Interstitial lung diseases (ILD) and, in particular, idiopathic pulmonary fibrosis, may have a significant impact on patient survival. Recent studies highlight the need for palliative care (PC) in the management of ILD patients. The aim of this study was to determine the current situation of PC in patients in Spain.
MethodsA 36-question survey addressing the main aspects of PC in ILD patients was designed. The survey was sent via email to all members of the Spanish Society of Pulmonology and Thoracic Surgery. Participation was voluntary.
ResultsOne hundred and sixty-four participants responded to the survey. Ninety-eight percent said they were interested in PC, 46% had received specific training, and 44% reported being responsible for PC in their ILD patients. Symptom control and end-of-life stage were the most frequent reasons for referral to PC teams. Regarding end-of-life, 78% reported consensual agreement with patients on the limitation of therapeutic efforts, 35% helped prepare an end-of-life advance directive, and 22% agreed on the place of death.
ConclusionDespite the well-known need for PC in patients with ILD and the notable interest of the survey participants in this subject, there are clear formative and organizational gaps that should be addressed to improve care in this area in ILD patients in Spain.
Las enfermedades pulmonares intersticiales difusas (EPID) y, concretamente, la fibrosis pulmonar idiopática, pueden tener un elevado impacto en la supervivencia de los pacientes. Recientes estudios destacan la necesidad de implementar los cuidados paliativos (CP) en el manejo del enfermo con EPID. El objetivo del estudio fue conocer la situación actual de los CP en nuestro país.
MétodosSe diseñó una encuesta de 36 preguntas, que abordaba los principales aspectos de los CP en el paciente con EPID. Esta encuesta fue remitida a través de correo electrónico a todos los miembros de la Sociedad Española de Neumología y Cirugía Torácica, cuya participación fue voluntaria.
ResultadosCientosesenta y cuatro participantes respondieron a la encuesta. El 98% manifestó tener interés en los CP, 46% habían recibido formación específica. El 44% refirió ser el responsable de los CP en sus pacientes EPID. El control de síntomas y la fase final de vida fueron los motivos más frecuentes de derivación a los equipos de CP. Referente a la fase final de vida el 78% refirió consensuar con los pacientes la limitación del esfuerzo terapéutico, el 35% realizar un documento de voluntades anticipadas y el 22% consensuar el lugar de fallecimiento.
ConclusiónA pesar de la conocida necesidad del CP en los pacientes con EPID y el notable interés de los participantes de la encuesta en este tema, existen claras lagunas formativas y organizativas, que deberían ser contempladas para mejorar la atención sobre esta área de salud en los pacientes con EPID de nuestro país.
The World Health Organization defines palliative care (PC) as “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual”.1
In the past 20 years there has been a significant deployment of specialized PC facilities,2 aimed at improving the quality of life of cancer patients. However, the need for PC is not limited to a single disease. Higginson et al., for example, showed that the early introduction of PC in the care of patients with advanced lung disease and refractory dyspnea improves symptom control,3 and the most recent national health strategies have underlined the importance of extending PC to terminal patients with other non-oncological diseases, irrespective of the diagnosis.4
The term “diffuse interstitial lung disease” (DILD) covers a wide array of diseases that share clinical, radiological and histological characteristics.5,6 DILD can have a significant impact on patient survival, particularly in the case of idiopathic pulmonary fibrosis (IPF).7 This disease, which has an estimated average survival of between 3 and 5 years, comparable to some malignant diseases, has a high impact on the life expectancy of patients and symptom control, particularly dyspnea and cough. Together, this leads to an increase in depressive symptoms and loss of quality of life.8
Recent studies have found that patients with DILD require PC in several domains, including physical symptoms and psychosocial and spiritual factors, and that the patient's status can improve if they are promptly referred to appropriate PC units.9,10 However, studies suggest that at present patients are generally referred only at very advanced disease stages.11
The manner in which pulmonologists assimilate PC into their daily practice with DILD patients has seldom been investigated in the literature. The aim of this study was to evaluate the current status of PC in Spain by surveying members of the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR).
MethodsThis study was jointly sponsored by the multidisciplinary DILD unit of the Hospital de la Santa Creu i Sant Pau (S.B., AM.A., D.C.) and the executive committee of the DILD area of SEPAR which was responsible for the design, analysis, and publication of the results (JA.R.P., A.R.O., O.A., D.C.).
International recommendations for optimizing studies based on internet surveys were followed when designing this study,12 which was conducted between October 2015 and September 2016.
SEPAR members were invited to participate in the survey, which consisted of 36 questions in different formats, including multiple-choice and open-ended questions. The aim was to examine the main areas of PC: training, organization, treatment options, and planning for end of life. The Google Drive application was used to prepare the questionnaire. The final version was approved by a specialist in PC (M.V.), and was sent by electronic mail to all SEPAR members (n: 3920) under the supervision of the SEPAR webmaster (J.G.) The full version of the questionnaire is available in the attached document.
Two separate invitations to take part in the survey were sent to SEPAR members during the first half of 2016. Electronic mails were checked to ensure responses were not duplicated, and if so, the second response was deleted. The personal information of the respondents was not recorded at any time, and no incentives were offered for completing the questionnaire.
When the survey was completed, the web platform was used to transfer all responses to a database for statistical analysis that was coordinated by a qualified statistician (F.A.). The analysis was performed using SPSS software version 16 for Windows (IBM Corp., Armonk, New York, USA). The results of the descriptive study are listed as numbers and percentages. All authors participated in the preparation of the final manuscript.
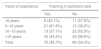
ResultsIn total, 164 professionals from all autonomous communities of Spain participated in the survey. The main sociodemographic characteristics are summarized in Table 1.
Respondents’ sociodemographic characteristics and training in palliative care.
| No. (%) | |
|---|---|
| Participants | 164 |
| Females | 101 (61.6) |
| Years of experience | |
| Less than 5 years | 19 (11.6) |
| Between 5 and 10 years | 34 (20.7) |
| Between 10 and 15 years | 35 (21.3) |
| More than 15 years | 76 (46.3) |
| Place of work | |
| Primary care center | 3 (1.8) |
| Secondary hospital | 37 (22.6) |
| Tertiary hospital | 15 (9.1) |
| University hospital | 107 (65.2) |
| Others | 2 (1.2) |
| Specialist area | |
| General respiratory medicine, with interest in DILD | 94 (57.3) |
| Dedicated DILD clinic | 35 (21.3) |
| Respiratory medicine, not dedicated to DILD | 28 (17.1) |
| Others | 7 (4.3) |
| Training | |
| Respondents with training in PC | 75 (46) |
| Respondents with specific training in PC in DILD | 3 (2) |
Values expressed in absolute number and percentage.
DILD: diffuse interstitial lung diseases; PC: palliative care.
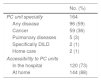
Among the respondents, 161 (98%) expressed an interest in PC, and 75 (46%) of them had received training in this area (Table 1). No differences were observed in years of experience (Table 2).
Training in Palliative Care by Years of Work Experience.
| Years of experience | Training in palliative care | |
|---|---|---|
| Yes | No | |
| <5 years | 8 (42.1%) | 11 (57.9%) |
| 5–10 years | 21 (61.8%) | 13 (38.2%) |
| 10–15 years | 13 (37.1%) | 22 (62.9%) |
| >15 years | 33 (43.4%) | 43 (56.6%) |
| Total | 75 (45.7%) | 89 (54.3%) |
Values expressed in absolute number and percentage.
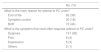
In contrast, 72 (44%) respondents reported that they managed the palliative treatment of their DILD patients, whereas the remaining 92 (56%) left this task to the PC teams. Access to these units was mostly simple, according to respondents, since they were available for any chronic disease. Only 36% stated that they were exclusively for cancer patients (Table 3).
Characteristics of Palliative Care Units.
| No. (%) | |
|---|---|
| PC unit specialty | 164 |
| Any disease | 96 (59) |
| Cancer | 59 (36) |
| Pulmonary diseases | 5 (3) |
| Specifically DILD | 2 (1) |
| Home care | 2 (1) |
| Accessibility to PC units | |
| In the hospital | 120 (73) |
| At home | 144 (88) |
Values expressed in absolute number and percentage.
DILD: diffuse interstitial lung diseases; PC: palliative care.
Fifty-three (32%) of the survey participants had a PC care protocol in place for the management of chronic respiratory patients, and 5 (3%) had a specific protocol for DILD patients. Among respondents who reported having a PC protocol, only 38 (23%) of these had been prepared in coordination with a team of PC specialists.
The main reasons for referring patients to the PC teams were symptom control and end-of-life care (Table 4). Table 5 lists the treatment options for the control of symptoms reported by the respondents. Most respondents (103, 63%) confirmed that they had discussed the end-of-life process with their patients. Likewise, most (128, 78%) also reported coming to an agreement with their patients and family members regarding limiting life-sustaining treatment, although a smaller proportion (58, 35%) usually recommended that a living will be prepared, and only a minority (36, 22%) agreed on the place of death. Answers to the questions about the end-of-life care are listed in Table 6.
Symptom Control.
| No. (%) | |
|---|---|
| What is your drug of choice for the symptomatic treatment of cough? | 164 |
| Codeine | 123 (75) |
| Dextromethorphan | 29 (18) |
| Lidocaine | 5 (3) |
| Others | 7 (4) |
| What route do you usually use for the treatment of dyspnea with opioids? | |
| Oral | 55 (34) |
| Subcutaneous | 12 (7) |
| Transdermal | 24 (15) |
| Oral and subcutaneous | 15 (9) |
| Oral and transdermal | 25 (15) |
| Transdermal and subcutaneous | 5 (3) |
| Oral, transdermal and subcutaneous | 20 (12) |
| Other | 8 (13) |
| How do you assess dyspnea severity? | |
| Visual analog scale | 54 (33) |
| Quality of life questionnaires | 6 (4) |
| Both | 38 (23) |
| None | 66 (40) |
| What first-line treatment do you use for palliative sedation? | |
| Opioids | 97 (59) |
| Midazolam | 64 (39) |
| Propofol | 2 (1) |
| Others | 1 (1) |
Values expressed in absolute number and percentage.
End-of-life Planning.
| No. (%) | |
|---|---|
| Do you discuss end of life with your patients? | 164 |
| Yes | 103 (63) |
| No | 49 (30) |
| I delegate it to the PC team | 12 (7) |
| Do you come to an agreement with your patients regarding limiting life-sustaining treatment? | |
| Always | 39 (24) |
| Often | 89 (54) |
| I delegate it to the PC team | 3 (2) |
| Rarely | 31 (19) |
| Never | 2 (1) |
| Do you encourage your patients to make a living will? | |
| Always | 10 (6) |
| Often | 48 (29) |
| I delegate it to the PC team | 5 (3) |
| Rarely | 75 (46) |
| Never | 26 (16) |
| Do you discuss place of death with your patients? | |
| Always | 3 (2) |
| Often | 33 (20) |
| I delegate it to the PC team | 11 (7) |
| Rarely | 77 (47) |
| Never | 40 (24) |
Values expressed in absolute number and percentage.
PC: palliative care.
This is the first Spanish study performed to evaluate the status of PC in DILD. The data obtained show that health professionals lack training in this area, PC is administered in an inconsistent manner, and most importantly, the approach to such an important event as end of life is significantly deficient in some areas.
DILD and, more particularly, IPF are diseases that have a high impact on a patient's quality of life.8 A survey published by Russell et al., based on interviews with IPF patients from 3 European countries, showed that patients reported a decline in both their physical and emotional quality of life due to their disease.13 IPF also has a high mortality rate, and is estimated to be the leading cause of death in about 60% of affected individuals.14 Clinical guidelines, the Spanish health system quality of care recommendations, and expert opinions all emphasize the importance of the role of PC in DILD patients.15–17
No data are available on the use of these resources in Spain, but our survey shows that most hospitals have PC units that provide care both in the clinic and in the patient's home. However, a significant number of pulmonologists do not refer their patients to these units, and instead assume the exclusive responsibility of caring for their patients’ needs. This may be because some PC units are dedicated solely to the care of cancer patients. This limitation is not unique to Spain. A review of around 60000 deaths conducted in the US found that PC care was deficient in chronic diseases (such as respiratory conditions), compared to oncological disease.18 In Europe, a study of a representative cohort of patients from 11 countries found that access to PC was limited in some countries.19 It seems reasonable, then, that the first step should be for DILD patients to be offered access to PC units when required. This would involve resolving structural constraints and fostering multidisciplinary initiatives between the respiratory medicine department and PC units.
Indeed, access to PC should ideally be established in consensus statements and included in clinical care protocols/guidelines. Another significant finding of this study is that most respondents do not have PC protocols in their hospitals, and those that do report that these documents were not drawn up in collaboration with the corresponding PC unit. The great distinction of PC is that it is not limited to pharmacological treatment, but addresses many other issues, such as emotional and spiritual concerns, that also need to be adequately addressed.9 Thus, one of the other areas of improvement detected is the introduction of consensus clinical guidelines in chronic respiratory patients.
As mentioned above, the wide range of diseases that constitute DILD can have a significant impact on patient quality of life. The 2 main symptoms of the disease, dyspnea and cough, can sometimes be very difficult to manage. A recent review of the literature found very little scientific evidence on the efficacy of several widely used drugs in relieving these symptoms.20 The data collected in this survey indicate homogeneity in the treatment of cough, with codeine being the drug most commonly prescribed. Dyspnea tends to be managed with opioids, although more variability is observed in routes of administration. There is a clear need, then, for more information on the best way to administer this treatment, and clinical trials designed to address this issue must be conducted.
Another very significant finding from our study is that, although dyspnea was the main reason for referral to the PC unit, up to 40% of respondents did not use a systemic scale to assess the severity of this symptom. It is therefore difficult to determine the outcome of any intervention, and our study reveals a pressing need to encourage the use of clinical scales and quality of life questionnaires to monitor symptoms in these patients. Indeed, simplified multidimensional tools developed specifically for chronic respiratory patients that could be used to measure the overall impact of the illness on patients’ lives would be of interest. This would help us to determine PC needs in a timely fashion and assist in improving the patient's quality of life.
With regard to drug treatment, it is striking that most respondents opted to use opioids as the first line of treatment in palliative sedation. In this specific situation, clinical management guidelines recommend the use of sedatives, primarily benzodiazepines.21,22
Finally, the few studies available on the provision of PC to DILD patients have revealed a number of deficiencies in this area, particularly with regard to planning end-of-life care and place of death. Bajwah et al. were the first to point out the lack of documented preferences for place of death in the medical notes of DILD patients.9 Lindell et al. subsequently reviewed a cohort of patients with IPF in the United States. Most of those who had died did so in a hospital, and only a minority had been formally referred to a PC unit in the months prior to admission.23 Another series, this time from Finland, obtained similar results with respect to place of death.11 This means that DILD patients are not only unable to choose their place of death, but may also be subjected to invasive procedures or unnecessary tests at the end of their life due to being hospitalized. Rajala et al. also showed that DILD patients who died in hospitals, particularly tertiary hospitals, underwent more diagnostic tests (chest X-ray, blood tests) than those in hospice care.11 In Spain, according to our survey, 71% of respondents do not discuss the place of death with their patients, in line with the findings from other countries mentioned above. Although this could be interpreted as suggesting that great majority of respondents delegate end-of-life discussions to the PC teams, it is interesting to note that most respondents do discuss the limitation of life-sustaining treatment with their patients. On the whole, the results of our survey show significant shortcomings in the end-of-life management of DILD patients that must be corrected; for example, patients are not informed about the possibility of making a living will.
One of the most significant issues highlighted in this study is that most respondents, despite their interest in PC, had not received training in this area, and it seems likely that this factor is related with the need for improvement in certain areas. Respiratory medicine specialization programs do not currently cover training in PC. Moreover, to our knowledge, no continuous professional development programs are provided by scientific societies for DILD specialists. An essential intervention would be to improve the training of healthcare professionals in PC for patients with chronic respiratory diseases.
The major limitation of this study, and one inherent to any type of survey conducted using similar methodology, is the voluntary nature of participation, giving rise to questions as to whether the results really represent the true situation under study. Data on the distribution of age, geographic region, and medical experience of our respondents allow us to conclude that the results most likely are a close reflection of the current status of PC in DILD in Spain. However, the possibility exists that those members who were more interested in this topic may have been more motivated to respond to the survey.
In conclusion, the healthcare professionals who participated in the survey show a considerable interest in the PC of DILD patients. Nevertheless, the data from our survey show that there are still clinical, structural, and educational deficiencies that must be addressed in order to optimize the palliative care currently provided to Spanish DILD patients.
Conflict of InterestsThe authors state that they have no conflict of interests.
We thank the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR), and specifically the webmasters for their help in distributing the questionnaire.
Please cite this article as: Barril S, Alonso A, Rodríguez-Portal JA, Viladot M, Giner J, Aparicio F, et al. Cuidados paliativos en la enfermedad pulmonar intersticial difusa: resultados de una encuesta de ámbito nacional. Arch Bronconeumol. 2018;54:123–127.