We thank Dr. Carratalá (Arch Bronconeumol 2018; 54:594) and colleagues for their comments on our study on the use of non-invasive mechanical ventilation (NIMV) versus continuous positive airway pressure (CPAP) in patients with cardiogenic acute pulmonary edema (APE) in an intensive care unit (ICU).1 The authors mention that our inclusion criteria were selective, as we excluded patients with chronic obstructive pulmonary disease (COPD) and respiratory infection causing heart failure. This exclusion was based on the fact that many patients with COPD exacerbations have severe respiratory acidosis, which might make the comparison of these two devices risky, particularly when NIMV is clearly indicated in COPD with respiratory acidosis.2 Many of the papers we referenced in our article similarly excluded patients with COPD or severe respiratory acidosis.3
With regard the CPAP system used (Boussignac® or WhisperFlow®), the Boussignac® was used in 98% of cases (43 patients). The main reasons for this were: (1) the availability of that system in the hospital emergency department (ED) at the time of the study; (2) its interface is more comfortable, and also allows patients to speak; and, (3) it is quieter than the WhisperFlow® device. In terms of tolerance, oronasal interfaces (both CPAP and NIMV) often cause ulcers on the bridge of the nose,4 side effects that while not registered in our study, are widely recorded in clinical practice after prolonged use (9%–40%).5
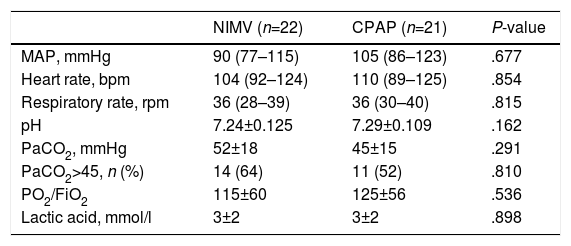
From a methodological point of view, we included 43 patients from the ED who had not improved despite medical treatment (24 with use of CPAP; none had used NIMV, as this device was not available during the study period). In order to preserve homogeneity and avoid bias, patients were randomized irrespective of their previous use of CPAP. The study protocol did not contemplate any crossover between the ventilatory support modalities. With regard to variables on admission to the ICU after referral from the ED (Table 1), despite most patients being hypercapnic, this did not negatively impact on the device used. The authors stress the importance of avoiding undesirable derecruitment when switching from one device to another, and, indeed, we did not record the level of CPAP used in the ED. However, the CPAP levels and expiratory positive airway pressure (EPAP) used during the first hour in the ICU were 7±2cm/H2O and 6±1cm/H2O, respectively. These values were within the range set in the references used in our study,3 and in reviews conducted in the ED setting.4
Comparison of Hemodynamic Variables and Arterial Blood Gases of Patients Referred from the ED.
| NIMV (n=22) | CPAP (n=21) | P-value | |
|---|---|---|---|
| MAP, mmHg | 90 (77–115) | 105 (86–123) | .677 |
| Heart rate, bpm | 104 (92–124) | 110 (89–125) | .854 |
| Respiratory rate, rpm | 36 (28–39) | 36 (30–40) | .815 |
| pH | 7.24±0.125 | 7.29±0.109 | .162 |
| PaCO2, mmHg | 52±18 | 45±15 | .291 |
| PaCO2>45, n (%) | 14 (64) | 11 (52) | .810 |
| PO2/FiO2 | 115±60 | 125±56 | .536 |
| Lactic acid, mmol/l | 3±2 | 3±2 | .898 |
CPAP: continuous positive airway pressure; ED: emergency department; MAP: mean arterial pressure; NIMV: non-invasive mechanical ventilation.
Finally, the duration of ventilation in the hypercapnic CPAP group that failed (n=4) was very similar to that of the NIMV hypercapnic group that failed (n=4) (4 [2–6] h vs 4 [2–6] h, respectively), which supports the homogeneity of the sample and the results obtained.
Please cite this article as: Belenguer Muncharaz A. Ventilación mecánica no invasiva versus presión continua positiva en la vía aérea en el edema agudo de pulmón cardiogénico en una unidad de cuidados intensivos. Arch Bronconeumol. 2019;55:63–64.