Obstructive fibrinous tracheal pseudomembrane (OFTP) is believed to be a complication of tracheal intubation. Here, we describe a unique case of OFTP after silicone stent insertion. In this case, an hourglass-shaped stent was inserted to mitigate airway obstruction in a patient diagnosed with post-intubation tracheal stenosis. Although silicone stents are considered safe, they are associated with numerous complications. To our knowledge, pseudomembrane formation after silicone stent insertion has never been reported.
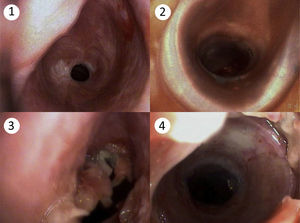
A 48-year-old man, a former smoker (about 30 pack-years), was admitted to our hospital with a 3-month history of progressive dyspnea, stridor, and cough. He had a medical history of intubation and mechanical ventilation 6 months previously due to drug intoxication. He had no relevant family history. On physical examination, the patient presented tachypnea and central cyanosis. The arterial blood gas analysis showed hypoxia (pH=7.42, PaO2=57mmHg, PaCO2=31mmHg, HCO3−=20mmol/l, room air). The complete blood count revealed leukocytosis of 10.75×109/L (normal range: 4.0–10.0×109/L). A diagnosis of post-intubation tracheal stenosis was considered first, and chest computed tomography was performed while the patient was receiving oxygen therapy. A marked circumferential stenosis of the trachea was found, with no signs of extrinsic mass. Fiber optic bronchoscopy was performed immediately to assess the airway stenosis, showing a subglottic stenosis of the trachea (Fig. 1.1). In order to reduce the dyspnea, an hourglass-shaped silicone stent (Dumon™Silicone stent) was inserted by means of rigid bronchoscopy, after which the bronchoscopy showed a widely patent airway (Fig. 1.2) and dyspnea improved significantly.
Two days later, dyspnea returned, and fiberoptic bronchoscopy was performed twice, finding a thick, valve-like membrane above the stent (Figs. 1.3 and 1.4). The membrane was removed under bronchoscopy with the help of grasping forceps, after which the patient's dyspnea completely resolved. The histopathological examination of the membrane showed fibrin, necrotic epithelium cells, and exudate, with no evidence of bacteria, fungi or mycobacterium.
Upper airway obstruction, which can be either malignant or benign, is a complicated clinical problem. The former is caused by primary or secondary lung cancer, while the latter is often caused by tracheal intubation, tracheostomy, and other medical treatments. The aim of therapy is to alleviate symptoms in order to prolong survival and improve quality of life. The silicone stent was first used in the management of airway stenosis in the 1990s,1 and has been associated with complications such as worsening cough, stent obstruction with secretion, migration, or granulation.2
It is rare to find an OFTP after silicone stent insertion; most cases have hitherto been reported after tracheal intubation. The OFTP patient often complains of dyspnea, hoarseness or stridor that may occur immediately after extubationor a few hours later, and in severe cases may lead to respiratory failure. Flexible or rigid bronchoscopy is essential for the diagnosis and treatment of OFTP.
The etiopathogenesis of OFTP remains unclear, and multiple hypotheses have been proposed. Sehgal and colleagues retrospectively analyzed a series of 54 cases, and found most pseudomembranes to be located in the subglottic region, the narrowest part, where the mucosa is most sensitive during intubation. However, not all cases are located below the glottis.3 Deslee and colleagues suggest cuff-induced ischemic damage as a possible cause, althought his theory does not explain cases in which high-volume low-pressure tubes were used.4 In 2013, Alvarez-Maldonado and colleagues reported a case of pseudomembrane formation following percutaneous dilatational tracheostomy (PDT).5 In our case, OFTP occurred after silicone stent insertion. Both cases show that various factors may be related to OFTP, including mechanical stimulus and local aseptic inflammation. To sum up, OFTP is an uncommon complication after silicone stent insertion, and can be fatal if not diagnosed promptly. Bronchoscopy is essential in the management of OFTP.
Please cite this article as: Han X-P, Liu D-J, Liu Y-L, Liu J-B. Seudomembrana traqueal fibrinosa obstructiva tras la inserción de una endoprótesis de silicona. Arch Bronconeumol. 2017;53:529–530.