction (left posterior oblique projection), showing fractures in the posteromedial region (arrowhead) of 2 contiguous ribs (8th and 9th) and significant widening of the eighth intercostal space (asterisk).
Intercostal hernias are associated with trauma or previous thoracic surgery.1 The hernial sac contains lung and pleural tissue, and isolated herniation of pleural fluid is exceptional. Herniation was caused by a sharp increase in intrathoracic pressure causing rib fractures. The wall defect was repaired and the fracture reduced with osteosynthesis material.2
Please cite this article as: Martín-Jiménez A, García-Gil D, Manuel Porcel J. Herniación pleuro-pulmonar como causa de tumoración en la pared torácica de inicio brusco. Arch Bronconeumol. 2020. https://doi.org/10.1016/j.arbres.2019.10.004