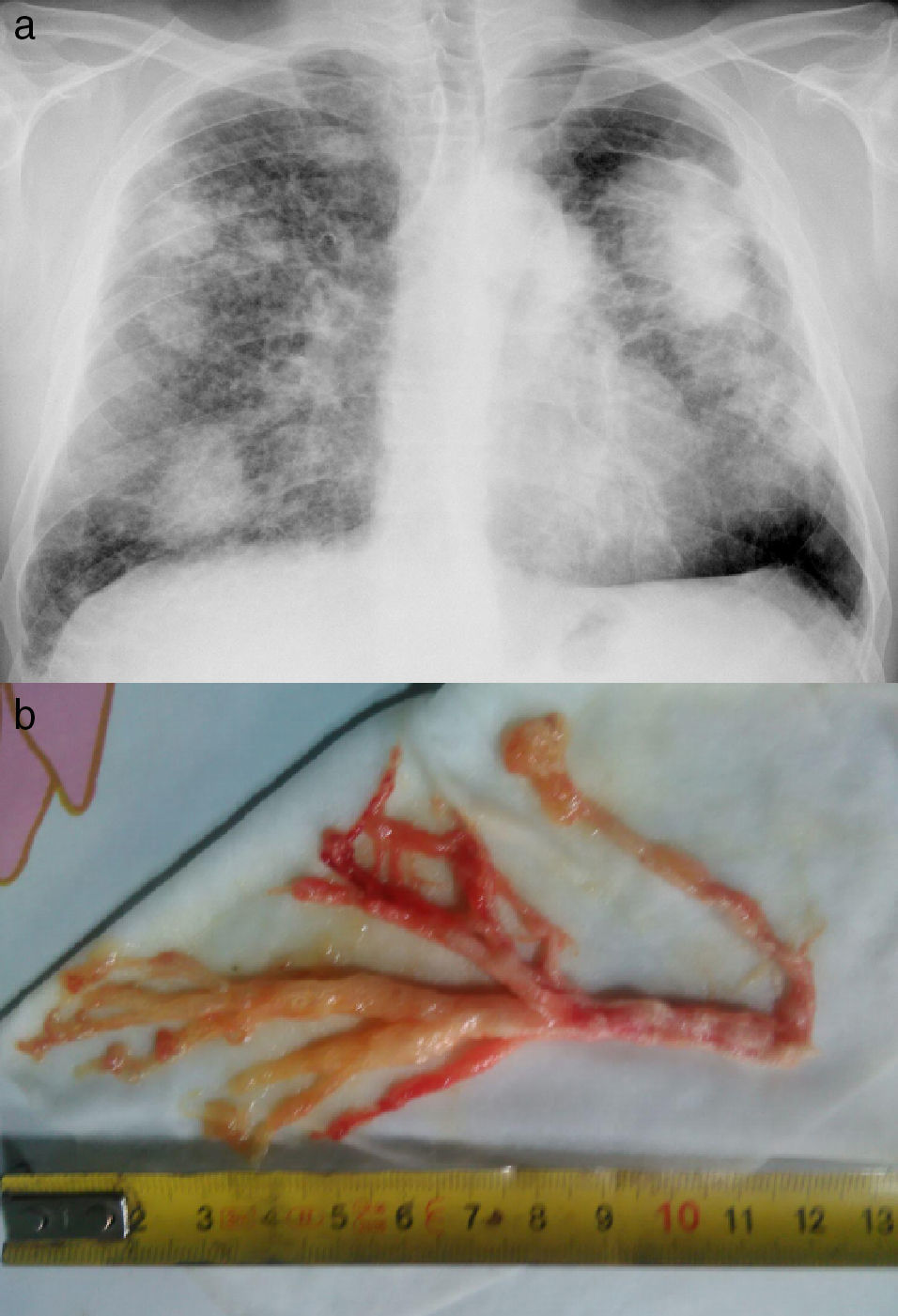
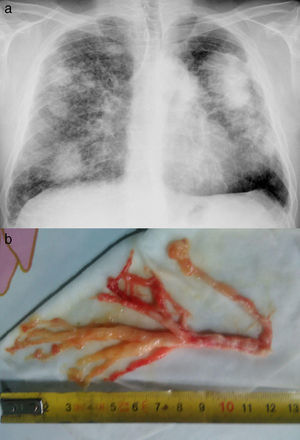
We report the case of a 49-year-old man with complicated silicosis and a history of pulmonary tuberculosis, non-smoker, with obstructive airflow limitation. He consulted due to episodes of intense dyspnea coinciding with expectoration of thick bloody secretions with a similar appearance to the bronchial tree (Fig. 1), occurring several days a week. The fiberoptic bronchoscopy showed no relevant findings and the pathology study of the bronchial cast revealed fibrinoinflammatory mucoid material, with abundant histiocytes.
Plastic bronchitis (PB) is a rare lung disease characterized by the formation and expectoration of bronchial casts that obstruct the bronchial lumen.1 It has been described as a complication of primary lymphatic abnormalities in patients with congenital heart disease (after the Fontan procedure), respiratory infections, cystic fibrosis, COPD, and allergic bronchopulmonary aspergillosis.1 We report a case of PB associated with silicosis. Treatment is controversial and therapeutic choices, which are based on isolated case reports, include mainly dornase alfa, low-dose macrolides, and nebulized hypertonic saline and acetylcysteine. Response to inhalation of fibrinolytics and nebulized heparin has been reported.1,2 In our patient, episodes of mucus plug expulsion reduced notably with the administration of prednisone (15mg/day) and nebulized heparin sodium (5000IU/12h).
Please cite this article as: Blanco Pérez JJ, Arnalich Montiel V, Guerra Vales JL. Bronquitis plástica en un paciente con silicosis. Arch Bronconeumol. 2017;53:516.