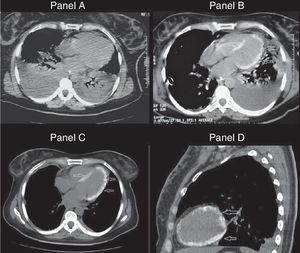
A previously healthy 28-year-old woman was admitted on the intensive care unit with a diagnosis of septic shock. Her blood pressure was 50/40mm Hg and presented signs of systemic hypoperfusion, including obnubilation. A chest computed tomography revealed pneumonia and bilateral pulmonary pleural effusion (Fig. 1: panel A). The patient required hemodynamic and ventilatory support, broad spectrum antibiotics and a bilateral thoracic drainage. The results of pleural fluid analysis were compatible with empyema; in the culture we were able to isolate Klebsiella pneumoniae. A new TC scan was repeated six days after the admission and found improvement on the pulmonary infiltrate, persistence of the pleural effusion and an unexplained myocardial left ventricular calcification1 (Fig. 1: panel B). She was discharged in a stable condition, with persistent tachycardia and a pleuritic chest pain. 20 days after being discharged, she returned for a routine control, presenting chest pain and tachycardia. The new CT revealed a minimal pleural effusion and radiologic improvement of the pneumonia with an increase in the density and distribution of the calcification in the left ventricle2 (Fig. 1: panels C and D). The pathophysiology of myocardial calcification is not fully explained. Usually, it represents the sequel of a local tissue damage, impaired membrane or cellular necrosis and is not associated with abnormalities in serum calcium levels or calcium metabolism. The most common cause is myocardial infarction, but it has also been reported in the context of trauma, infections, inflammatory or neoplastic processes.3
Panel A. Tomography performed on admission showing bilateral pleural effusion and pulmonary consolidation. Panel B. Similar tomography slice obtained 7 days later, revealing calcified ventricular myocardium. Panels C and D. Extensive calcification throughout the left ventricular myocardium (day 30).
Please cite this article as: Torracchi Carrasco AM. Calcificación miocárdica: una complicación excepcional de la neumonía y la sepsis. Arch Bronconeumol. 2017;53:270.