Pulmonary endarterectomy (PE) is the treatment of choice for chronic thromboembolic pulmonary hypertension (CTEPH). The aim of this study was to analyze our experience in the medical and surgical management of CTEPH.
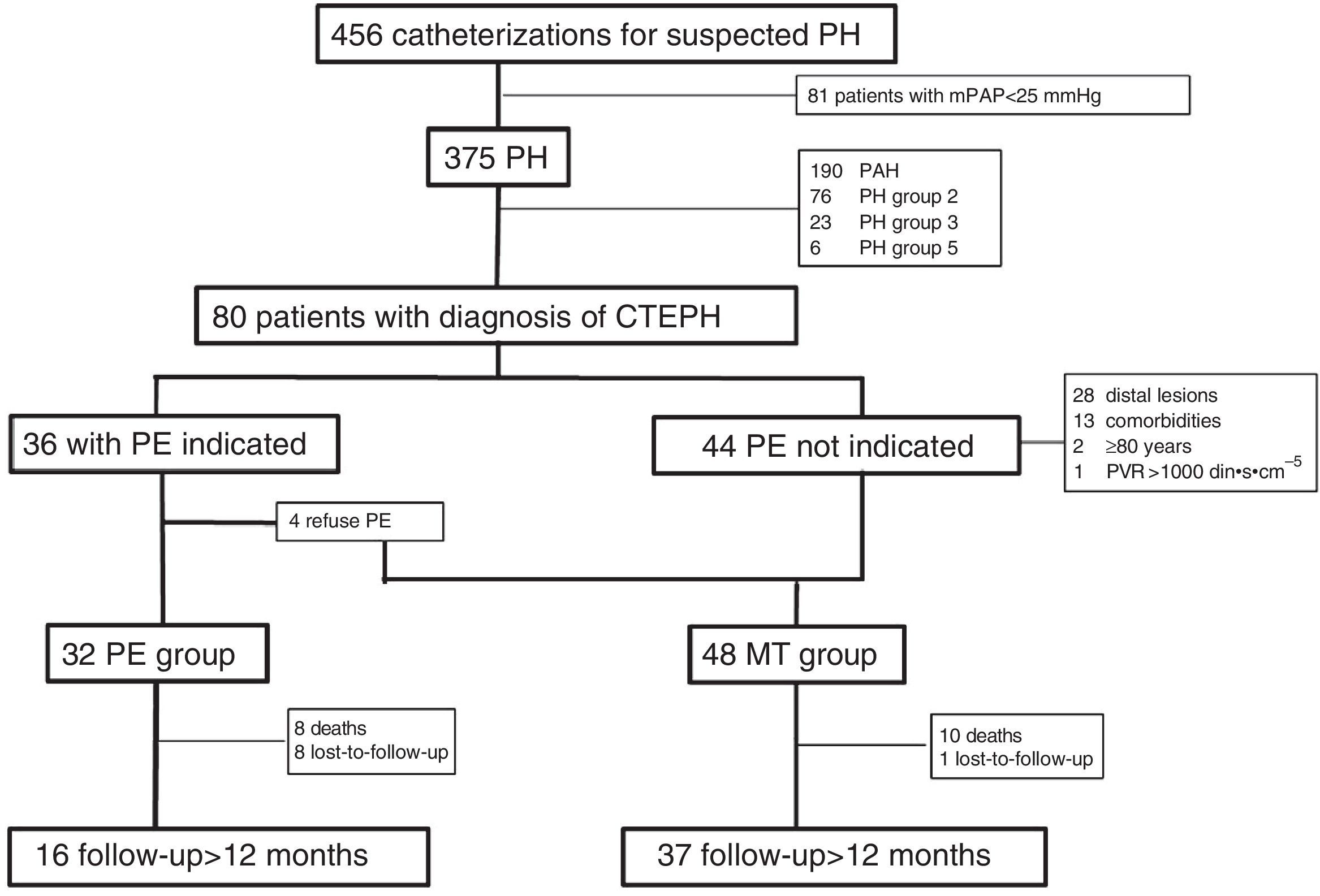
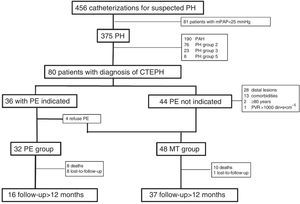
MethodsWe included 80 patients diagnosed with CTEPH between January 2000 and July 2012. Thirty-two patients underwent PE and 48 received medical treatment (MT). We analyzed functional class (FC), 6-min walking distance (6MWD), and pulmonary hemodynamics. Mortality in both groups and periods were analyzed.
ResultsPatients who underwent PE were younger, mostly men, and had longer 6MWD. No differences were observed in pulmonary hemodynamics or FC at diagnosis. One year after treatment, all PE patients versus 41% in MT group were at FC I–II. At follow-up, the PE group showed greater increase in 6MWD, and greater reduction in mean pulmonary arterial pressure and pulmonary vascular resistance than the MT group (P<.05). Overall survival in the MT group at 1 and 5years was 83% and 69%, respectively. Conditional survival in patients alive 100days post-PE at 1 and 5years was 95% and 88%, respectively. Surgical mortality in operated patients in the first period (2000–2006) was 31.3%, and 6.3% in the second (2007–2012).
ConclusionsPE provides good clinical results, and improves pulmonary hemodynamics in patients who successfully overcome the immediate postoperative period. After a learning period, the current operatory mortality in our center is similar to international standards.
La endarterectomía pulmonar (EP) es el tratamiento de elección para la hipertensión pulmonar tromboembólica crónica (HPTEC). El objetivo del estudio fue analizar nuestra experiencia en el tratamiento médico (TM) y quirúrgico de la HPTEC.
MétodosSe evaluaron 80 pacientes diagnosticados de HPTEC en el periodo enero 2000-julio 2012. En 32 casos se realizó EP, el resto recibió TM. Se analizaron: clase funcional (CF), distancia recorrida en seis minutos (PM6M) y hemodinámica pulmonar. Se analizó la mortalidad según el tratamiento y el periodo.
ResultadosLos pacientes del grupo EP eran más jóvenes, mayoritariamente hombres y recorrieron mayor distancia en la PM6M. No hubo diferencias hemodinámicas ni de CF al diagnóstico. Al año del tratamiento, el 100% del grupo EP y el 41% del grupo TM estaban en CF I-II. Al seguimiento, el grupo EP presentó mayor incremento en la PM6M y mayor reducción de la PAPm y la RVP que en el grupo TM (p<0,05). La supervivencia global del grupo TM a 1 y 5años fue del 83% y del 69%, respectivamente. La supervivencia condicionada de los pacientes vivos 100días post-EP a 1 y 5años fue del 95 y del 88%, respectivamente. La mortalidad quirúrgica en los pacientes operados en el período 2000-2006 fue del 31,3%, y en el período 2007-2012, del 6,3%.
ConclusionesLa EP proporciona buenos resultados clínicos, hemodinámicos y de supervivencia en los pacientes que superan satisfactoriamente el postoperatorio inmediato. Tras un periodo de aprendizaje, la mortalidad perioperatoria actual en nuestro centro es superponible a los estándares internacionales.
Chronic thromboembolic pulmonary hypertension (CTEPH) is a severe form of pulmonary hypertension (PH) associated with high levels of morbidity and mortality if not appropriately treated.1,2
In most patients who present with an episode of acute pulmonary embolism, clots resolve completely. However, between 0.9% and 3.8% develop CTEPH.3 Nevertheless, the real incidence of CTEPH may be greater, since a significant proportion of CTEPH patients have no prior history of acute pulmonary embolism.4–8 In the Spanish Pulmonary Arterial Hypertension Registry (REHAP) the prevalence of CTEPH was 3.2 cases per million adults, and the incidence was 0.9 cases per million adults/year.9 These figures are lower than in the United Kingdom, where an incidence of 1.75 cases per million adults/year has been reported.10
Survival of patients with CTEPH is closely related with the severity of PH and is similar to that of idiopathic pulmonary arterial hypertension (PAH).9 More than half of patients with mean pulmonary arterial pressure (mPAP) over 50mmHg do not live longer than 1 year after diagnosis.9,11
Pulmonary endarterectomy (PE) is the treatment of choice for CTEPH.2 The procedure is potentially curative and significantly improves symptoms and pulmonary hemodynamics.12 The procedure is performed in just a few specialized centers throughout the world, and mortality rates in the immediate post-operative period range between 4% and 24%.13–15 Post-operative mortality is related with the site of the clots, hemodynamic severity, experience of the medical and surgical teams, and comorbidities.16 A significant proportion of patients with CTEPH cannot be considered candidates for surgery, either because of comorbidities that greatly increase surgical risk or inaccessible thrombotic lesions.17 Clinical practice guidelines advise the administration of medical treatment (MT) with specific drugs for PH in these cases,2 although current evidence for efficacy is sparse.18,19 Very little data is available on the long-term progress of CTEPH patients treated with PE or MT.
PE is regularly performed in only 2 centers in Spain, the Hospital 12 de Octubre, Madrid20 and the Hospital Clínic, Barcelona, where this procedure was performed for the first time in Spain.21
The aim of this study was to analyze and report the experience in the MT and surgical treatment of CTEPH in patients consecutively diagnosed in the Hospital Clínic of Barcelona, and to describe their short- and long-term survival.
MethodsProspective observational cohort study to analyze the outcomes of MT and surgical intervention in patients with CTEPH.
Between January 2000 and July 2012, a total of 80 patients were diagnosed with CTEPH. A PH diagnostic algorithm was used for all patients in our unit.22 Patients in whom scintigraphy findings were highly suggestive of pulmonary thromboembolism were evaluated by computed tomography angiogram and digital subtraction angiography to ascertain the site and surgical accessibility of the thrombotic lesions. In the same procedure, pulmonary hemodynamics was determined by right heart catheterization and acute vasodilator test with inhaled nitric oxide (NO). Diagnosis of CTEPH was established on the basis of the following criteria:
- (1)
Evidence of precapillary PH: pulmonary arterial pressure (mPAP) ≥25mmHg and pulmonary wedge pressure (PWP) ≤15mmHg.
- (2)
Perfusion defects in pulmonary scintigraphy and/or thrombotic lesions in computed tomography angiogram of the chest.
- (3)
Persistent perfusion defects or thrombotic lesions after 3 months of appropriate anticoagulation.
After confirmation of the thromboembolic origin of PH, thrombophilia testing was performed, functional class (FC) was determined, and exercise tolerance was quantified with a 6-min walking test (6MWT).
Selection of Candidates for Pulmonary EndarterectomyA multidisciplinary team, made up of pulmonologists, surgeons, cardiologists, anesthetists, radiologists, and intensive medicine specialists studied the viability of surgery. The decision to operate was based on FC, accessibility of thrombotic lesions, hemodynamic status, and comorbidities.
Surgical Technique and Post-operative PeriodAn inferior vena cava filter was placed in all patients before surgery.
The surgical procedure was performed according to the technique described by Jamieson23 and all extracted material was sent for pathological examination. The technique consisted of bilateral PE performed via median sternotomy with extracorporeal circulatory support and periods of intermittent hypothermic circulatory arrest.24
After anesthetic induction, a Swan-Ganz catheter was placed in the pulmonary artery and a transesophageal echocardiogram transducer was introduced. Patients were ventilated mechanically with orotracheal intubation in the operating room and subsequently in the intensive care unit (UCI) for 12–48h. In the immediate post-operative period, patients received treatment with intravenous diuretics, proton pump inhibitors, and antibiotic prophylaxis. They were also anticoagulated with intravenous sodium heparin in the absence of significant bleeding. Until 2009, inhaled NO was used systematically in the immediate post-operative period in all operated patients. Later, it was used only in patients with residual post-operative PH.
Treatment of Non-surgical PatientsPatients classified as inoperable or who refused surgery began MT with calcium antagonists or specific anti-PH drugs (Fig. 1).
Follow-upPatients were called for a visit to the dedicated PH clinic in our center after 30 days, 3 months, and then every 3 months after hospital discharge, in the case of patients who underwent PE, or after diagnosis for TM patients.
Pulmonary hemodynamics after PE was reassessed on discharge in 8 patients and in 16 patients between 6 and 24 months after surgery. Follow-up hemodynamic evaluations were not performed systematically in all non-surgical patients. In cases with poor progress after starting MT or if a poor prognosis was determined from diagnostic catheterization (24 patients), hemodynamic testing was repeated 6–24 months later. In all cases, survival, FC, and exercise tolerance (6MWT) at 12 months were determined.
Statistical AnalysisThe following data were included in the analysis: demographic data, pre-operative or pre-MT data (FC, distance walked on 6MWT, and hemodynamics), post-operative variables (length of ICU stay in days, hours of mechanical ventilation, and morbidity), and follow-up data (mortality, and the same clinical and hemodynamic data as collected in the pre-operative period).
In order to separate mortality associated with surgery from disease-associated mortality, a conditional survival analysis was performed in patients alive 100 days after PE. In addition, with the aim of evaluating the effect of experience on perioperative mortality, survival in an initial period from 2000 to 2006 and in a second period from 2007 to 2012 were analyzed separately. Continuous variables are presented as mean±standard deviation (SD) or median and interquartile range (IQR), depending on whether distribution was normal or not. Categorical variables are presented as absolute values and percentages (%). Quantitative variables were analyzed using the Student's t-test or the Mann–Whitney U-test, depending on whether distribution was normal or not. Association between categorical variables was analyzed using the Chi-squared test or Fisher's exact test. Survival curves were calculated using the Kaplan–Meier method. Comparison of survival between groups was carried out using the log-rank test.
A P-value <.05 was considered statistically significant. All statistical analyses were performed using SPSS 18.0 software (SPSS Inc., Chicago, IL).
ResultsPopulation CharacteristicsThe study population was formed of 80 patients with consecutive diagnoses of CTEPH in the period between January 2000 and July 2012, with minimum follow-up of 6 months (Fig. 1). Thirty-three patients (41.3%) were men, and the mean age was 57±16 years. A total of 74% of patients presented FC III–IV, while 21% had a history of syncope and 37% had signs of right heart failure. At the time of diagnosis, mean distance walked on the 6MWT was 352±123m.
A total of 38% of patients had a history of deep venous thrombosis and 23% showed thrombophilia, lupus anticoagulant being the most common factor (15%).
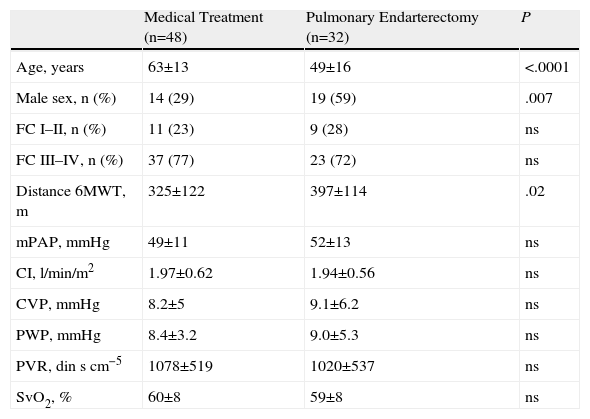
Pulmonary EndarterectomyA total of 36 patients (45%) were considered candidates for PE, of which 32 finally underwent the procedure (PE group) (Fig. 1). In comparison with the group that received only MT, patients in the PE group were younger and predominantly male (Table 1). The proportion of patients with FC III–IV was similar and the PE group achieved greater distances on the 6MWT. Both groups had a similar hemodynamic profile.
Patient Characteristics at Diagnosis.
| Medical Treatment (n=48) | Pulmonary Endarterectomy (n=32) | P | |
| Age, years | 63±13 | 49±16 | <.0001 |
| Male sex, n (%) | 14 (29) | 19 (59) | .007 |
| FC I–II, n (%) | 11 (23) | 9 (28) | ns |
| FC III–IV, n (%) | 37 (77) | 23 (72) | ns |
| Distance 6MWT, m | 325±122 | 397±114 | .02 |
| mPAP, mmHg | 49±11 | 52±13 | ns |
| CI, l/min/m2 | 1.97±0.62 | 1.94±0.56 | ns |
| CVP, mmHg | 8.2±5 | 9.1±6.2 | ns |
| PWP, mmHg | 8.4±3.2 | 9.0±5.3 | ns |
| PVR, dinscm−5 | 1078±519 | 1020±537 | ns |
| SvO2, % | 60±8 | 59±8 | ns |
FC: functional class; CI: cardiac index; CVP: central venous pressure; mPAP: mean pulmonary arterial pressure; 6MWT: 6-min walking test; PWP: pulmonary wedge pressure; PVR: pulmonary vascular resistance; SvO2: mixed venous oxygen saturation; ns: not significant.
Mean±SD or n (%).
Fourteen patients (43.7%) were operated without preconditioning treatment, while 18 (56.3%) underwent presurgical preconditioning to reduce pulmonary vascular resistance (PVR). These treatments included endothelin receptor antagonists (ERAs) (27.8%), phosphodiesterase-5 (PDE-5) inhibitors (22.2%), prostanoids (11.1%), calcium antagonists (11.1%), and combined therapy (27.8%).
During PE, median excorporeal circulation time was 152min (IQR 139–180) and median circulatory arrest time was 24min (IQR 16–36). After intervention, median mechanical ventilation time was 2 days (IQR 1–21), ICU stay was 8 days (IQR 7–22), and total hospital stay was 17 days (IQR 11–26).
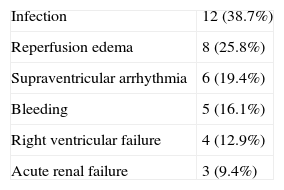
Main post-operative complications included infection (38.7%), the most common being pneumonia, reperfusion edema (25.8%), and supraventricular arrhythmias (19.4%) (Table 2). In the PE group, 33% presented post-operative residual PH, with an mPAP of 37±7mmHg.
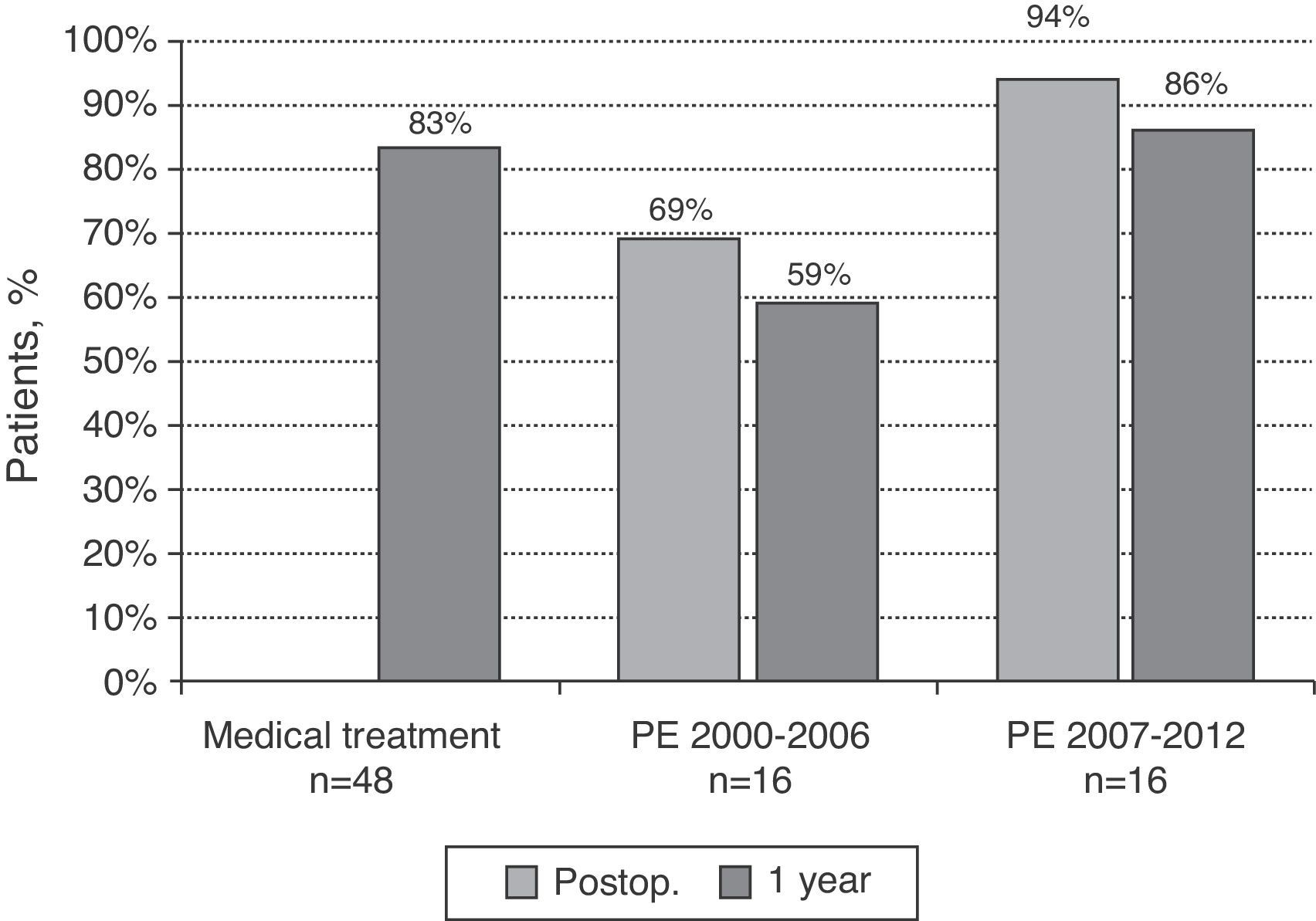
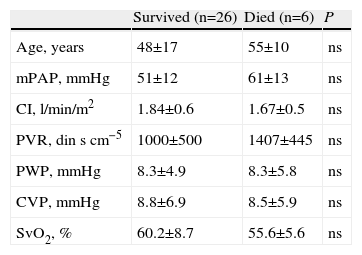
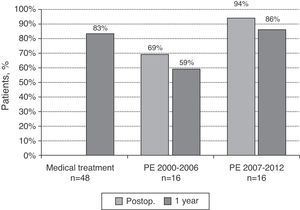
Six patients (18.8%) died in the immediate post-operative period. Patients who died had a poorer hemodynamic profile than survivors, although the differences were not statistically significant (Table 3). When broken down by periods, surgical mortality in the PE group between 2000 and 2006 was 5 out of 16 cases (31.3%), while in patients operated between 2007 and 2012, the mortality rate was 1 out of 16 patients (6.3%).
Characteristics of Patients Who Died After Pulmonary Endarterectomy.
| Survived (n=26) | Died (n=6) | P | |
| Age, years | 48±17 | 55±10 | ns |
| mPAP, mmHg | 51±12 | 61±13 | ns |
| CI, l/min/m2 | 1.84±0.6 | 1.67±0.5 | ns |
| PVR, dinscm−5 | 1000±500 | 1407±445 | ns |
| PWP, mmHg | 8.3±4.9 | 8.3±5.8 | ns |
| CVP, mmHg | 8.8±6.9 | 8.5±5.9 | ns |
| SvO2, % | 60.2±8.7 | 55.6±5.6 | ns |
CI: cardiac index; CVP: central venous pressure; mPAP: mean pulmonary arterial pressure; PWP: pulmonary wedge pressure; PVR: pulmonary vascular resistance; SvO2: mixed venous oxygen saturation; ns: not significant.
Mean±SD.
Patients unsuitable for surgery and who refused the procedure (Fig. 1) were treated with specific PH drugs or with calcium antagonists (MT group). The most commonly used specific PHA drugs were ERAs (49%), followed by PDE inhibitors (31%). Only 1 patient needed to receive combined therapy with 2 specific drugs (prostanoids and PDE inhibitors). Three patients were included in a clinical trial in which they initially received riociguat or placebo for 4 months, followed by riociguat. Patients with a vasodilator response classified as positive on pulmonary vascular reactivity testing began treatment with calcium antagonists (10%). Two patients in the MT group were evaluated for transplant, although the procedure was ultimately ruled out.
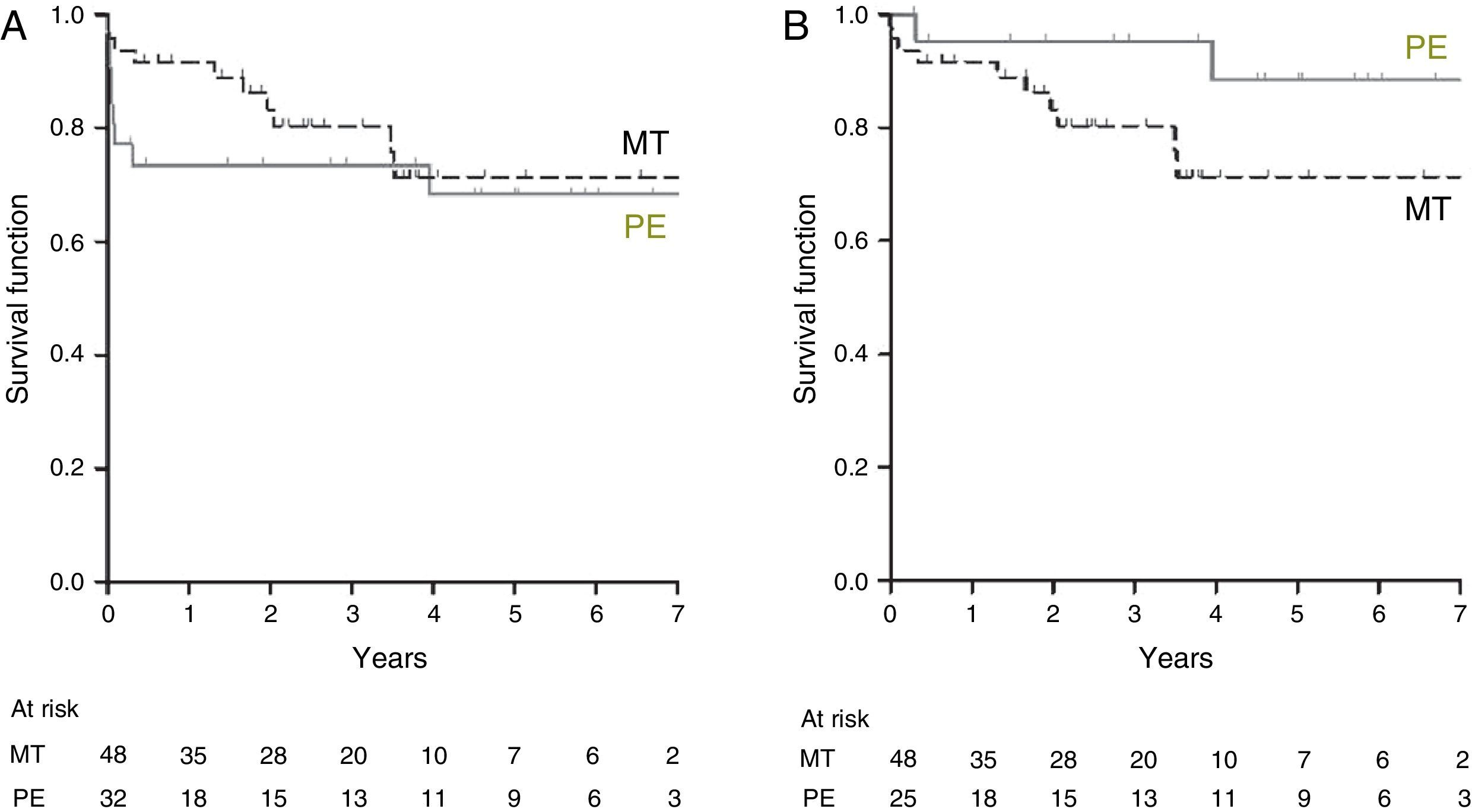
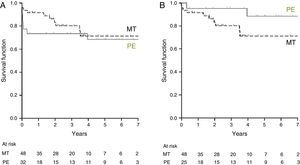
Long-term ResultsOverall 1-, 3-, and 5-year survival in the MT group was 83%, 69%, and 69%, respectively, and in the PE group it was 72%, 67%, and 67%, respectively (Fig. 2A). Conditional survival in patients in the PE group (those alive 100 days after intervention) was 95% at 1 year and 88% at 5 years (Fig. 2B). Patients undergoing PE between 2000 and 2006 had an immediate survival rate of 69%, and a 1-year survival rate of 59%. In patients operated between 2007 and 2012, immediate survival was 94% and 1-year survival was 86% (Fig. 3).
Survival (Kaplan–Meier) of patients with chronic thromboembolic pulmonary hypertension treated with pulmonary endarterectomy (PE) (solid line) or medical treatment (MT) (dashed line). Figure A shows overall survival of the PE group. Figure B shows conditional survival (patients alive 100 days after intervention) in the PE group.
Survival of patients with chronic thromboembolic pulmonary hypertension receiving medical treatment (MT) or pulmonary endarterectomy (PE). The latter group was analyzed in 2 parts: patients operated in the 2000–2006 period and patients operated in the 2007–2012 period. One-year survival results for all groups and immediate postoperative (postop.) survival in patients undergoing PE are shown.
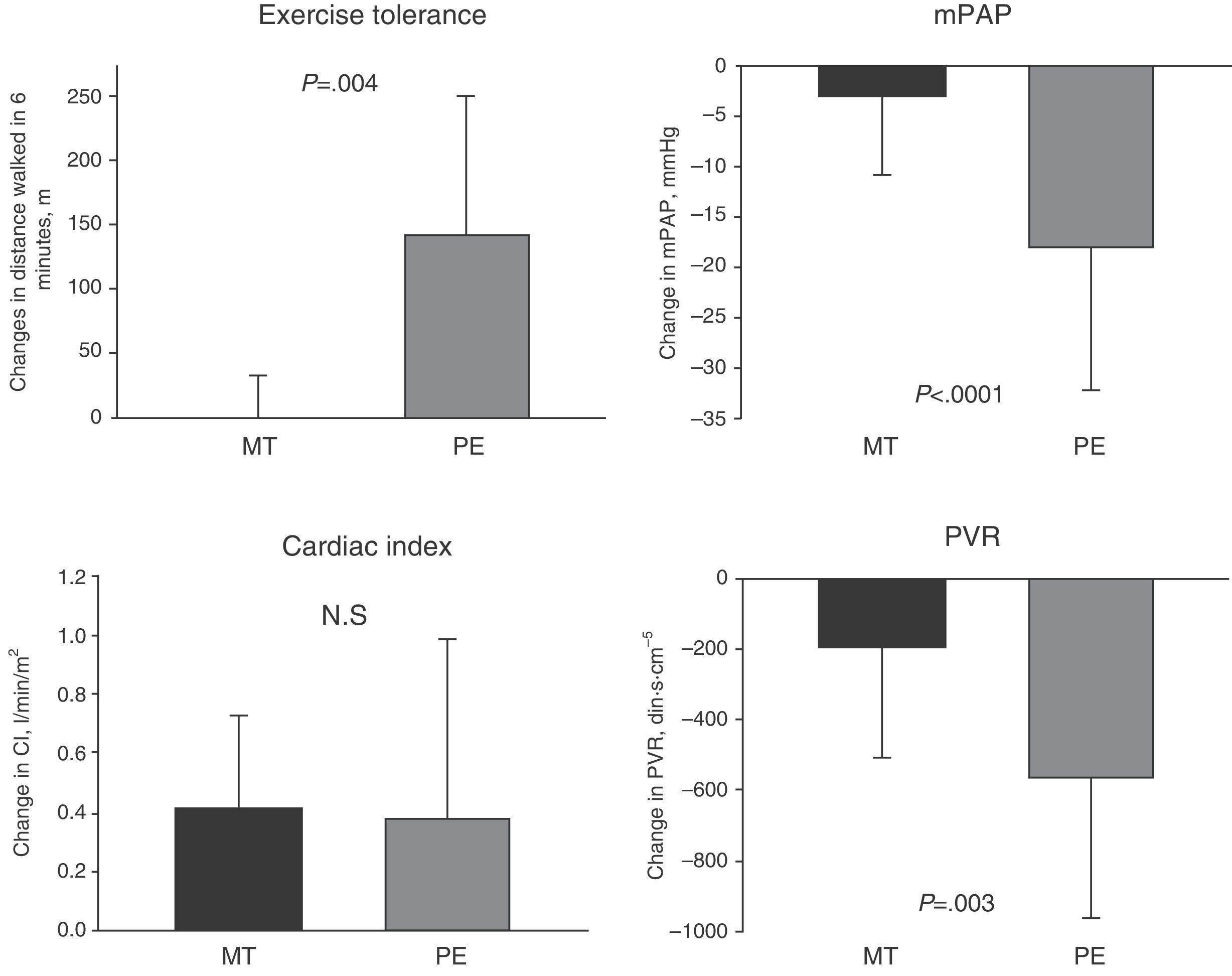
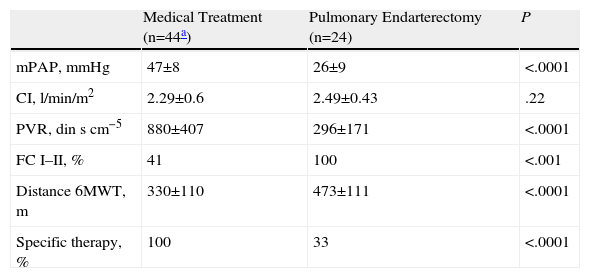
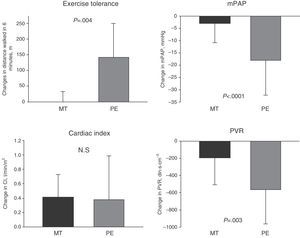
The clinical course of the PE group and the MT group is summarized in Table 4, showing that all patients in the PE group presented FC I–II and achieved a greater distance in the 6MWT. Compared with pre-treatment values (in both PE and MT), a greater increase in the distance covered in the 6MWT and greater reduction in mPAP and PVR were seen in the PE group, compared to the MT group (Fig. 4).
Long-term Progress.
| Medical Treatment (n=44a) | Pulmonary Endarterectomy (n=24) | P | |
| mPAP, mmHg | 47±8 | 26±9 | <.0001 |
| CI, l/min/m2 | 2.29±0.6 | 2.49±0.43 | .22 |
| PVR, dinscm−5 | 880±407 | 296±171 | <.0001 |
| FC I–II, % | 41 | 100 | <.001 |
| Distance 6MWT, m | 330±110 | 473±111 | <.0001 |
| Specific therapy, % | 100 | 33 | <.0001 |
FC: functional class; CI: cardiac index; mPAP: mean pulmonary arterial pressure; 6MWT: 6-min walking test; PVR: pulmonary vascular resistance.
Mean±SD or n (%).
Changes in follow-up (6–24 months) in patients with chronic thromboembolic pulmonary hypertension receiving medical treatment (MT) or pulmonary endarterectomy (PE): distance walked in 6min in meters (m), mean pulmonary arterial pressure (mPAP), cardiac index, and pulmonary vascular resistance (PVR).
Only 33% of the operated patients had residual pulmonary hypertension requiring specific therapy.
DiscussionThe results of analysis of CTEPH activity in our center highlight the good therapeutic outcome of PE, which gives better results than MT in patients who successfully overcome the immediate post-operative period. Mortality in the immediate post-operative period fell significantly in the second period of activity, and is now within international standards.12
PE outcomes in patients with CTEPH have not been evaluated in controlled clinical trials, and there is little information available on this approach compared to MT.10 In any event, the long-term outcomes reported, in terms of functional capacity, pulmonary hemodynamics and survival, make PE the treatment of choice in these patients.2,25
Our results show clear clinical improvement in exercise capacity and pulmonary hemodynamics 1 year after PE. Improvement was also observed in the MT group, but of a smaller magnitude. These results are consistent with other national and international registries.10,12,20,26
In all, 40% of patients in whom PE was indicated finally underwent the procedure. This figure is slightly lower than the 57% reported by an international prospective PE survey carried out in 26 European centers and 1 center in Canada,12 but higher than the 30% reported in all Spanish centers, according to the REHAP data registry.9 The main causes of inability to operate were related with inaccessibility of thrombotic lesions and comorbidities.
Firm evidence that PE gives highly satisfactory outcomes10,12 should encourage physicians to refer patients to centers with facilities for this procedure for pre-operative evaluation.2,12
As in other specialized sites,13,20,27 immediate post-operative survival after PE in our center improved in the second period of activity (2007–2012), reflecting the learning curve of our team in this and other complex surgical interventions, such as transplantation.28 This improvement correlates with our growing experience in clinical evaluation, the surgical procedure itself, and the post-operative management of the patient and of complications.
Analysis of conditional survival also shows that patients who successfully overcome the post-operative period show excellent long-term survival, consistent with the improved hemodynamics achieved with PE. Consequently, the reduction of mortality in the post-operative period, as a result of our greater experience, is having a positive impact in the long-term survival of our PE patients.
Drug Treatment of Chronic Thromboembolic Pulmonary HypertensionAt present, the indication of drug treatment in CTEPH is limited to (1) patients with residual PH after PE, and (2) patients not suitable for PE. These indications are based on expert recommendations,29 but there is little evidence of efficacy.18,19
In our center, 56% of patients considered suitable for surgery received specific therapy for PH in accordance with the recommendations in place during the study period2; this figure is similar to other studies.10 The aim of treatment was to reduce PVR before surgery, since a very high PVR (>1000dinscm−5) is one of the primary factors for reperfusion edema and adverse outcomes in the post-operative period.30 Some investigator groups are now advising against this preconditioning treatment because there is no evidence to support its efficacy and it may cause a delay in surgery.29,31
At the time of writing this article, no drug had yet been approved for the treatment of CTEPH in Spain, although the great majority of CTEPH patients considered unsuitable for surgery receive specific PH treatment,8,10,12 in accordance with clinical guidelines. In our center, 55% of patients were considered unsuitable for PE surgery, and specific treatment was administered to 90% of these cases. This indication is based on evidence of histological lesions indistinguishable from the typical lesions seen in patients with PAH.32 Data from specialized centers in the United Kingdom suggest that the prognosis of patients with inoperable CTEPH has improved in recent years.10 However, this initial functional improvement does not last beyond the first year after diagnosis. In our series of MT patients, a significant improvement was observed in functional capacity and in pulmonary hemodynamics 1 year after initiating specific therapy, although the values reached were lower than those observed in the PE group. These data are in line with those described by Condliffe et al.10
Long-term survival in patients considered inoperable who received medical treatment for PH in our series was similar to the rates reported by the U.K. group.10 However, long-term survival in MT patients was lower than conditional survival in the PE group and overall survival in the PE group operated during the second period of activity (2007–2012).
To conclude, analysis of the experience with CTEPH in our center confirms that PE provides clear hemodynamic improvements and better functional capacity in patients who successfully overcome the perioperative period; the disease can be cured in 67% of patients. After a learning period, the post-operative mortality rate in our center is currently within international standards.
These results, together with those previously reported by Blázquez et al.,18 should help increase the number of CTEPH patients undergoing PE in Spain. In accordance with current clinical guidelines, all patients with CTEPH should be offered the chance to be evaluated by an expert PE team, with the aim of identifying those who may benefit from this potentially curative treatment.
FundingThis project has been partially funded with an unconditional grant from Bayer S.L. M.L. Coronel and V. Amado have received a training grant from Pfizer S.L. N. Chamorro has received a grant from the Catalan Society of Pulmonology (SOCAP).
AuthorshipM.L. Coronel, N. Chamorro, and I. Blanco: data collection and recording, statistical analysis, interpretation of results, manuscript preparation.
Verónica Amado and R. del Pozo: data collection and recording, manuscript review.
J.L. Pomar, J.R. Badia, I. Rovira, P. Matute, G. Argemí, and M. Castellà: performance of clinical procedures in patients, analysis of results and manuscript review.
J.A. Barberà: study development and design, performance of clinical procedures in patients, interpretation of results and manuscript review.
All authors have reviewed the manuscript and are in agreement with its contents.
Conflict of InterestNone of the authors has any conflict of interests.
The authors thank Drs. M. Sánchez, P. Arguis, M. Burrel and M. Barrufet of the Radiodiagnostics Department for their invaluable help, and also the nursing staff from the Pulmonology Room, the Intensive Respiratory Care Unit, the Cardiovascular Specific Surgical Care Unit and Operating Room.
Please cite this article as: Coronel ML, Chamorro N, Blanco I, Amado V, del Pozo R, Pomar JL, et al. Tratamiento médico y quirúrgico de la hipertensión pulmonar tromboembólica crónica: experiencia en un único centro. Arch Bronconeumol. 2014;50:521–527.