Asthma is a disease that is heterogeneous in its clinical presentation and epidemiology. Since the 1960s, its prevalence among adults and children has increased in both developed and developing countries. Despite this increase, a significant reduction in asthma-related mortality and the number of hospital admissions for severe exacerbations has been observed since 1990, mainly due to improved access to health services and the increasing use of inhaled corticosteroids (ICS). The decrease in mortality and hospitalization rates appears to have slowed during the last decade1,2 and remains unchanged worldwide, and in Spain there is even evidence of an increase over the last 4 years3 despite significant advances in new therapies and improvements in drug delivery devices and patient care. Thus, asthma remains one of the most prevalent treatable diseases at the global level, and constitutes a serious public health problem mainly due to inequity in access to health services, sociocultural differences that impact on mortality, poor treatment compliance, and probably excessive use of short-acting bronchodilators (SABA).4,5
Mild asthma is the most common type of asthma, and should also be the most easily controlled. Despite this, a significant percentage of patients have inadequate disease control, and the only treatment they receive is SABA as-needed, which produces a rapid relief of symptoms while perpetuating and even increasing bronchial inflammation.6 It has now been demonstrated that the long-term or on-demand use of SABA in monotherapy can trigger or facilitate eosinophilic inflammation,7,8 increase the risk of severe asthma exacerbations, and cause higher mortality.9 These factors together with evidence from important studies in this respect published last year have led to changes in the Global Initiative for Asthma (GINA) recommendations for the treatment of mild asthma. One change is the inclusion of formoterol (long-acting β2 adrenergic agonist [LABA])/ICS as-needed or the use of ICS for the control of these patients in the first treatment step.10 O’Byrne et al.11 and Bateman et al.12 have shown that patients with mild asthma treated with LABA/ICS as-needed not only had greater control of symptoms compared to treatment with SABA, but also reduced the annual rate of severe exacerbations by 64%, the rate of moderate to severe exacerbations by 60%, and the cumulative dose of ICS or systemic medications used. Moreover, the reduction in severe exacerbations was similar when compared to treatment with continued ICS, although it should be noted that the combination was less effective than maintenance ICS in symptom control and lung function. It also should be pointed out that compliance with ICS treatment in the study was close to 80%, a far cry from that observed in real life.
In this context we have retrospectively analyzed a cohort of patients with a previous diagnosis of bronchial asthma admitted to our tertiary university hospital between June 2018 and June 2019 for severe asthmatic exacerbation, defined as the presence of signs and symptoms of respiratory failure.13 We performed a detailed analysis of the characteristics of patients with life-threatening exacerbations, defined as patients who required admission to the intensive care unit (ICU) or the semicritical care unit.14
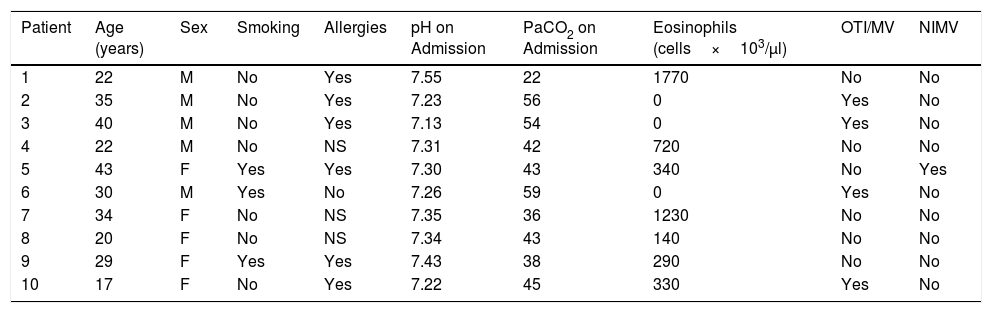
In terms of results, a total of 96 patients with a previous diagnosis of asthma were admitted with severe exacerbations. The median age of the group was 58 years with an average length of stay of 8 days. Of these patients, 10.4% had a life-threatening asthma exacerbation, requiring admission to the ICU or semicritical care unit. Analysis of this subgroup of patients revealed a typical profile of young individuals with a mean age of 28 years; most had a diagnosis of allergic asthma and all were treated with rescue SABA alone. About half required orotracheal intubation and mechanical ventilation for a mean of 31 hours. There were no deaths during admission or during the 90 days after discharge (phone follow-up). None of the patients had been followed up during the last year by the respiratory medicine or allergology units. It should be noted that none of the patients had presented severe exacerbations in the previous year, and based on the Spanish guidelines for asthma management (GEMA), 8 patients had intermittent/intermittent-mild asthma and disease status could not be established in 2 patients, and were therefore still monitored by their primary care physician (Table 1).
Characteristics of the Subgroup of Patients With Life-threatening Exacerbations.
| Patient | Age (years) | Sex | Smoking | Allergies | pH on Admission | PaCO2 on Admission | Eosinophils (cells×103/μl) | OTI/MV | NIMV |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 22 | M | No | Yes | 7.55 | 22 | 1770 | No | No |
| 2 | 35 | M | No | Yes | 7.23 | 56 | 0 | Yes | No |
| 3 | 40 | M | No | Yes | 7.13 | 54 | 0 | Yes | No |
| 4 | 22 | M | No | NS | 7.31 | 42 | 720 | No | No |
| 5 | 43 | F | Yes | Yes | 7.30 | 43 | 340 | No | Yes |
| 6 | 30 | M | Yes | No | 7.26 | 59 | 0 | Yes | No |
| 7 | 34 | F | No | NS | 7.35 | 36 | 1230 | No | No |
| 8 | 20 | F | No | NS | 7.34 | 43 | 140 | No | No |
| 9 | 29 | F | Yes | Yes | 7.43 | 38 | 290 | No | No |
| 10 | 17 | F | No | Yes | 7.22 | 45 | 330 | Yes | No |
MV: mechanical ventilation; NIMV: non-invasive mechanical ventilation; NS: non-significant; OTI: orotracheal intubation.
In conclusion, our study reveals a profile of a young “mild” asthmatic patient with an allergic phenotype, treated only with as-needed SABA who was ultimately admitted to the emergency department with a life-threatening asthma exacerbation. It should be noted that salbutamol is the seventh most sold drug in Spanish pharmacies, provided in many cases without a correct medical prescription. It produces rapid relief of symptoms but perpetuates inflammation and can have fatal consequences, so we believe that the treatment of mild asthma with SABA as-needed should be reassessed, even in the first treatment step. Today, despite increasing evidence, the latest version of GEMA9 continues to recommend as-needed SABA in the first treatment step, although on the basis of current scientific evidence it does recommend the use of maintenance ICS in step 2.
This study has its limitations: it is retrospective and the number of patients is low; however, we believe that our observations should give pause for thought on the consequences of inadequate treatment. Therefore, taking into account our data and the results published by O’Byrne et al.,11 we believe that treatment with LABA/ICS as-needed could have a beneficial impact on patients with mild asthma, particularly when the problem of poor compliance with inhaled treatment in this type of patients is taken into account, as it would help maintain high effectiveness in the prevention of serious exacerbations. We are, however, aware of the difficulty in identifying these patients, and community pharmacists are probably in a better position to detect them when they come for rescue medication, and these professionals would therefore be another key link in the chain of prevention and control of asthma.
Please cite this article as: González-García JG, Chalela R, Carballo N, Ausín P. Asma leve y exacerbaciones de riesgo vital: ¿es hora de que demos un paso adelante? Arch Bronconeumol. 2020;56:395–396.