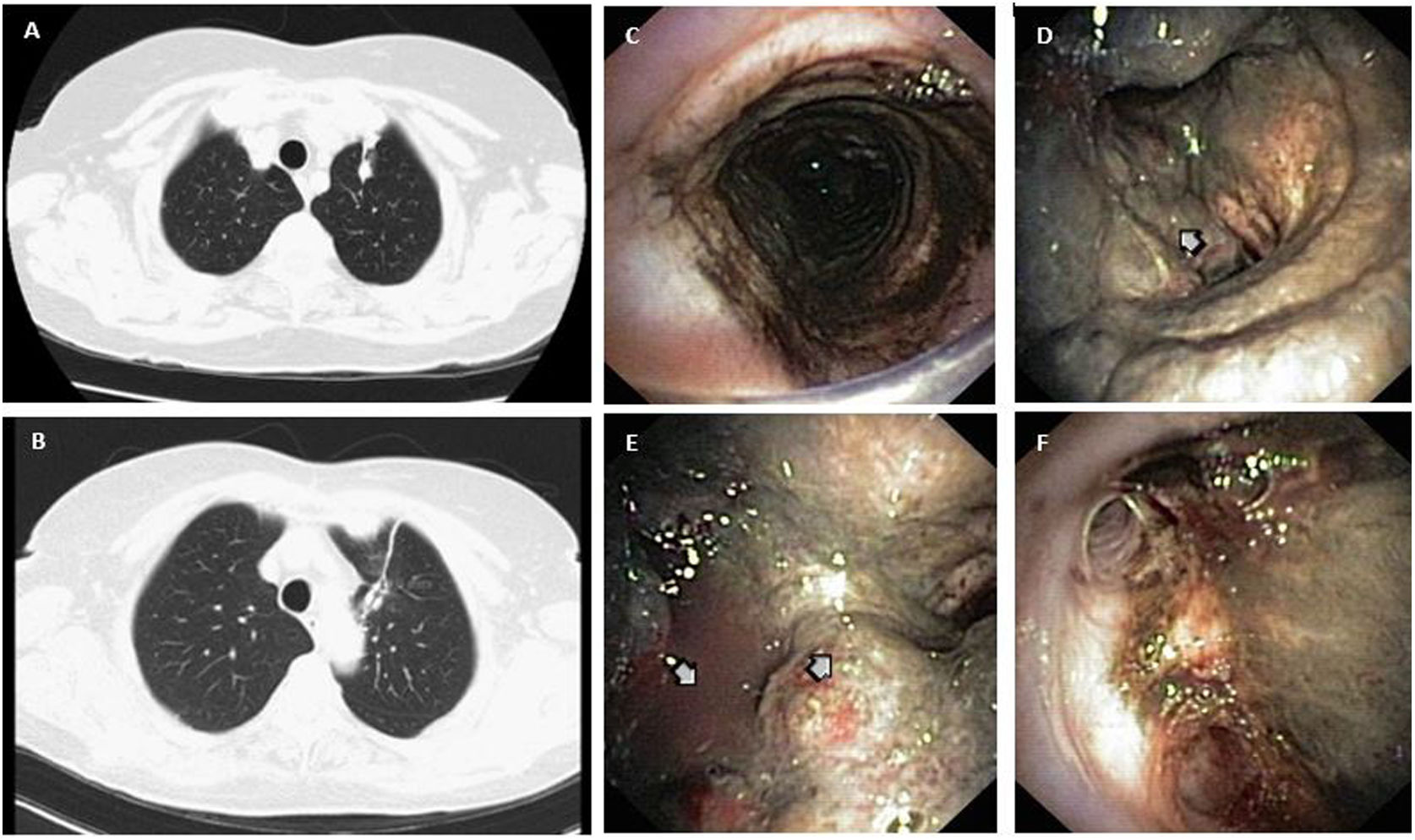
A 76-year-old non-smoking woman presented with malignant melanoma pulmonary recurrence (Fig. 1A and B). CT/PET-scan showed 18-FDG uptake adjacent to the previous surgical suture. The patient presented chronic productive cough without hemoptysis. CT-scan was performed 3 months before the proposed upper-left lobectomy and showed no central airway lesions. During anesthetic induction, progression of a double lumen endobronchial tube was difficult and ventilation was impossible and black material was aspirated through a probe. Flexible bronchofibroscopy was performed showing exuberant and extensive black pigmented mucosal infiltration, starting from the subglottic trachea and reaching almost the entire tracheobronchial tree. Tracheal and bronchial friable masses were visible, invading the carina and the left main bronchus (Fig. 1C–F). Patient was deemed inoperable and bronchial biopsy confirmed melanoma metastasis.
Melanoma metastases comprise 4.5% of all endobronchial metastases1 and are associated with poor prognosis,2 with 6 month overall median survival.1 Melanoma cannot be regarded as cured even after long disease-free periods, specially when thick primary tumors or metastatic disease. Bronchoscopic biopsy can establish the diagnosis of endobronchial metastases1 and should be performed before lung surgery of metastatic melanoma, especially if recurring and when there is a suspicion of progression to endobronchial disease.