While the benefits of pulmonary rehabilitation programs (PR) in COPD have been demonstrated, poor adherence, related with worse clinical outcomes, is common.
ObjectiveThe purpose of this study was to examine causes for drop-out during a 12-week multidisciplinary pulmonary rehabilitation program and to investigate the characteristics of patients with poor adherence, with special emphasis on functional and clinical characteristics.
MethodA prospective study was performed between February and November 2015 in 83 COPD patients enrolled in an outpatient program of 36 strength+resistance training sessions. Ambulances were provided to facilitate access to the clinic. Patients were divided into: adherent (A) (attended at least 70% of the program) or non-adherent (NA) (at least one session).
ResultsA total of 83 patients were evaluated and 26 excluded; 15.7% refused to participate. The drop-out rate was 38.5%. The main causes were low motivation and transport problems. Lower forced vital capacity (NA, 58.9% vs A, 67.8%; P=.03), worse results on submaximal exercise test (NA, 6.2min vs A, 9.2min; P=.02), in total distance walked (NA, 42.6 vs A, 56.5; P=.03) and VO2 in ml/min/kg (NA, 11.4 vs A, 13.6; P=.03) and in ml/min (NA, 839 vs A, 1020; P=.04) were found in the non-adherent group. This group also showed higher use of oral steroids (NA, 23.8% vs A, 2.9%; P=.01).
ConclusionsMore than 1/3 of patients leave programs. The main causes are related to motivation and transport. The patients who dropout are those with worse functional tests, more exacerbations, steroids and smoking habit.
Aunque los beneficios de los programas de rehabilitación respiratoria (RR) en pacientes EPOC han sido demostrados, la adherencia es baja, relacionándose con peores resultados.
ObjetivoIdentificar las causas de abandono de un programa de RR para EPOC y las características de los pacientes con mala adherencia, haciendo especial énfasis en características funcionales y clínicas.
MétodoEstudio prospectivo en 83 EPOC desde febrero a noviembre de 2015. Se realizó un programa mixto (fuerza y resistencia) ambulatorio de 36 sesiones. Se facilitó la accesibilidad con ambulancias. Los pacientes fueron divididos en adherentes (acudieron al menos al 70% del programa) o no adherentes (al menos a una sesión).
ResultadosSe evaluaron 83 pacientes, de los que 26 fueron excluidos. Un 15,7% rehusó participar. La tasa de abandono fue del 38,5%. Las principales causas fueron tener baja motivación para acudir al gimnasio y problemas de trasporte. El grupo que abandonó el programa presentó una menor capacidad vital forzada (abandonan 58,9% vs completan 67,8%; p=0,03), peores resultados en el test de esfuerzo submáximo (abandonan 6,2min vs completan 9,2min; p=0,02), en W totales (abandonan 42,6 vs completan 56,5; p=0,03) y en VO2, tanto en ml/min/kg (abandonan 11,4 vs completan 13,6; p=0,03) como en ml/min (abandonan 839 vs completan 1.020; p=0,04). Este grupo también presentó mayor uso de esteroides orales (abandonan 23,8% vs completan 2,9%; p=0,01).
ConclusionesMás de 1/3 de los pacientes abandonan los programas. Las causas principales son relativas a la motivación y el transporte. El perfil de paciente que abandona presenta peores pruebas funcionales, más exacerbaciones, uso de esteroides y tabaquismo.
Respiratory rehabilitation is currently defined by the American Thoracic Society/European Respiratory Society (ATS/ERS) as “a comprehensive intervention based on a thorough patient assessment followed by patient-tailored therapies that include, but are not limited to, exercise training, education, and behavior change, designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long-term adherence to health-enhancing behaviors”.1 Although the benefits of respiratory rehabilitation programs in patients with chronic obstructive pulmonary disease (COPD) on dyspnea, health-related quality of life and exercise capacity have been widely established,2 patients must be carefully selected if the best results are to be obtained.3 However, despite appropriate patient selection and a multidisciplinary approach to treatment, adherence to rehabilitation programs varies widely, with reports in the literature of substantial drop-out rates and poor attendance (between 10% and 32%)4; these circumstances have been linked with poor clinical outcomes. Several reasons for dropping out of rehabilitation programs have been identified, some of the most important being ongoing comorbidities, transport problems, no perception of improvement, lack of family support, depression, smoking, etc.4–8 Evidence suggests that even the attitude of the doctor when explaining the need to join programs could improve adherence.9 However, the variables that might predict poorer compliance with respiratory rehabilitation programs have not been fully defined, and even the definition of adherence differs between studies, with some authors including patients who refuse to participate after being offered a program among non-adherents.8 In the papers cited, less information is provided on functional characteristics, including maximal and submaximal exercise tests, and certain clinical features, such as use of concomitant medication or specific respiratory therapies. The objectives of our study were to identify the main causes of drop-out from a specific COPD respiratory rehabilitation program, along with the characteristics of patients with poor adherence, focusing particularly on specific clinical and functional aspects.
Patients and MethodPatientsThis was a prospective study performed in 83 COPD patients in the Respiratory Medicine Department of Hospital Virgen Macarena (Seville), enrolled in a specific respiratory rehabilitation program between February and November 2015. STROBE recommendations for observational studies were followed. Criteria for inclusion included a diagnosis of COPD according to spirometry (any stage of severity), smoking history, and symptoms despite optimal treatment. Exclusion criteria were presence of psychiatric or behavioral disorders that would hinder collaboration in the program, musculoskeletal disease incompatible with exercise training, and acute cardiovascular disease.
Patients were divided into 2 groups: adherent or non-adherent. Patients were considered adherent if they attended at least 70% of scheduled sessions, guaranteeing at least 8 weeks’ compliance and beneficial effects on health. Drop-outs (non-adherents) were patients who attended at least 1 program session but less than 70% of the total sessions. Patients who refused to participate in the program after it was offered were excluded from the study.
Type of ProgramThe outpatient respiratory rehabilitation program consisted of 36 sessions, requiring attendance at the hospital 3 times a week. Sessions consisted of 10min of warm-up exercises and respiratory physiotherapy, followed by 20min of lower limb resistance training on a static bicycle set at 70% of the peak work rate recorded in a previous maximal exercise test, and 2 series of 6–8 repetitions of each exercise at 75% of the maximum achieved in 1 repetition (1MR) test. The strength training program included several exercises: (1) chest pull (to strengthen the latissimus dorsi muscle); (2) butterfly (pectoralis major muscle); (3) neck press (triceps brachii and deltoids); (4) leg flexions (biceps femoris), and (5) leg extensions (quadriceps femoris).10 This was complemented with educational talks at the beginning and the end of the program, explaining different aspects of the disease, correct inhaler techniques, dietary recommendations, self-management of the disease, and recommendations on physical activity at home. Oxygen supplements were provided during the exercise sessions for all patients who were receiving home oxygen therapy. Ambulances were provided for transport to the hospital, if necessary.
VariablesData were collected on demographics (age, sex, body mass index [BMI]), smoking history, dyspnea grade according to the modified Medical Research Council (MRC) scale, COPD severity according to GOLD 2009,11 comorbidities, visits to the emergency room in the past year, and concomitant medications, including the use of non-invasive mechanical ventilation (NIMV). A comprehensive evaluation of lung function parameters was conducted: forced vital capacity (FVC) and forced expiratory volume in 1s (FEV1) according to spirometry performed using a Jaeger Viasys Mastercope spirometer,12 6-min walk test (6MWT) performed according to ATS recommendations13 in a 30-m corridor, maximal exercise test with a cycle ergometer using an incremental exercise protocol,14 cycle ergometer submaximal exercise test at 80% maximal work rate obtained in the maximal exercise test and the 1MR test, for evaluation of muscle strength. Quality of life questionnaires were also administered to both groups: St. George's specific respiratory disease questionnaire,15 the CRQ,16 and the Hospital Anxiety and Depression (HADS) questionnaire.17
Finally, the reasons which led patients to drop out of the program were recorded.
Statistical AnalysisThe statistical analysis was performed using the SPSS statistical package for Windows (SPSS v22 [2013], Chicago, IL, USA). After normal distribution was ascertained, values were expressed as mean±standard deviation for quantitative variables or percentage for qualitative variables. Comparisons between adherent and non-adherent patients were performed using the Chi-squared test for categorical variables and the Student t-test for continuous variables. The minimal level of significance in all cases was taken as P<.05.
Ethical AspectsThis study was reviewed and approved by the Clinical Research Ethics Committee of the Hospital Virgen Macarena in Seville. All participants were informed about the nature of the study and its objectives, and agreed to participate by signing an informed consent form. Data were obtained under conditions of strict confidentiality in accordance with Spanish Personal Data Act 15/1999.
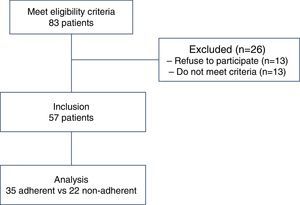
ResultsA total of 83 patients were evaluated, of which 26 were excluded: 13 (15.7%) refused to participate in the program, and the other 13 failed to meet inclusion criteria. Of those who did not meet the inclusion criteria, the causes recorded were: unstable angina (1 patient), mental disease (2 patients), severe musculoskeletal disease (2 patients), few symptoms (3 patient), did not attend evaluations (5 patients). Finally, 57 patients were included, of whom 35 completed the program and 22 dropped out (Fig. 1).
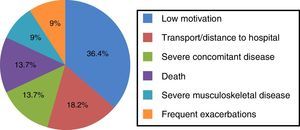
Reasons for Drop-OutThe drop-out rate from our program was 38.5%. The main causes recorded were lack of motivation (8 patients), transport problems due to distance from the hospital/travel time (4 patients), severe concomitant disease (3 patients), death (3 patients), severe orthopedic disease preventing continuation (2 patients), and frequent exacerbations (2 patients) (Fig. 2).
Demographic and Clinical CharacteristicsMost patients in both program groups were men in their sixties. Although there was a higher percentage of former smokers in the group that completed the program (80% vs 68.2%), and tobacco use was lower, the differences were not significant. No differences were found in comorbidities, and both groups had a mean of more than 2 exacerbations per year, with more than twice the number of exacerbations observed among drop-outs, although this trend was not significant. Another trend, also non-significant, toward poorer dyspnea scores was seen among drop-outs (Table 1).
Demographic and Clinical Characteristics and Comparison Between Patients who Completed or did not Complete the Respiratory Rehabilitation Program.
| Characteristics | Did not complete (n=22) | Completed (n=35) | Significance (P) |
|---|---|---|---|
| Sex (% men) | 90.90 | 88.63 | .78 |
| Age (years) | 67.22±8.21 | 65.10±9 | .38 |
| Former smoker | 68.24 | 80 | .32 |
| Tobacco consumption (pack-years) | 76.8±33 | 63.71±30 | .13 |
| AHT | 54.53 | 57.13 | .85 |
| DL | 22.72 | 17.15 | .60 |
| DM | 36.43 | 17.14 | .10 |
| Ischemic HD | 4.57 | 8.64 | .56 |
| CHF | 9.12 | 20 | .27 |
| GOLD stage | |||
| II | 9.05 | 11.75 | .92 |
| III | 27.30 | 29.45 | |
| IV | 63.65 | 58.80 | .55 |
| MRC dyspneaa | |||
| 0–2 | 31.80 | 41.70 | |
| 3–4 | 68.20 | 58.30 | |
| Exacerbation/previous year | 4.3±4.32 | 2.6±2.62 | .08 |
| BMI (kg/m2) | 27±3.73 | 28±4.54 | .38 |
Qualitative variables expressed as percentage. Quantitative variables expressed as mean and standard deviation. A P-value of <.05 was considered statistically significant.
AHT, arterial hypertension; BMI, body mass index; CHF, chronic heart failure; DL, dyslipidemia; DM, diabetes mellitus; HD, heart disease; MRC, Medical Research Council.
The main findings were a lower percentage FVC (58.9% in non-adherents vs 67.8% in adherents; P=.03), poorer results in the submaximal exercise test (6.2min in non-adherents vs 9.2min in adherents; P=.02), in maximal workload achieved (W) (42.6 in non-adherents vs 56.5 in adherents; P=.03), and in oxygen consumption, both ml/min/kg (11.4 non-adherents vs 13.6 adherents; P=.03) and ml/min (839 non-adherents vs 1020 adherents; P=.04) among the program drop-outs. With regard to medication, a greater percentage of patients of those who dropped out the program were receiving oral corticosteroids (23.8% non-adherents vs 2.9% adherents; P=.01), despite the controversies surrounding the use of this medication in stable patients. More than twice as many of the adherent group were receiving non-invasive ventilation devices (NMVI, BiPAP) compared to the non-adherent group (13.6 vs 22.9), but the difference was not significant. No significant differences were found in the other parameters evaluated (Table 2).
Functional Assessment and Use of Treatments and Comparison Between Patients who Completed or did not Complete the Respiratory Rehabilitation Program.
| Characteristics | Did not complete (n=22) | Completed (n=35) | Significance (P) |
|---|---|---|---|
| Lung function tests | |||
| FEV1 (cc) | 1013±361 | 1198±450 | .10 |
| FEV1 (%) | 37.71±13.50 | 42.22±10.51 | .16 |
| FVC (cc) | 2118±697 | 2480±711 | .06 |
| FVC (%) | 58.91±16.71 | 67.82±13.31 | .03 |
| FEV1/FVC | 48.43±14 | 47.82±7.51 | .85 |
| Diffusing capacity (DLCO) (%) | 39.49±18.91 | 47.92±21 | .26 |
| Corrected DCLO (%) | 56.44±25.68 | 63.12±30 | .19 |
| 6MWT (m) | 358±113 | 381±155 | .58 |
| Submaximal test (min) | 6.22±2.13 | 9.25±4.67 | .02 |
| Maximal exercise test | |||
| Maximum work rate (w) | 42.61±17.82 | 56.49±22.72 | .03 |
| Maximum work rate (%) | 37.41±13.43 | 44±16.82 | .15 |
| Maximum VO2 (ml/min/kg) | 11.42±2.83 | 13.66±3.67 | .03 |
| Maximum VO2 (ml/min) | 839±201 | 1020±338 | .04 |
| Maximum VO2 (%) | 48.21±10.50 | 55.60±15 | .07 |
| 1MR test | |||
| Chest pull (kg) | 25.71±7.91 | 27.82±9.63 | .93 |
| Butterfly (kg) | 16.38±6.43 | 16.11±7.81 | .72 |
| Leg flexion (kg) | 10.39±4.12 | 15.12±8.13 | .25 |
| Leg extension (kg) | 22.93±10.61 | 24.42±8.91 | .57 |
| Elbow flexion-extension (kg) | 10.43±5 | 9.32±4.23 | .36 |
| SABA | 45.50 | 48.61 | .82 |
| LABA | 9.13 | 0 | .07 |
| LAMA | 90.91 | 94.32 | .63 |
| LABA+ICS | 68.23 | 54.33 | .29 |
| Theophyllines | 0 | 2.43 | .43 |
| BiPAP | 13.61 | 22.92 | .39 |
| Home oxygen therapy | 59.10 | 54.32 | .72 |
| Systemic corticosteroids (%) | 23.80 | 2.90 | .01 |
BiPAP, bilevel positive air pressure; ICS, inhaled corticosteroids; LABA, long action beta agonist; LAMA, long action muscarinic agonist; SABA, short action beta agonist.
Qualitative variables expressed as percentage. Quantitative variables expressed as mean and standard deviation. A P-value of <0.05 was considered statistically significant.
No differences were found between the groups in any of the specific respiratory disease questionnaires administered, either in overall score or in any of the separate dimensions. Nor were differences found for anxiety and depression (Table 3).
Total Scores Obtained From Quality of Life Questionnaires and Comparison Between Patients who Completed or did not Complete the Respiratory Rehabilitation Program.
| Characteristics | Did not complete (n=22) | Completed (n=35) | Significance (P) |
|---|---|---|---|
| Anxiety (HADS) | 5±4.10 | 5.72±4.13 | .56 |
| Depression (HADS) | 5.23±3.61 | 4.71±4.40 | .71 |
| CRQ (total points) | 79±24.50 | 86±23 | .28 |
| Dyspnea | 11.63±5.60 | 12.41±4.13 | .50 |
| Fatigue | 16.73±5.10 | 18.09±6.10 | .39 |
| Emotional function | 33.33±11.20 | 34.32±10.61 | .49 |
| Disease control | 18.31±6.22 | 20.83±6.50 | .16 |
| St George's (total points) | 58.50±18 | 52.41±16.39 | .19 |
| Symptoms | 61.48±22.37 | 57.81±20 | .50 |
| Activity | 75.61±20.40 | 69.72±18.90 | .28 |
| Impact | 47.91±19.12 | 40.80±17.63 | .16 |
| CAT | 19.42±11 | 19.81±7 | .93 |
CAT, COPD Assessment Test; CRQ, Chronic Respiratory Disease Questionnaire; HADS, Hospital Anxiety and Depression Scale.
Qualitative variables expressed as percentage. Quantitative variables expressed as mean and standard deviation. A P-value of <.05 was considered statistically significant.
Our study, aimed at characterizing non-adherent patients in a respiratory rehabilitation program, found that drop-outs presented more exacerbations, greater forced vital capacity (probably indicating increased air trapping), and worse results on exercise tests; generally, then, patients with a more severe profile.
Respiratory rehabilitation is an evidence-based treatment with clear benefits that should be offered to all COPD patients, irrespective of their severity grade. However, we are aware that the success of rehabilitation programs is largely dependent on the correct selection of patients, but the patients evaluated often do not meet the eligibility criteria or refuse to participate. In our study, almost 16% of patients refused to participate in the program, and the drop-out rate was high (38.5%), but close to that described in the literature.5,8 In a similar study to ours,8 around 40% of patients did not complete the program, although the definition of non-adherence included patients who refused to participate (the majority), as well as those who dropped out after starting. Although this latter group was much smaller than ours (6 patients), the short program duration (4 weeks) may have had an impact, particularly if we take into account that in our study, attendance for at least 8 weeks was required.
The reasons for dropping out of the program varied, although lack of motivation and transport problems or distance from the site were the most common,4,8,18 even though an ambulance service was provided to facilitate transport to the hospital.
With respect to the demographic and clinical characteristics, most studies4,7,8,19,20 have reported active smoking as a determinant factor for poor adherence. In our case, although non-adherents smoked more, the difference was not significant, and was probably associated with the sample size. Another consideration, also described in the literature, is that attending a rehabilitation program may indicate a greater inclination to stop smoking.20
A trend toward a higher dyspnea grade among non-adherents was also observed, which might explain the loss of motivation if the patient feels more poorly or more limited in their exercise capacity. Hogg et al.6 reported similar findings in a study in which patients with higher MRC dyspnea grade had significantly poorer adherence. Moreover, FVC, which might cause greater air trapping resulting in dynamic hyperinflation and limited exercise capacity, was significantly worse in patients who dropped out of the program. This may also be associated with the presence of a larger proportion of patients on NIMV in the adherent group, since some evidence suggests that NIMV in stable COPD patients improves pulmonary hyperinflation and may allow the patient to achieve more intense exercise levels, suggesting that this intervention is beneficial not only during sleep, but also as an aid to rehabilitation.1,21 It should be pointed out that the criterion for indicating NIMV was the same in all cases (according to the consensus recommendations), and that it was indicated after hospital admission for hypercapnic encephalopathy. Moreover, none of the patients had concomitant neuromuscular disease or rib cage abnormalities.
In general, patients who drop out of the program appear to be those with greater functional decline (worse results on exercise tests) and use of oral corticosteroids. Few studies have evaluated so many functional parameters, particularly cardiopulmonary exercise tests, so closely. Fisher et al.,22 in a 12-weeek study evaluating cardiopulmonary exercise tests, failed to identify any demographic, clinical or psychological factors that could predict drop-out. Similar results were reported by other groups.4,8,23 Hayton et al.,24 however, support our results; these authors suggested, on the basis of a shuttle walking test, that patients who drop out of rehabilitation programs may have poorer exercise tolerance.
With regard to medication, one study8 did not find any association with the occasional use of cycles of oral corticosteroids. In our experience, the use of oral corticosteroids might reflect the fact that non-adherents were patients with more severe and advanced disease, and with higher exacerbation rates (more than double that of the other group), with the subsequent negative effect on program adherence. The side effects of steroids, such as osteoporosis and myopathies, would also have a negative impact on the physical activity of these patients.
Like other authors, such as Young et al.8 or Fan et al.,25 we found no relationship between quality of life, anxiety and depression, and lack of adherence. However, our results conflict with those of other studies which reported that lack of adherence was associated with depression,4,5 psychological profile,26 or worse scores on the St. George's questionnaire.5 In this respect, it should be pointed out that one of the benefits of rehabilitation is improved levels of anxiety and depression, common comorbidities among COPD patients.27
One of the limitations of our study is the sample size, which may have prevented factors with a trend toward significance from becoming statistically significant or unsuspected differences from emerging. The mean age of the patients is rather high, and most have severe or very severe COPD, so this population could be more inflexible in terms of behavior and beliefs, and find it more difficult to adopt lifestyle changes and modification of habits. Additionally, the fact that most patients are men may limit the generalization of results, but while the latest studies in COPD are already showing increased proportions of women, perhaps these changes are not yet so obvious in populations of older patients seen in our clinics. However, this is a study performed under standard clinical practice conditions (elderly patients with advanced disease), and clearly reflects the population that might be encountered in a respiratory rehabilitation clinic. It may be of great importance to remind all healthcare professionals that respiratory rehabilitation has proven benefits, and that it should be implemented when the disease is in its early stages, particularly if we understand that a poorer functional status may be associated with poorer adherence rates.
In conclusion, low adherence to rehabilitation programs appears to be associated not only with motivation or distance from the hospital, but also with a specific patient profile. This group, who we found to present the most severe disease (worse functional tests, chronic users of oral corticosteroids, higher rates of exacerbations and smoking), needs special attention and a more individualized approach. It would also be of interest to implement strategies to help motivate not only patients who join the program but also those who are unwilling to even start. Larger studies are needed to identify predictive factors for low adherence and to introduce effective strategies to promote compliance.
Authorship- -
Planning and preparation of the research project: Teodoro Montemayor Rubio.
- -
Design and data collection: Virginia Almadana Pacheco, Ana Gómez-Bastero Fernández, Ana Mirian Muñiz Rodríguez, Rodrigo Tallón Moreno.
- -
Analysis and presentation of results: Virginia Almadana Pacheco, María Pavón Masa.
The authors state that they have no conflict of interest.
Please cite this article as: Pacheco VA, Masa MP, Fernández APGB, Rodríguez AMM, Moreno RT, Rubio TM. Perfil de pacientes que abandonan un programa de rehabilitación respiratoria. Arch Bronconeumol. 2017;53:257–262.