Failure to rescue (FTR), defined as the mortality rate among patients suffering from postoperative complications, is considered an indicator of the quality of surgical care. The aim of this study was to investigate the risk factors associated with FTR after anatomical lung resections.
MethodPatients undergoing anatomical lung resection at our center between 1994 and 2018 were included in the study. Postoperative complications were classified as minor (grade I and II) and major (grade IIIA to V), according to the standardized classification of postoperative morbidity. Patients who died after a major complication were considered FTR. A stepwise logistic regression model was created to identify FTR predictors. Independent variables included in the multivariate analysis were age, body mass index, cardiac, renal, and cerebrovascular comorbidity, ppoFEV1%, VATS approach, extended resection, pneumonectomy, and reintervention. A non-parametric ROC curve was constructed to estimate the predictive capacity of the model.
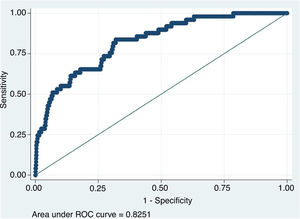
ResultsA total of 2.569 patients were included, of which 223 (8.9%) had major complications and 49 (22%) could not be rescued. Variables associated with FTR were: age (OR: 1.07), history of cerebrovascular accident (OR: 3.53), pneumonectomy (OR: 6.67), and reintervention (OR: 12.26). The area under the ROC curve was 0.82 (95% CI: 0.77–0.88).
ConclusionsOverall, 22% of patients with major complications following anatomical lung resection in this series did not survive until discharge. Pneumonectomy and reintervention are the most significant risk factors for FTR.
El fallo en el rescate (FTR) definido como la tasa de fallecimientos entre los pacientes que sufren una complicación postoperatoria, es considerado un indicador de la calidad de los cuidados quirúrgicos. El objetivo de este estudio es investigar los factores de riesgo asociados al FTR después de resecciones pulmonares anatómicas.
MétodoSe incluyeron en el estudio pacientes sometidos a resección pulmonar anatómica en nuestro centro entre 1994 y 2018. Las complicaciones postoperatorias se clasificaron en menores (grados I y II) y mayores (grados IIIa a V) según la clasificación estandarizada de morbilidad postoperatoria. Los casos que fallecieron tras una complicación mayor fueron considerados FTR. Se creó un modelo de regresión logística por pasos para identificar los factores predictores de FTR. Se consideraron variables independientes en el análisis multivariante la edad, índice de masa corporal, comorbilidad cardiaca, renal, cerebrovascular, VEF1ppo%, abordaje VATS, resección extendida, neumonectomía y reintervención. Se construyó una curva ROC no paramétrica para estimar la capacidad predictiva del modelo.
ResultadosSe analizaron 2.569 pacientes. En total, 223 casos (8,9%) tuvieron complicaciones mayores y 49 (22%) no pudieron ser rescatados. Las variables asociadas con FTR fueron: edad (OR: 1,07), antecedente de ACV (OR: 3,53), neumonectomía (OR: 6,67) y reintervención (OR: 12,26). El área bajo la curva de la curva ROC fue 0,82 (IC 95%: 0,77–0,88).
Conclusiones22% de los pacientes que presentan complicaciones mayores tras la resección pulmonar anatómica en esta serie no sobreviven al alta. La neumonectomía y la reintervención son los factores de riesgo más potentes para FTR.
The term “failure to rescue” (FTR) was first coined in 1992 by Silber et al.1 and refers to patient mortality after major postoperative complication. The FTR of complicated patients has been proposed as an alternative parameter to postoperative morbidity and mortality rates to measure quality of care and assess the functioning of a surgical or hospital facility. According to Silber et al.1, while patient characteristics determine the occurrence of postoperative complications, hospital characteristics are associated with FTR. Thus, several studies2–4 have linked high rates of FTR with hospital factors, such as low volume of surgeries or low nurse-patient ratios. Furthermore, according to Farjah et al.5, the variation in mortality rates between different hospitals is more strongly related to the ability to rescue complicated patients than to the occurrence of complications. The FTR parameter, then, offers a perspective that complements the conventional postoperative morbidity and mortality outcomes used to assess the quality of surgical units6. For this reason, some hospitals and departments have already introduced FTR as an additional indicator of quality.
Although FTR is closely related to the ability to promptly detect and treat complications, and is based mainly on hospital characteristics, some studies have investigated whether there are intrinsic patient factors that could increase the risk of FTR after complex surgeries with high complication rates7–10, although none of these analyses included patients undergoing lung resection surgeries.
Our hypothesis was that certain high-risk patients are more likely to die of a major postoperative complication after lung resection, compared to the general population. The aim of the study was to investigate FTR among patients undergoing anatomical lung resection and to determine whether certain patient or surgical characteristics are predictors of FTR.
MethodStudy populationWe retrospectively analyzed the records of all patients consecutively undergoing scheduled anatomical lung resection (standard segmentectomy, lobectomy, bilobectomy, or pneumonectomy) for any cause between October 1994 and February 2018 at our center. All patients with at least one major postoperative complication, defined as grade IIIa or higher according to the standardized Clavien-Dindo morbidity classification, were included in the study11. Patients with missing data at discharge were excluded from the analysis.
Patient selection criteria were consistent throughout the study period and were based on the preoperative functional assessment guidelines in place at the time of the intervention12–15. The patients were operated on by 5 expert surgeons. The surgical approach was via axillary thoracotomy without muscle section or video-assisted thoracoscopic surgery (VATS) in all cases. The patients were extubated in the operating room, and after 6h in the reanimation unit were transferred to the hospital ward. Postoperative analgesia consisted of an epidural catheter with bupivacaine and fentanyl in patients undergoing thoracotomy or a paravertebral catheter with the same medication in cases of VATS approach for 48h and paracetamol and non-steroidal anti-inflammatory drugs thereafter. Postoperative physiotherapy was initiated the day before surgery and continued after patient discharge. During the first 2 years of the study, patients were supervised by nursing staff during physiotherapy. However, in November 2002, the current intensive physiotherapy protocol based on physical exercise on a static bike was implemented. These sessions are supervised by an expert physiotherapist who also assists patients with breathing maneuvers using an incentive spirometer and helps them achieve effective coughing.
Patient data were prospectively collected in an institutional database. To improve the quality of the data included in the registry, the completeness and accuracy of the data entries was monitored by a data manager at 2 different timepoints: first, upon discharge from the hospital, and then at the time the last histological result was included in the final medical reports.
Statistical analysisThe outcome variable was FTR, defined as mortality (in-hospital or 30-day) among patients who experienced a major postoperative complication. In the event of death after hospital discharge, patient records were re-evaluated to determine if the patient died as a result of an in-hospital complication.
Postoperative complication was defined as any adverse event that occurred during admission or within 30 days of surgery, including: respiratory failure (need for mechanical ventilation for more than 24h or need for re-intubation at any time), acute respiratory distress syndrome, atrial arrhythmia, ventricular arrhythmia, atelectasis requiring bronchoscopy, pneumonia, pulmonary embolism, acute myocardial infarction, renal failure, cerebrovascular accident (CVA), prolonged air leak (defined as persistent air leak through the pleural tube for more than 5 days after surgery), hemothorax, pneumothorax with or without air leak requiring drainage, bronchial fistula, wound dehiscence, wound hematoma, empyema, chylothorax, recurrent paralysis, and phrenic nerve paralysis. These complications were defined in advance according to the definition of variables published jointly by the American (STS) and European (ESTS) Societies of Thoracic Surgeons16 and subsequently reclassified retrospectively according to the standardized Clavien-Dindo classification of postoperative morbidity as major (grade III: complications requiring endoscopic or radiological reintervention with or without general anesthesia; grade IV: life-threatening complications requiring treatment in intensive or intermediate care; grade V: complications leading to patient death) or minor (grade I: any deviation from the normal postoperative period that does not require reintervention, while allowing the administration of electrolytes, antiemetics, antipyretics, analgesics, and physiotherapy; grade II: complications requiring pharmacological treatment with drugs other than those allowed for grade I complications, including blood products and parenteral nutrition).
The variables considered as risk factors for postoperative morbidity and mortality, mostly specified in the Eurolung 1 and 2 risk models17, were used as independent predictors in multivariate binary logistic regression analysis: age, body mass index (BMI), cardiac, renal, cerebrovascular comorbidity (CVA), expiratory volume in 1s predicted postoperatively (ppoFEV1%), video-assisted thoracoscopy (VATS) approach, extensive resection, pneumonectomy, and reintervention.
A logistic regression model was created for the occurrence of FTR. A backward stepwise logistic regression test was used to select the variables. Only variables with p value <0.05 remained in the final model.
To estimate the predictive capacity of the model, a non-parametric ROC curve was constructed and the area under the curve (AUC) and its 95% confidence interval (95% CI) were calculated.
Statistical analysis was carried out using the STATA/IC 15.1 statistical software package.
ResultsDuring the study period, 2569 cases underwent lung resection. In total, 53 patients (2.1%) were excluded due to incomplete data. The demographic and clinical variables of the series are listed in Table 1.
Demographic and clinical variables.
| Variable | N (%) |
|---|---|
| Sex (male) | 2058 (81.8) |
| Vascular disease | 46 (1.83) |
| Renal failure | 60 (2.38) |
| Coronary artery disease | 380 (15.1) |
| Approach (VATS) | 480 (19.08) |
| Extended resection | 367 (14.59) |
| Pneumonectomy | 307 (12.2) |
| Reintervention | 81 (3.22) |
| Mean±standard deviation | |
| Age | 65.28±9.98 |
| BMI | 26.4±4.16 |
| ppoFEV1% | 63.41±18.15 |
BMI: body mass index; ppoFEV1%: predicted postoperative forced expiratory volume in 1s; VATS: video-assisted thoracoscopy.
Overall, 223 (8.9%) had major complications and, of these, 49 (22%) could not be rescued.
Table 2 shows the results of the stepwise logistic regression analysis (dependent variable: failure to rescue). In the final model, the variables associated with FTR were: age, history of stroke, pneumonectomy, and reintervention.
The ROC curve obtained, that estimates the predictive capacity of the model, can be seen in Fig. 1. The AUC was 0.82 (95% CI: 0.77–0.88).
DiscussionReproducible indicators that accurately reflect the quality of medical care are essential for health systems. However, traditional parameters, such as complication rate, appear to have a poor correlation with in-hospital mortality due, mainly to differences in the characteristics and risk factors for death after complications among the different patient populations18,19. Moreover, the occurrence of postoperative complications is more strongly related to patient-related factors than to hospital characteristics and quality of care1,18. These circumstances mean that the complication rate is a suboptimal indicator of quality of care. A more precise parameter is the measure of the effectiveness of the response to a complication in preventing mortality. Therefore, the use of the FTR index as a measure of the quality of healthcare, understood as the number of deaths among patients experiencing an adverse event such as a postoperative complication, is increasing significantly.
According to the latest report of the European Society of Thoracic Surgeons (ESTS), the rate of mortality and cardiorespiratory morbidity after anatomical lung resection is estimated to be 2.3% and 14.9%, respectively20; according to our results, the prevalence of major complications after anatomical lung resection is 8.9%, with the FTR index reaching 22%. This is similar to the data recorded by Ahmed et al.21 after cardiac surgery (RTF: 19.8%), although greater than the 6% published by Liou et al.7 after esophagectomy.
In this study, we identified several patient- and surgery-related factors that predict FTR after anatomical lung resection. To date, studies that have evaluated FTR have focused only on hospital characteristics such as size, patient volume, technological facilities, educational level, and nurse-patient ratios2,22. In thoracic surgery literature, FTR has been studied in lung and esophageal cancer, and findings regarding hospital qualities have been similar5,23,24.
Although modifying certain hospital characteristics may help improve outcomes, our aim was to assess whether any specific patient- or surgery-related factors were associated with a higher probability of mortality after a major postoperative complication, so that by identifying patients at high risk for FTR, we could focus efforts on how to prevent complications in these patients or how to rescue them after a complication does occur.
Our data show that age, history of cerebrovascular disease, pneumonectomy, and need for reintervention increase the risk of failure to rescue after lung resection. The logistic regression model based on these variables accurately predicts FTR (AUC: 0.82). All the variables listed by the risk models of cardiorespiratory morbidity and postoperative mortality (Eurolung 1 and 2) were included as independent variables in multivariate binary logistic regression analysis but, of the patient-related factors, only age and history of stroke emerged as predictors of FTR, while for the surgical procedure, pneumonectomy and the need for reintervention increased the risk of FTR. The effect of the latter, furthermore, is very significant, to the extent that a pneumonectomized patient with a major complication is 6.6 times more likely to die than a patient with a smaller resection. Similarly, a patient who needs a reintervention is 12 times more likely to die than a patient who does not need a reintervention.
These findings are consistent with previous studies. Elderly patients have higher FTR rates after urgent surgical interventions than younger patients25. Liou et al.7 and Varley et al.10 found that older age was a predictor of FTR after esophagectomy and duodenopancreatectomy, respectively. Our findings of a high risk after complex surgery such as pulmonary resection are therefore not unexpected, as the patient is subjected to extreme physiological stress in all 4 situations.
Numerous studies have shown that pneumonectomy is associated with significant postoperative mortality that can be as high as 8.4% at 30 days and reach 18.5% within 6 months of the intervention26. The factors that determine these results include patient age, the laterality of the procedure, and the occurrence of postoperative cardiorespiratory complications, so it stands to reason that pneumonectomy is a predictor for FTR.
However, a recent British study comparing high-mortality hospitals versus low-mortality hospitals after esophagectomy showed that low-mortality hospitals performed more reinterventions for complications but had lower rates of FTR. Our results contradict these findings, and can be explained by the fact that reinterventions after lung resection are usually the consequence of a serious initial complication (hemorrhagic or infectious) from which additional complications arise (prolonged intubation, pneumonia, etc.). It is, therefore, the accumulation of complications associated with the intervention that leads to FTR, as occurs in other similar scenarios10.
Our study has some limitations: as in any retrospective analysis, causality cannot be determined from the different variables analyzed; mortality was only determined in-hospital and at 30 days after discharge; deaths related to postoperative complications that occurred beyond 30 days were not included in the analysis; finally, in terms of the type of anatomical resection performed, although the study included all patients undergoing standard segmentectomy, lobectomy, bilobectomy, or pneumonectomy, only procedures that were found in previous studies to constitute a potential risk of postoperative morbidity and mortality (extended resection and pneumonectomy) were taken into account and included in the multivariate analysis as independent risk variables.
In conclusion, our results show that 22% of patients with a major complication did not survive discharge. Factors that predict mortality after major complications include age, history of stroke, pneumonectomy, and reintervention. Although failed rescue efforts may be the result of certain hospital deficiencies, our results confirm the hypothesis that some patients are more likely to die after a major postoperative complication. Further studies are needed to determine how complications could be detected earlier and treated more effectively in this group of high-risk patients.
Source of fundingThis study has not received specific grants from public sector agencies, the commercial sector, or non-profit organizations.
Conflict of interestsThe authors state that they have no conflict of interests.
Please cite this article as: Gómez Hernández MT, Novoa Valentín N, Fuentes Gago M, Aranda Alcaide JL, Varela Simó G, Jiménez López MF. Variables predictivas de muerte en pacientes complicados tras resección pulmonar anatómica. Arch Bronconeumol. 2021;57:625–629.