EPOCONSUL is the first national audit to analyze medical care for COPD in pulmonology departments in Spain. The main objective was to perform a retrospective analysis to determine the distribution of GesEPOC 2017 COPD risk levels and to evaluate management according to the new recommendations.
Material and methodsThis is a cross-sectional clinical audit in which consecutive COPD cases were recruited over one year. The study evaluated risk and clinical phenotype according to GesEPOC 2017, and their correlation with the clinical interventions employed.
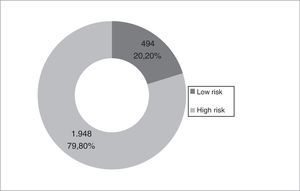
ResultsThe most common risk category was high risk (79.8% versus 20.2%; P<.001), characterized by a higher level of severity on BODE and BODEx indexes, and a higher comorbidity burden. The most common phenotype was non-exacerbator. The most commonly used treatment in low-risk patients was bronchodilator monotherapy (34.8%) and triple therapy in high-risk patients (53.7%). Patients with high risk were more requently classified according to their phenotype (57.6% versus 52%; P=.014) and had more frequently recorded pulmonary function tests: lung volume (47.7% versus 35.8%; P<.001), lung diffusion (51.4% versus 42.1%; P<.001) and walk test (37.8% versus 15.8%; P<.001).
ConclusionsMost patients treated in pulmonology departments were high-risk and non-exacerbator phenotype. Clinical interventions differed according to risk level and mainly followed GesEPOC recommendations, although there is significant room for improvement.
EPOCONSUL es la primera auditoría nacional que analiza la atención sanitaria de la EPOC en consultas de neumología en España. El objetivo principal fue determinar, en un análisis retrospectivo, la distribución de los niveles de riesgo de la EPOC según GesEPOC 2017 y evaluar las actuaciones clínicas según las nuevas recomendaciones.
Material y métodosEs una auditoría clínica de diseño trasversal, con reclutamiento de casos consecutivos de EPOC durante un año. Se evaluó el nivel de riesgo y el fenotipo clínico según GesEPOC 2017 y su relación con las intervenciones clínicas realizadas.
ResultadosEl nivel de alto riesgo fue más frecuente (79,8 versus 20,2%; p<0,001) y se caracterizó por un mayor nivel de gravedad medido por los índices BODE y BODEx, además de por mayor comorbilidad. El fenotipo clínico más frecuente fue el no agudizador. La opción más utilizada en el bajo riesgo fue la monoterapia broncodilatadora (en un 34,8%) y la triple terapia en el alto riesgo (en un 53,7%). En el alto riesgo fue más frecuente la caracterización por fenotipos (57,6 versus 52%; p=0,014) y la realización de pruebas de función respiratoria: volúmenes pulmonares (47,7 versus 35,8%; p<0,001), test de difusión (51,4 versus 42,1%; p<0,001) y test de marcha (37,8 versus 15,8%; p<0,001).
ConclusionesLa mayoría de los pacientes atendidos en las consultas de neumología fueron de alto riesgo y con fenotipo clínico no agudizador. La práctica clínica realizada fue diferente según el nivel de riesgo y mayoritariamente acorde con las recomendaciones de GesEPOC, aunque con importantes áreas de mejora.
Chronic obstructive pulmonary disease (COPD) is a complex disease that requires a comprehensive approach and a multidimensional evaluation that includes risk assessment. In recent years, multidimensional scales such as the BODE or BODEx1–3 have been proposed as alternatives to FEV1. These scales show improved prognostic value for predicting future complications, but their uptake in clinical practice is very low.4,5
Recent updates of clinical practice guidelines for the management of COPD have incorporated various proposals for the assessment of the disease based on scientific evidence and expert consensus, with the aim of delivering more personalized medicine.6–8
The latest edition of the Spanish COPD Guidelines (GesEPOC) responds to the need for better classification of patients in order to simplify risk stratification and determine appropriate levels of diagnostic and therapeutic intervention. GesEOPC proposes a new 2-level risk classification (low and high) that promotes simplified care programs for low-risk patients and greater diagnostic accuracy and more personalized treatment for high-risk patients. This new approach to classifying patients is supported by the medical literature, but to date the implications of its use in daily clinical practice have not been analyzed.
The EPOCONSUL study is the first national audit that analyzes COPD care in pulmonology clinics in Spain.6 In previous analyses, EPOCONSUL confirmed a high level of implementation of the 2012 version of the GesEPOC9: 46.3% of the clinical records audited included phenotype classification according to the GesEPOC criteria, although adherence to good clinical practice recommendations varied widely among the hospitals.6
In this study, we used the EPOCONSUL database to perform a retrospective analysis of the distribution of COPD risk levels and clinical phenotypes according to GesEPOC 2017, and to determine if medical care was delivered according to risk level, as recommended by these guidelines.
MethodologyThe methodology of the EPOCONSUL study has been described in detail elsewhere.6 Briefly, EPOCONSUL is a clinical audit sponsored by the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR). It is designed to assess clinical practice and clinical and organizational factors associated with the type of care delivered to COPD patients in pulmonology clinics in Spain. This was an observational, cross-sectional, prospective study conducted between May 2014 and May 2015. A total of 59 centers participated (33.7% of those potentially eligible) from 16 of the 17 Spanish autonomous communities (all except La Rioja). Most were university hospitals (83.1%) with 20 or more respiratory medicine beds (83.7%). Historic data from clinical records and associated documents together with current data related to hospital resources were collected. Forty-six variables associated with the hospitals and 153 associated with the patients were collected and divided into 3 groups: (1) available resources and workflow; (2) patient characteristics, and (3) clinical practice models, comprising actions taken during follow-up and in the last audited visit.
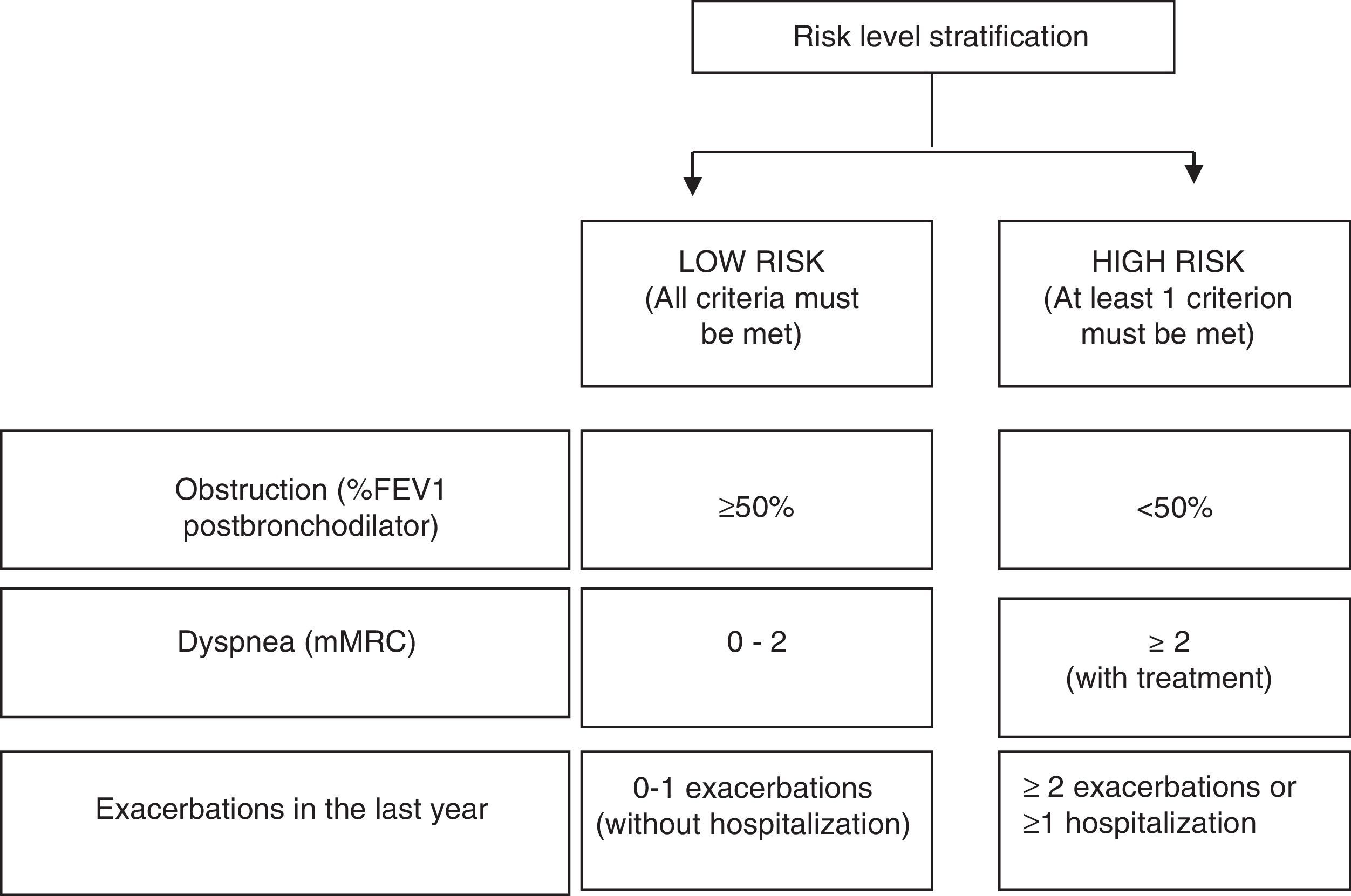
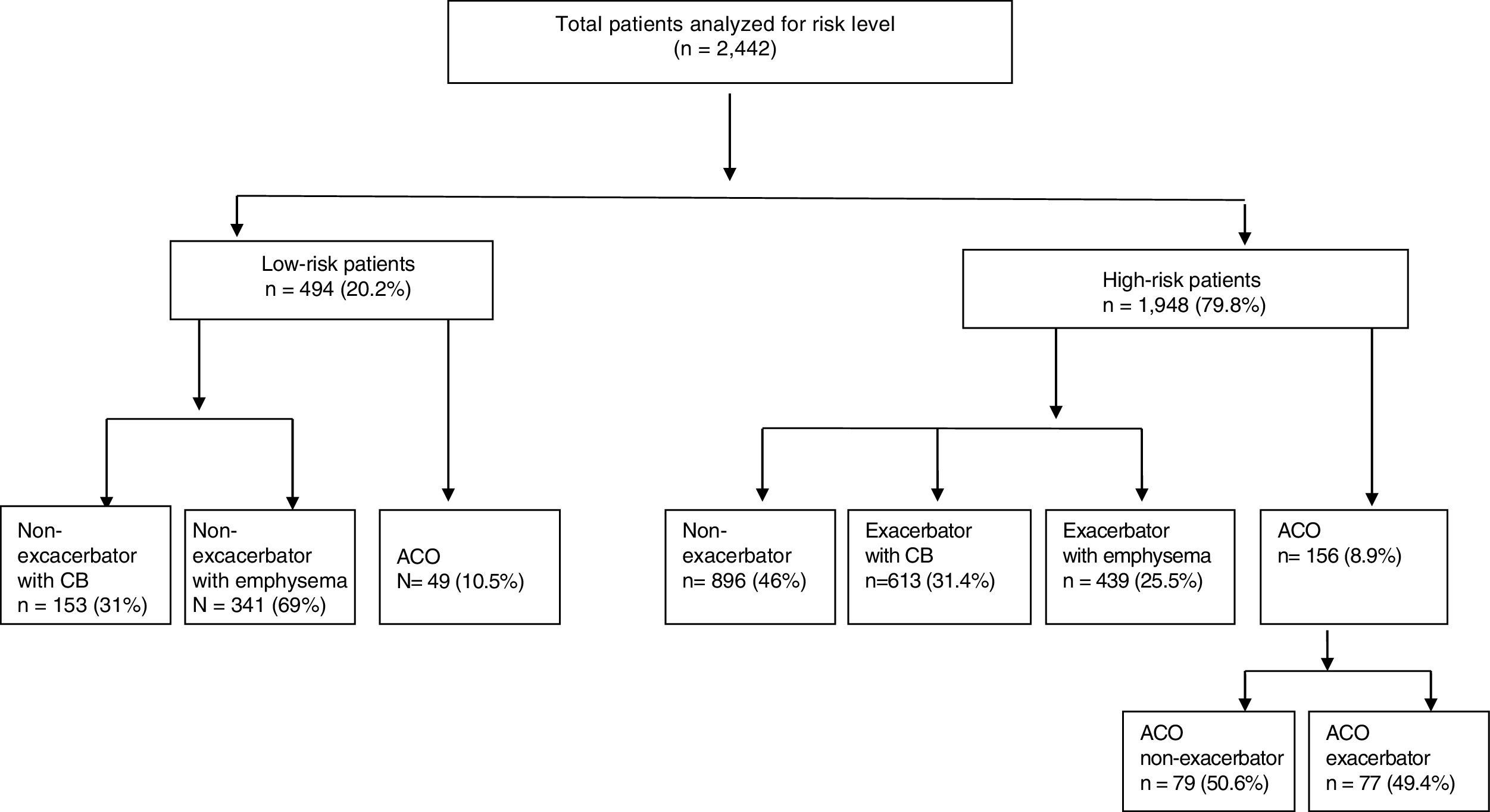
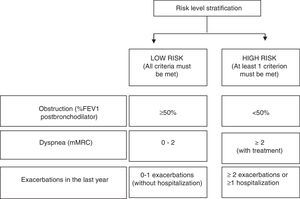
Risk groups in the retrospective analysis were established according to the level of risk, which was defined following the new GesEPOC functional (percent post-bronchodilator FEV1) and clinical (dyspnea grade and history of exacerbations) criteria8 described in Fig. 1. The clinical phenotype of COPD was also classified according to GesEPOC criteria, using the following algorithm: (1) patients with 0 or 1 exacerbation and no hospitalizations for exacerbation in the previous year were classified as non-exacerbators; (2) patients who had at least 2 exacerbations or 1 hospitalization in the previous year, with chronic cough and expectoration, were identified as exacerbators with chronic bronchitis; (3) patients who had at least 2 exacerbations or 1 hospitalization in the previous year without cough or sputum production, with clinical/radiological or functional evidence of exacerbation were classified as exacerbators with emphysema, and (4) patients with a concomitant diagnosis of bronchial asthma or COPD, or patients with clinical symptoms suggestive of asthma and a positive bronchodilator test greater than or equal to 15% were identified as asthma-COPD overlap (ACO) phenotype.
The protocol (C.I. 14/030-E) was approved by the Clinical Research Ethics Committee of the Hospital Clínico San Carlos (Madrid, Spain), who certified that it met the requirements of the Declaration of Helsinki on ethical principles for medical research and respected the confidentiality of the participating patients. The local Ethics Committee of each of the participating centers approved the protocol and authorized the study. The need for informed consent was waived due to the non-interventionist nature of the study, the anonymisation of the data, and the need for blind assessment of the clinical strategies. This was explained in the protocol and approved by the ethics committees. To avoid changes in routine clinical practice and to maintain the blind in the evaluation of clinical strategies, medical staff were not informed of the audit.
Statistical AnalysisThe statistical analysis was carried out using the IBM SPSS statistical package (IBM Corporation, Armonk, New York, USA), version 23.0. Quantitative variables were expressed as mean and standard deviation (SD), and median and interquartile range were presented for asymmetric continuous variables. Qualitative variables were expressed by absolute and relative frequency (percentage). The Chi-squared test was used to compare qualitative variables in the high and low risk groups. Quantitative variables in the 2 risk groups were compared using the Student's t test for symmetric variables, or the nonparametric Mann–Whitney U test for asymmetric variables. A logistic regression model was conducted to identify clinical and epidemiological factors independently associated with the risk level. All variables that were statistically significant in the univariate model were included in this model. In all tests of the hypothesis, the null hypothesis was rejected with a type I error or an α error of less than 0.05.
ResultsFifty-nine of the 175 Spanish National Health System hospitals with a pulmonology clinic, according to the Ministry of Health registry of 2012, participated in the study. The estimated reference population for the EPOCONSUL study was 18,104,350 individuals, representing 39% of the population of Spain. Participating hospitals and investigators are listed in Annex 1.
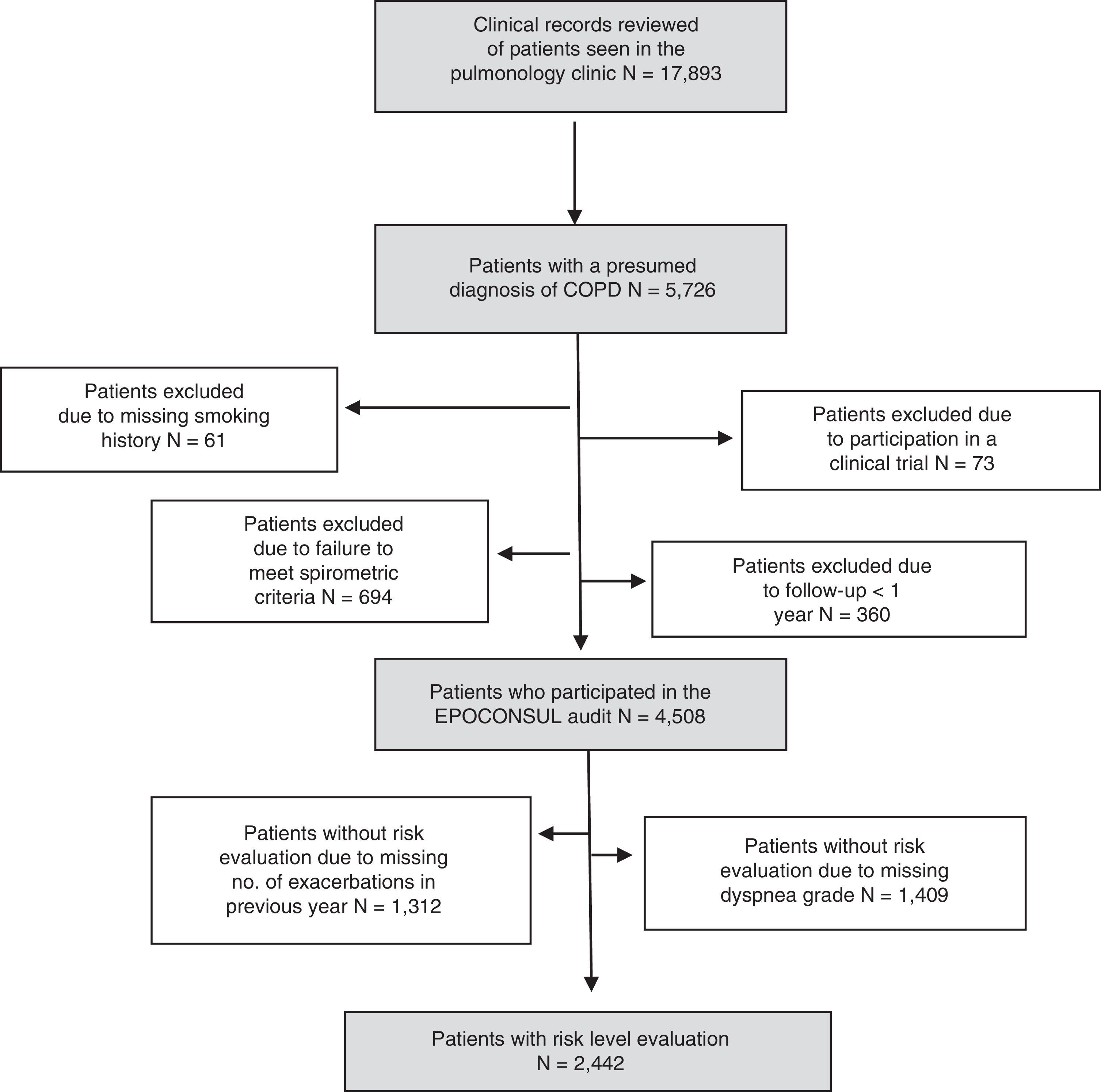
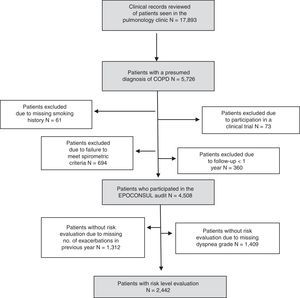
A total of 17,893 clinical records of patients seen the pulmonology clinic were evaluated during the study period, and of these, 4508 patients with a diagnosis of COPD who met the acceptability criteria were audited. Risk levels were analyzed in 2442 patients who presented all the GesEPOC criteria for defining these levels. The sampling process is described in a STROBE10 flow chart (Fig. 2).
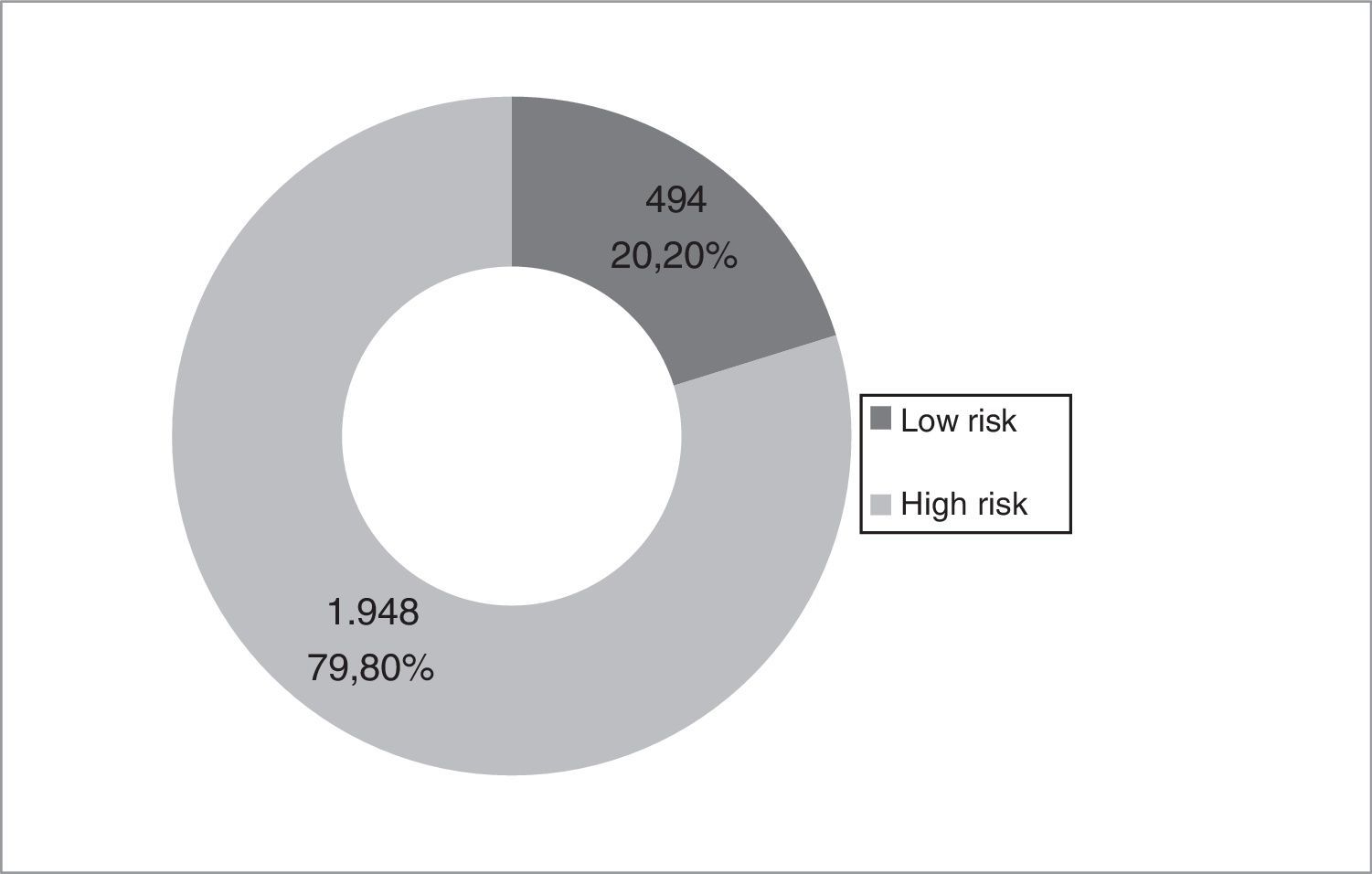
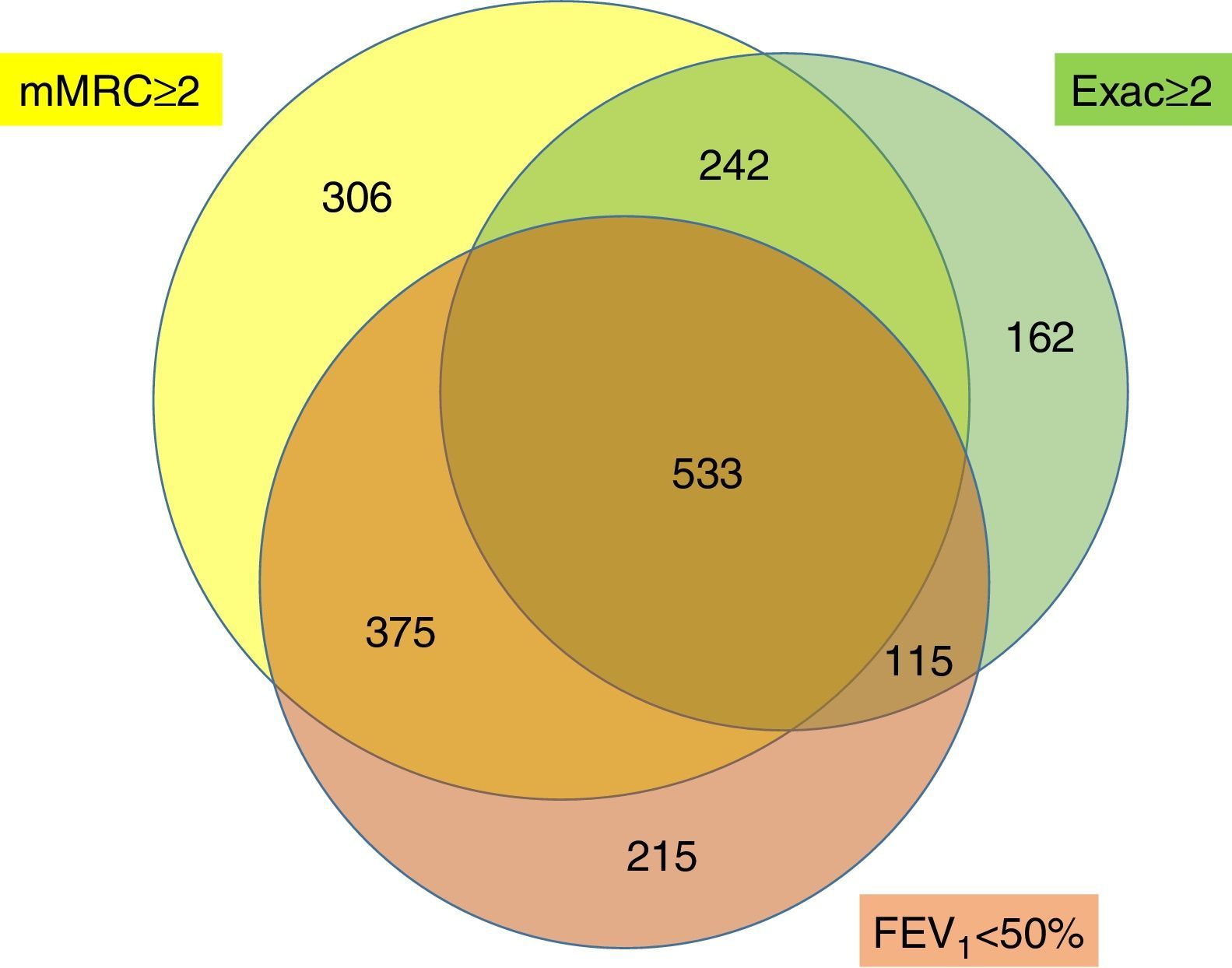
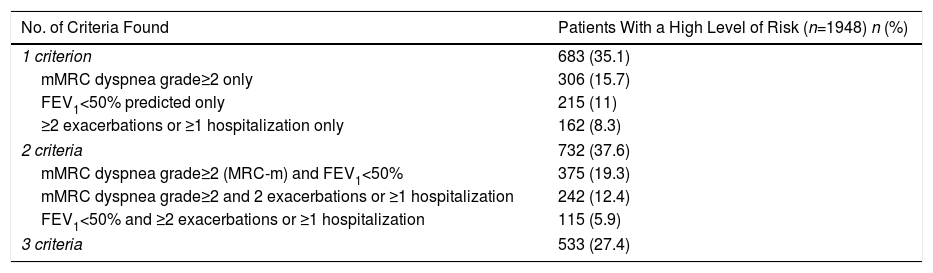
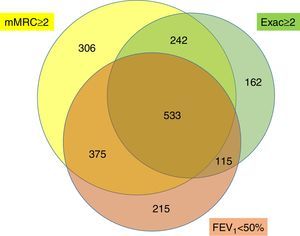
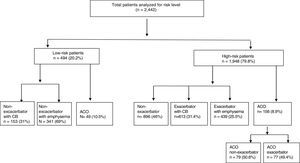
Distribution of Risk Levels and Demographic and Clinical CharacteristicsAmong the study cohort, 1948 (79.8%) patients were classified as high-risk and 494 (20.2%) as low-risk (Fig. 3). Table 1 shows the distribution of the criteria that defined patients as high-risk. In total, 27.4% of high-risk patients presented 3 criteria, and 35.1% presented a single criterion. The most common high-risk criterion was mMRC dyspnea grade≥2, and this was the only criterion detected in 15.7% of the high-risk patients. Fig. 4 shows a proportional Venn diagram of the criteria that define the high-risk level.
Distribution of High-risk Patients According to the Number of Criteria and the Criteria That Define Their High-risk Level.
| No. of Criteria Found | Patients With a High Level of Risk (n=1948) n (%) |
|---|---|
| 1 criterion | 683 (35.1) |
| mMRC dyspnea grade≥2 only | 306 (15.7) |
| FEV1<50% predicted only | 215 (11) |
| ≥2 exacerbations or ≥1 hospitalization only | 162 (8.3) |
| 2 criteria | 732 (37.6) |
| mMRC dyspnea grade≥2 (MRC-m) and FEV1<50% | 375 (19.3) |
| mMRC dyspnea grade≥2 and 2 exacerbations or ≥1 hospitalization | 242 (12.4) |
| FEV1<50% and ≥2 exacerbations or ≥1 hospitalization | 115 (5.9) |
| 3 criteria | 533 (27.4) |
FEV1: postbronchodilator FEV1 percent predicted; mMRC: modified Medical Research Council.
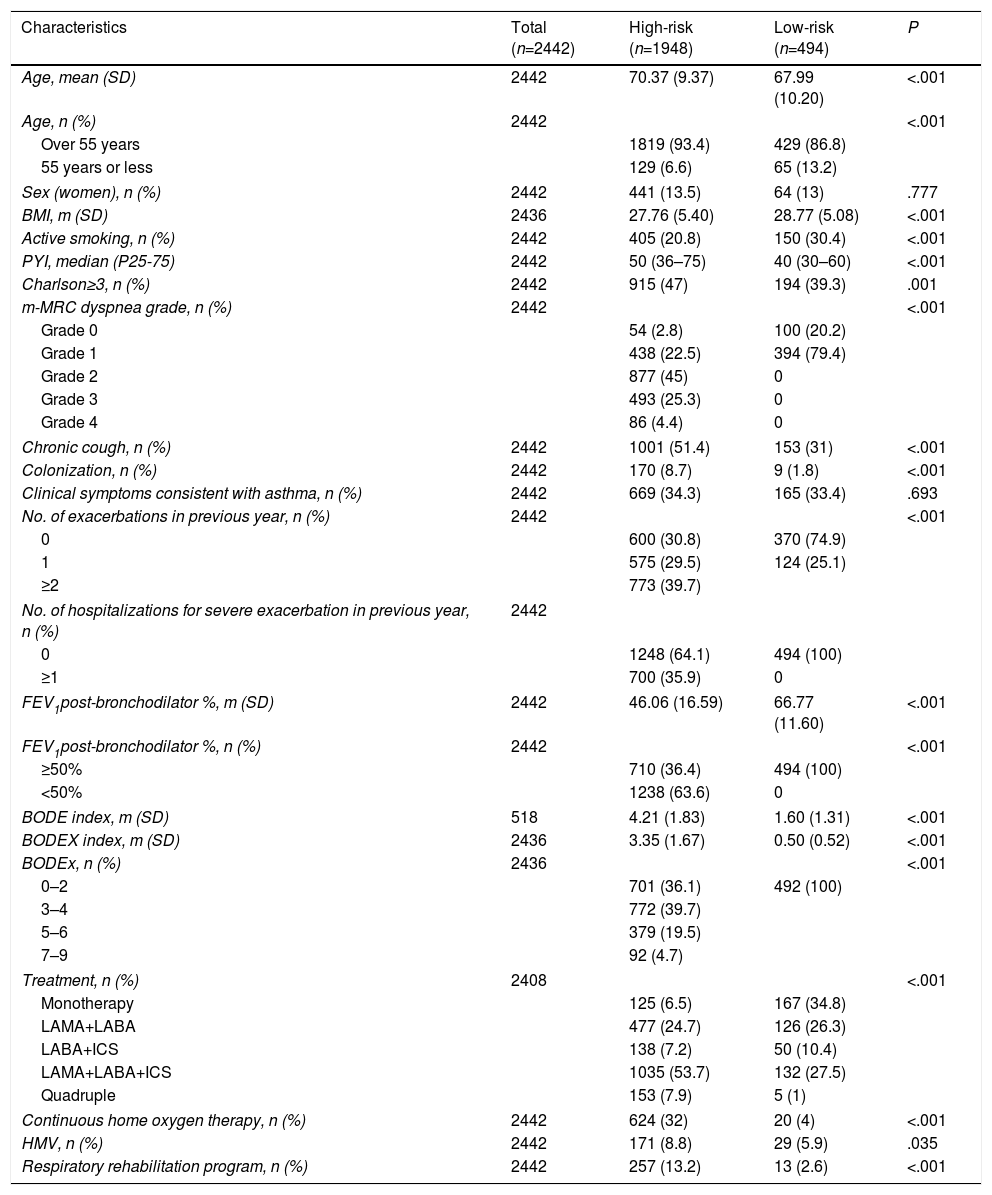
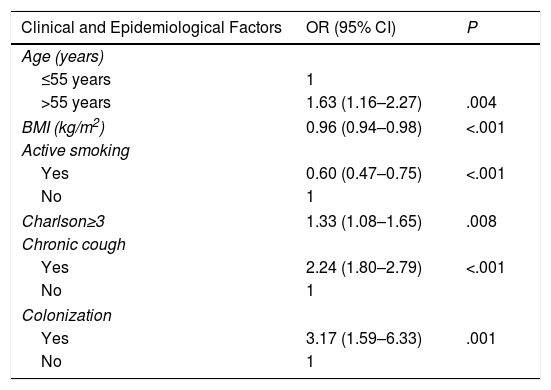
Demographic and clinical characteristics by risk level are shown in Table 2. Statistically significant differences were observed for all variables, except sex and clinical symptoms consistent with bronchial asthma. High-risk patients were characterized by their older age and greater comorbidity assessed by the Charlson index, and these factors were identified in the multivariate model (Table 3) as independently associated. In addition, high-risk patients had more severe disease, as assessed by the BODE and BODEx indices.
Clinical Characteristics According to GesEPOC Risk Level.
| Characteristics | Total (n=2442) | High-risk (n=1948) | Low-risk (n=494) | P |
|---|---|---|---|---|
| Age, mean (SD) | 2442 | 70.37 (9.37) | 67.99 (10.20) | <.001 |
| Age, n (%) | 2442 | <.001 | ||
| Over 55 years | 1819 (93.4) | 429 (86.8) | ||
| 55 years or less | 129 (6.6) | 65 (13.2) | ||
| Sex (women), n (%) | 2442 | 441 (13.5) | 64 (13) | .777 |
| BMI, m (SD) | 2436 | 27.76 (5.40) | 28.77 (5.08) | <.001 |
| Active smoking, n (%) | 2442 | 405 (20.8) | 150 (30.4) | <.001 |
| PYI, median (P25-75) | 2442 | 50 (36–75) | 40 (30–60) | <.001 |
| Charlson≥3, n (%) | 2442 | 915 (47) | 194 (39.3) | .001 |
| m-MRC dyspnea grade, n (%) | 2442 | <.001 | ||
| Grade 0 | 54 (2.8) | 100 (20.2) | ||
| Grade 1 | 438 (22.5) | 394 (79.4) | ||
| Grade 2 | 877 (45) | 0 | ||
| Grade 3 | 493 (25.3) | 0 | ||
| Grade 4 | 86 (4.4) | 0 | ||
| Chronic cough, n (%) | 2442 | 1001 (51.4) | 153 (31) | <.001 |
| Colonization, n (%) | 2442 | 170 (8.7) | 9 (1.8) | <.001 |
| Clinical symptoms consistent with asthma, n (%) | 2442 | 669 (34.3) | 165 (33.4) | .693 |
| No. of exacerbations in previous year, n (%) | 2442 | <.001 | ||
| 0 | 600 (30.8) | 370 (74.9) | ||
| 1 | 575 (29.5) | 124 (25.1) | ||
| ≥2 | 773 (39.7) | |||
| No. of hospitalizations for severe exacerbation in previous year, n (%) | 2442 | |||
| 0 | 1248 (64.1) | 494 (100) | ||
| ≥1 | 700 (35.9) | 0 | ||
| FEV1post-bronchodilator %, m (SD) | 2442 | 46.06 (16.59) | 66.77 (11.60) | <.001 |
| FEV1post-bronchodilator %, n (%) | 2442 | <.001 | ||
| ≥50% | 710 (36.4) | 494 (100) | ||
| <50% | 1238 (63.6) | 0 | ||
| BODE index, m (SD) | 518 | 4.21 (1.83) | 1.60 (1.31) | <.001 |
| BODEX index, m (SD) | 2436 | 3.35 (1.67) | 0.50 (0.52) | <.001 |
| BODEx, n (%) | 2436 | <.001 | ||
| 0–2 | 701 (36.1) | 492 (100) | ||
| 3–4 | 772 (39.7) | |||
| 5–6 | 379 (19.5) | |||
| 7–9 | 92 (4.7) | |||
| Treatment, n (%) | 2408 | <.001 | ||
| Monotherapy | 125 (6.5) | 167 (34.8) | ||
| LAMA+LABA | 477 (24.7) | 126 (26.3) | ||
| LABA+ICS | 138 (7.2) | 50 (10.4) | ||
| LAMA+LABA+ICS | 1035 (53.7) | 132 (27.5) | ||
| Quadruple | 153 (7.9) | 5 (1) | ||
| Continuous home oxygen therapy, n (%) | 2442 | 624 (32) | 20 (4) | <.001 |
| HMV, n (%) | 2442 | 171 (8.8) | 29 (5.9) | .035 |
| Respiratory rehabilitation program, n (%) | 2442 | 257 (13.2) | 13 (2.6) | <.001 |
ACO: asthma-COPD overlap; BMI: body mass index; BODE: body mass index, airflow obstruction, dyspnea, and exercise capacity; BODEx: body mass index, airflow obstruction, dyspnea and severe exercises; FEV1 post-bronchodilator %: postbronchodilator FEV1 percent predicted; HMV: home mechanical ventilation; LABA/ICS: long-acting beta-2 adrenergic agonist/inhaled corticosteroid; LABA/LAMA: long-acting beta-2 adrenergic agonist/long-acting muscarinic antagonist; LABA: long-acting beta-2 adrenergic agonist; LAMA/LABA/ICS: long-acting muscarinic antagonist/long-acting beta-2 adrenergic agonist/inhaled corticosteroid; LAMA: long-acting muscarinic antagonist; PYI: pack-year index; Quadruple: long-acting muscarinic antagonist/long-acting β-2 adrenergic agonist/inhaled corticosteroid/other drug (roflumilast or theophylline or long-term antibiotic).
Factors Associated With High-risk Level. Multivariate Analysis.
| Clinical and Epidemiological Factors | OR (95% CI) | P |
|---|---|---|
| Age (years) | ||
| ≤55 years | 1 | |
| >55 years | 1.63 (1.16–2.27) | .004 |
| BMI (kg/m2) | 0.96 (0.94–0.98) | <.001 |
| Active smoking | ||
| Yes | 0.60 (0.47–0.75) | <.001 |
| No | 1 | |
| Charlson≥3 | 1.33 (1.08–1.65) | .008 |
| Chronic cough | ||
| Yes | 2.24 (1.80–2.79) | <.001 |
| No | 1 | |
| Colonization | ||
| Yes | 3.17 (1.59–6.33) | .001 |
| No | 1 | |
Fig. 5 shows the distribution of patients by risk level and GesEPOC clinical phenotype. The most common phenotype in the high-risk group was non-exacerbator (46%). ACO was the least common phenotype (10.5% in the low-risk level, and 8.9% in the high-risk level).
Distribution of patients by risk level and GesEPOC clinical phenotype. The ACO phenotype was defined as having a diagnosis of bronchial asthma or clinical symptoms consistent with asthma, in addition to a positive bronchodilator test greater than or equal to 15%. ACO: asthma-COPD overlap phenotype; CB: chronic bronchitis.
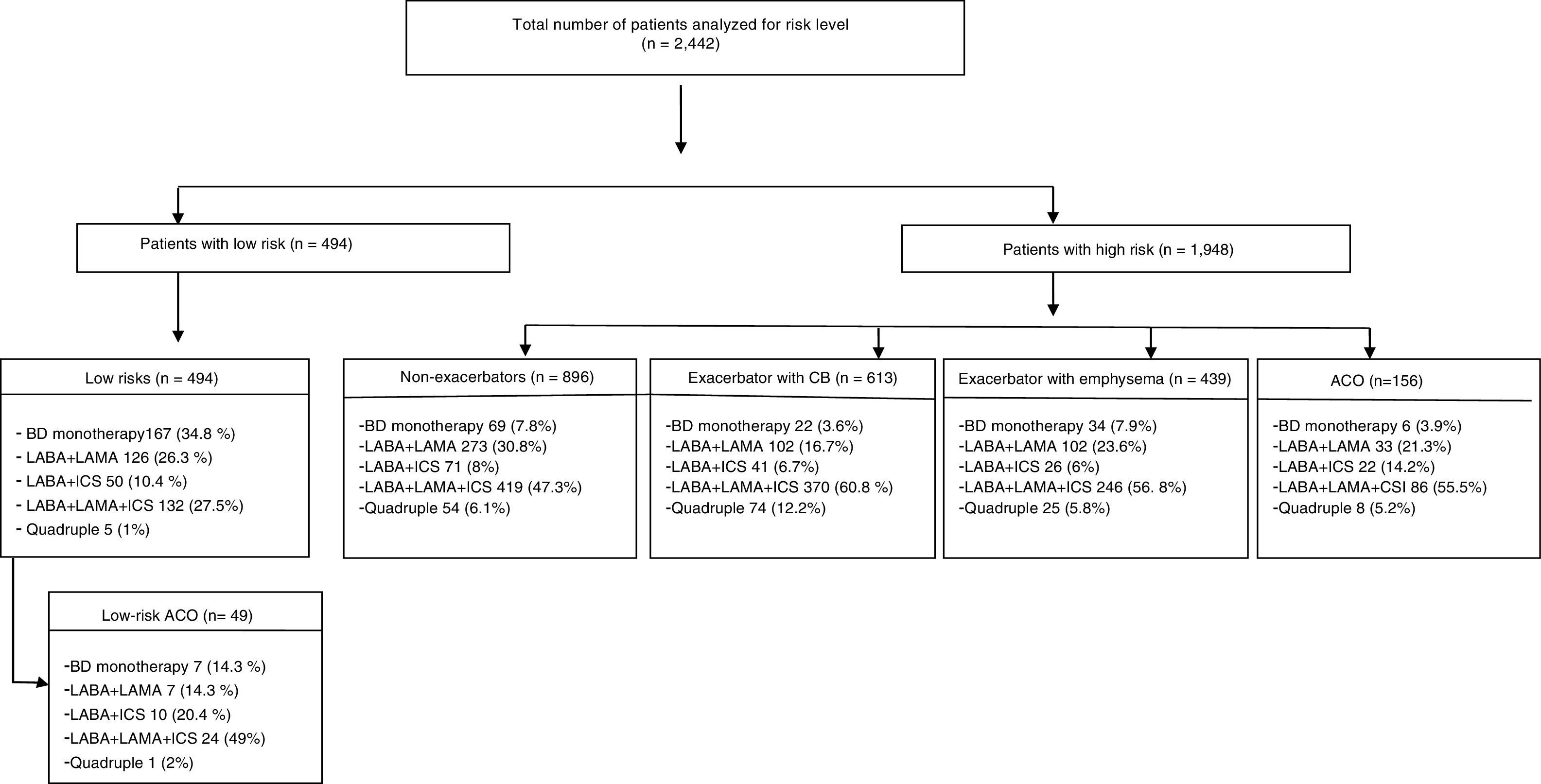
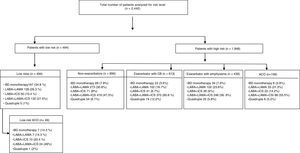
Fig. 6 shows the distribution of drug treatments for COPD by risk level and clinical phenotype. The most commonly used options were single-agent bronchodilators in the low-risk group (34.8%) and triple therapy (long-acting muscarinic antagonists/long-acting β-2 agonists/inhaled corticosteroids [LAMA/LABA/ICS]) in the high-risk group (53.7%).
Pharmacological treatment by risk level and GesEPOC clinical phenotype. ACO: asthma-COPD overlap; BD: bronchodilator; CB: chronic bronchitis; LABA/ICS: long-acting beta-2 adrenergic agonist/inhaled corticosteroid; LABA/LAMA: long-acting beta-2 adrenergic agonist/long-acting muscarinic antagonist; LABA: long-acting beta-2 adrenergic agonist; LAMA/LABA/ICS: long-acting muscarinic antagonist/long-acting beta-2 adrenergic agonist/inhaled corticosteroid; LAMA: long-acting muscarinic antagonist; Quadruple: long-acting muscarinic antagonist/long-acting β-2 adrenergic agonist/inhaled corticosteroid/other drug (roflumilast or theophylline or long-term antibiotic).
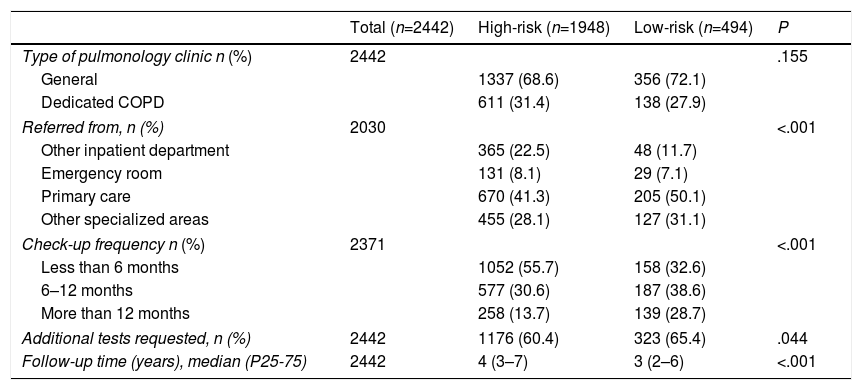
Care resources offered by risk level are described in Table 4. No differences were found in the type of clinic (general or COPD specialist) in which the patients were seen, according to the risk levels encountered. Low-risk patients were mainly referred from primary care centers (50.1%), while 20.4% of the high-risk patients were referred from other inpatient departments. High-risk patients attended visits more frequently, at intervals of less than 6 months in 55.7%, and their period of follow-up was longer.
Medical Care by Risk Level.
| Total (n=2442) | High-risk (n=1948) | Low-risk (n=494) | P | |
|---|---|---|---|---|
| Type of pulmonology clinic n (%) | 2442 | .155 | ||
| General | 1337 (68.6) | 356 (72.1) | ||
| Dedicated COPD | 611 (31.4) | 138 (27.9) | ||
| Referred from, n (%) | 2030 | <.001 | ||
| Other inpatient department | 365 (22.5) | 48 (11.7) | ||
| Emergency room | 131 (8.1) | 29 (7.1) | ||
| Primary care | 670 (41.3) | 205 (50.1) | ||
| Other specialized areas | 455 (28.1) | 127 (31.1) | ||
| Check-up frequency n (%) | 2371 | <.001 | ||
| Less than 6 months | 1052 (55.7) | 158 (32.6) | ||
| 6–12 months | 577 (30.6) | 187 (38.6) | ||
| More than 12 months | 258 (13.7) | 139 (28.7) | ||
| Additional tests requested, n (%) | 2442 | 1176 (60.4) | 323 (65.4) | .044 |
| Follow-up time (years), median (P25-75) | 2442 | 4 (3–7) | 3 (2–6) | <.001 |
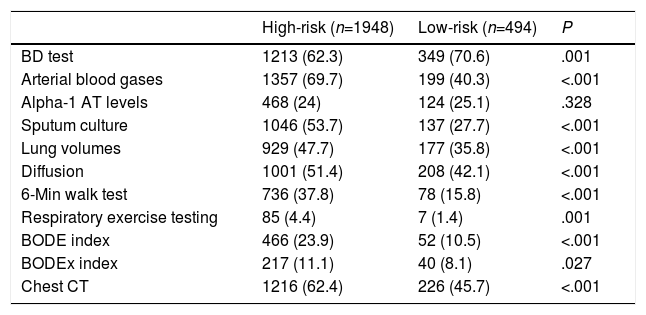
The main diagnostic procedures performed during follow-up are described in Table 5. The functional assessment tests most frequently performed in the high-risk level were lung volume assessment (47.7% versus 35.8%; P<.001), diffusion test (51.4% versus 42.1%; P<.001), and the walk test (37.8% versus 15.8%; P<.001). In contrast, the bronchodilator test was performed more frequently in low-risk patients (70.6% versus 62.3%; P=.001). Chest computed axial tomography (CT), sputum analysis, and the estimation of severity using BODE and BODEx were more frequent in the high-risk level.
Diagnostic Procedures by Risk Level.
| High-risk (n=1948) | Low-risk (n=494) | P | |
|---|---|---|---|
| BD test | 1213 (62.3) | 349 (70.6) | .001 |
| Arterial blood gases | 1357 (69.7) | 199 (40.3) | <.001 |
| Alpha-1 AT levels | 468 (24) | 124 (25.1) | .328 |
| Sputum culture | 1046 (53.7) | 137 (27.7) | <.001 |
| Lung volumes | 929 (47.7) | 177 (35.8) | <.001 |
| Diffusion | 1001 (51.4) | 208 (42.1) | <.001 |
| 6-Min walk test | 736 (37.8) | 78 (15.8) | <.001 |
| Respiratory exercise testing | 85 (4.4) | 7 (1.4) | .001 |
| BODE index | 466 (23.9) | 52 (10.5) | <.001 |
| BODEx index | 217 (11.1) | 40 (8.1) | .027 |
| Chest CT | 1216 (62.4) | 226 (45.7) | <.001 |
Alpha-1 AT: alpha-1 antitrypsin; BODE: body mass index, airflow obstruction, dyspnea and exercise capacity; BODEx: body mass index, airflow obstruction, dyspnea and severe exacerbations; BD test: bronchodilator test; CT: computed tomography.
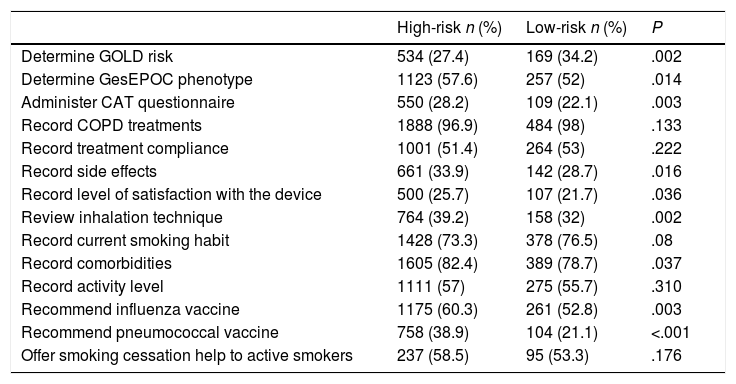
Table 6 lists the main clinical actions taken during the last audited visit of each patient. The most frequent action in the high-risk group was determination of GesEPOC phenotype (57.6% versus 52%; P=.014). Other more frequent actions in this group were recording of comorbidities (82.4% versus 78.7%; P=.037), review of inhalation technique (39.2% versus 32%; P=.002), administration of the CAT questionnaire (28.2% versus 22.1%; P=.003), and recommendation of influenza and pneumococcal vaccines.
Actions Taken by Risk Level.
| High-risk n (%) | Low-risk n (%) | P | |
|---|---|---|---|
| Determine GOLD risk | 534 (27.4) | 169 (34.2) | .002 |
| Determine GesEPOC phenotype | 1123 (57.6) | 257 (52) | .014 |
| Administer CAT questionnaire | 550 (28.2) | 109 (22.1) | .003 |
| Record COPD treatments | 1888 (96.9) | 484 (98) | .133 |
| Record treatment compliance | 1001 (51.4) | 264 (53) | .222 |
| Record side effects | 661 (33.9) | 142 (28.7) | .016 |
| Record level of satisfaction with the device | 500 (25.7) | 107 (21.7) | .036 |
| Review inhalation technique | 764 (39.2) | 158 (32) | .002 |
| Record current smoking habit | 1428 (73.3) | 378 (76.5) | .08 |
| Record comorbidities | 1605 (82.4) | 389 (78.7) | .037 |
| Record activity level | 1111 (57) | 275 (55.7) | .310 |
| Recommend influenza vaccine | 1175 (60.3) | 261 (52.8) | .003 |
| Recommend pneumococcal vaccine | 758 (38.9) | 104 (21.1) | <.001 |
| Offer smoking cessation help to active smokers | 237 (58.5) | 95 (53.3) | .176 |
CAT: COPD assessment test; CRQ: global initiative for chronic obstructive lung disease.
This is the first study to contribute data on the distribution and clinical characteristics of patients seen in pulmonology clinics in Spain, classified according to their COPD risk levels using the current GesEPOC guidelines.8
One of the most important factors that should be included in the evaluation of COPD patients is risk assessment, understood as the likelihood of the patient experiencing exacerbations (with or without hospitalization), disease progression, future complications, or greater use of health care resources. Numerous studies have shown that FEV1 is a good predictor of mortality and morbidity.11,12 However, it should be remembered that other parameters predict mortality independently of function, for example, dyspnea13 and exacerbations.5,14 These 3 parameters are used in the GesEPOC guidelines for stratifying COPD risk, taking into account the need for applying appropriate levels of diagnostic and therapeutic intervention.
The results of our study show that most COPD patients seen in pulmonology clinics in Spain are classified as high-risk. In total, 37.6% of patients were defined as high-risk because they met 2 criteria, and 27.4% because they met 3 criteria (dyspnea grade, airflow obstruction, and history of exacerbations). It is worth noting that most of the high-risk patients met the criteria of mMRC dyspnea grade≥2 (74.7%) and FEV1<50% (63.6%). However, only 35.9% had been hospitalized at least once, and only 39.7% had had more than 1 moderate exacerbation in the previous year. Recent studies in pulmonology clinics in Spain confirm that less than one third of COPD patients have a history of ≥2 exacerbations, while mMRC dyspnea grade≥2 or FEV1<50% is seen in more than 2 thirds of patients.15–17
It should also be mentioned that in our study, only 34 patients (1.75% of the high-risk group) were classified as high-risk on the basis of a single criterion of dyspnea grade 2 and receiving bronchodilator therapy as maintenance treatment, for which reason they may be considered to be undertreated. However, future studies may contribute more information for weighting the variables that define the level of risk.
In our study, patients with a high risk level were older and presented more comorbidities, along with chronic expectoration and more frequent colonization, factors independently associated with a high risk. These findings are in line with numerous studies that have shown that the presence of comorbidities, cough with chronic expectoration, and bacterial load in the airway are associated with an increased risk of exacerbations, worse prognosis and increased mortality.18–21 Several studies have found that age is inevitably associated with an increase in mortality, although this could be explained in part by the presence of related factors such as social support, physical disability, depression, and quality of life,22 factors that would define a subgroup of highly complex or “fragile” patients who, in addition to their high risk of complications, will require a more individualized approach.23 Active smoking was less common among patients in the high-risk group, probably as a consequence of their level of severity.
In our study, patients with a high risk level showed greater severity measured on the BODE/BODEx indices, with significant differences with respect to the low-risk group. All patients with a low risk level were in quartile 1 of the BODEx scores. These results support the usefulness of GesEPOC risk stratification as a tool for assessing patients and for adapting the level of intervention.
The distribution of clinical phenotypes was similar to that obtained in other national and international studies, the non-exacerbator phenotype being the most common among patients seen in our pulmonology clinics.15,16,24 This is interesting considering that most patients had severe obstruction, but could be explained to a certain extent by the more intense treatment and follow-up received by these patients. The ACO phenotype, defined by the criteria discussed above, was uncommon (10.5% in the low-risk and 8.9% in the high-risk levels), in line with previous studies and with minimal differences according to the criteria used.16,24–27 However, in our study we did not include peripheral eosinophilia as a diagnostic criterion for ACO, and this may have led to an underestimation of prevalence.
With regard to treatment by risk level and clinical phenotype, a high percentage of patients in both risk levels received ICS. In the high-risk level, triple therapy was the most widely used combination, prescribed in 47.4% of non-exacerbators and up to 60.8% of exacerbators with chronic bronchitis. Triple therapy was also administered to low-risk patients, although the most common option was monotherapy with a long-acting bronchodilator. However, 10.4% of low-risk patients were receiving LABA+ICS and 27.4% were receiving LABA+LAMA+ICS. This overuse of ICS in low-risk patients cannot be explained by the frequency of the ACO phenotype, as only 10.5% of patients met these criteria. It will be of interest in the future to analyze the number of low-risk patients who fulfill the GesEPOC criteria for ACO28 and how they are treated, since GesEPOC recommends that only bronchodilators should be used in this risk group. It should also be mentioned that only 34 patients (1.75% of the high-risk group) were classified as high-risk by meeting a single criterion of dyspnea grade 2 and receiving bronchodilator therapy as maintenance treatment, for which reason they may be considered to be undertreated.
Numerous national and international studies in different levels of care have shown intensive ICS use in COPD patients.29,30 In Spain, several studies30,31 have shown that more than 60% of COPD patients receive treatment with ICS alone or in combination with a long-acting bronchodilator, often at high doses. Moreover, ICS are often prescribed in combination with bronchodilators as first-line therapy after diagnosis,32 thus deviating from good clinical practice guidelines.33 However, in recent years, studies in Spain evaluating treatment according to clinical phenotypes have shown that the use of ICS in non-exacerbators has fallen.34 Indeed, the FENEPOC study, conducted in 2013 in both healthcare settings in Spain, showed that triple therapy was given as maintenance treatment to 28.7% of non-exacerbators, 58% of exacerbators, and 59.5% of ACO patients.15
With regard to the medical care and actions taken according to the level of risk, it should be noted that although high-risk patients were seen more frequently and received longer follow-up, we found no differences in the type of clinic where the patients were seen (general or dedicated COPD clinic). In contrast, differences between the two risk levels were detected in diagnostic and therapeutic interventions: certain tests, such as the measurement of lung volumes, computed tomography, the walk test, phenotyping and administration of the CAT questionnaire were more frequent in the high-risk group. These data are in line with the GesEPOC recommendations, which establish a greater need for diagnostic or therapeutic interventions in patients with a high level of risk. However, while these results demonstrate that COPD patients are treated differently in the pulmonology clinic depending on their level of risk, much can be done to improve adherence to good clinical practice recommendations in both risk levels, and these variations in adherence can be explained by patient variables in only a small proportion of cases. Screening for alpha-1 antitrypsin deficiency was very low in both risk levels.
Finally, some methodological limitations must be pointed out. For example, the selection of hospitals for participation in this study was not random, as it was based on previous participation in COPD clinical audits and the willingness of the sites to participate. We must also remember that this was a cross-sectional study, so differences in risk of exacerbations, complications and mortality between risk levels cannot be evaluated. Another limitation, intrinsic to all clinical audits, is that despite the use of specific inclusion criteria and regular supervision of data entry, some values were missing from the records consulted and therefore could not be included in the database. Nevertheless, despite these limitations, we believe that the study sample, which includes a population from 16 autonomous communities, is representative of the medical care delivered to COPD patients in pulmonology clinics in Spain.
ConclusionStratification of COPD patients into risk levels must be considered a key step in the evaluation and treatment of these individuals. Variables that determine the level of risk have the virtue of being potentially modifiable. This attribute reinforces the importance of planning therapeutic interventions according to risk level and implementing strategies aimed at reversing the effects of such variables, thereby improving the survival of patients with COPD.
The results of this study contribute to the understanding of the strengths and weaknesses of the care we offer in terms of the risk level defined in GesEPOC 2017, although we must take into account the limitations intrinsic to any study based on a clinical audit in selected centers.
Further studies, then, are needed to determine whether the risk level has an impact on clinically relevant outcomes, such as the risk of exacerbations and survival, which would support future changes in the diagnostic and therapeutic strategy in COPD.
FundingThe Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) promoted and sponsored this study, with financial support from Boehringer Ingelheim. The funding body did not participate in the study design, data collection, analysis, publication, or preparation of this manuscript.
Conflict of InterestsThe authors state that they have no conflict of interests.
The authors thank the investigators and the hospitals that participated in the EPOCONSUL study (Annex 1), and Boehringer Ingelheim for their collaboration in this project.
Participating hospitals and investigators (EPOCONSUL Group):
Andalusia: José Luis Rojas Box, H. de Alta Resolución de Écija, Seville. José Domingo García Jiménez, H. de Alta Resolución de Utrera, Seville. Adolfo Domenech del Río, Ana Muñoz, H. Carlos Hayas, Malaga. Antonia Soto Venegas, H. San Juan de la Cruz, Úbeda, Jaén. Aurelio Arnedillo Muñoz, H. U. Puerta del Mar, Cádiz. Agustín Valido Morales, H. Virgen de Macarena. Seville. José Velasco Garrido, Carlos Rueda Ríos, Macarena Arroyo Varela, H. Virgen de la Victoria. Málaga. Francisco Ortega Ruiz, Eduardo Márquez Martin, Carmen Calero Acuña, H. Virgen del Rocío, Seville. Francisco Luis García Gil, H. U. Reina Sofía, Córdoba.
Aragón: Joaquín Carlos Costan Galicia, H. Clínico U. Lozano Blesa, Zaragoza. Ana Boldova Loscertales, H. Royo Villanova, Zaragoza.
Asturias: Cristina Martínez González, Rosirys Guzmán Taveras, H. U. Central de Asturias, Oviedo.
Murcia: Juan Luis de la Torre Álvaro, H. U. Santa Lucía, Cartagena. M. Jesús Avilés Ingles, H. General U. Reina Sofía, Murcia. Rubén Andújar Espinosa, H. U. Virgen de la Arrixaca, Murcia.
Canary Islands: Juan Manuel Palmero Tejera, Juan Marco Figueira Conçalves, H. U. Nuestra Señora de la Candelaria, Santa Cruz de Tenerife.
Cantabria: Ramón Agüero Balbín, Carlos Amado Diago, Beatriz Abascal Bolado, H. Marqués de Valdecilla, Santander. Juan Luis García Rivero, Marcelle Cohen Escovar, H. de Laredo, Santander.
Castile La Mancha: Francisco Javier Callejas González, Complejo Hospitalario Universitario de Albacete, Albacete. Ángel Ortega González, H. Nuestra Señora del Prado, Talavera de la Reina, Toledo. Rosario Vargas González, H. Virgen de la Luz, Cuenca. Encarnación López Gabaldón, Raúl Hidalgo Carvajal, H. Virgen de la Salud, Toledo.
Castile and Leon: Elena Bollo de Miguel, Silvia Fernández Huerga, Complejo Hospitalario Universitario de León, León. Ana Pueyo Bastida, Complejo Asistencial de Burgos, Burgos. Jesús R. Hernández Hernández, Ruth García García, H. Nuestra Señora de Sonsoles, Ávila. Miguel Barrueco Ferrero, Marco López Zuibizarreta, E. Consuelo Fernández, H. Universitario de Salamanca, Salamanca.
Catalonia: David de la Rosa Carrillo, H. Plató, Barcelona. Jordi Esplugas Abós, Noelia Pablos Mateos, H. Sant Joan de Déu, Martorell. Elena de Miguel Campos, H. Sant Joan de Despí, Barcelona. Pablo Rubinstein, Hospital General de Cataluña, Barcelona. Hernán Abraham Manrique Chávez, H. Sagrat Cor, Barcelona. Miriam Barrecheguren, H. U. Vall d’Hebrón, Barcelona.
Valencia: Carmen Aguar Benito, H. de Arnau de Villanova, Valencia. Pablo Catalán Serra, H. de Requena, Requena. Eusebi Chiner Vives. H. U. de San Juan, Alicante. Juan Antonio Royo Prats. H. General de Castellón, Castellón de la Plana. Cristina Sabater Abad, Esther Verdejo Mengual, H. General Universitario de Valencia, Valencia. Eva Martínez-Moragón, H. Universitario Dr. Peset, Valencia.
Extremadura: Francisca Lourdes Márquez Pérez, H. U. Santa Cristina, Badajoz.
Galicia: Alberto Fernández Villar, Cristina Represas Represas, Ana Priegue Carrera, Complejo Hospitalario de Vigo, Vigo. Marina Blanco Aparicio, Pedro Jorge Marcos Rodríguez, H. U. Juan Canalejo, Corunna.
Balearic Islands: Federico Gonzalo Fiorentino, M. Magdalena Pan Naranjo, H. Son Espases, Palma de Mallorca. Antonia Fuster Gomila, H. Sant Llatzer, Palma de Mallorca.
Madrid: Germán Peces Barba, Felipe Villar Álvarez, Fundación Jiménez Díaz, Madrid. Carlos José Álvarez Martínez, H. 12 de Octubre, Madrid. Juan Luis Rodríguez Hermosa, J. L. Álvarez Sala-Walther, H. Clínico San Carlos, Madrid. José Andrés García Romero de Tejada, H. U. Infanta Sofía, San Sebastián de los Reyes, Madrid. Javier Jareño, Sergio Campos Téllez, H. Central de la Defensa, Madrid. Raúl Galera Martínez, H. La Paz. Rosa Mar Gómez Punter, Emma Vázquez Espinosa, H. La Princesa, Madrid. Esther Alonso Peces, H. Príncipe de Asturias, Alcalá de Henares, Madrid. Juan Manuel Diez Piña, Raquel Pérez Rojo, H. U. de Móstoles, Madrid. Luis Puente Maestu, Julia García de Pedro, H. U. Gregorio Marañón, Madrid. Soledad Alonso Viteri, H. U. de Torrejón, Torrejón de Ardoz, Madrid.
Navarre: María Hernández Bonaga, Complejo Hospitalario de Navarra, Pamplona.
Basque Country: María Milagros Iriberri Pascual, H. de Cruces, Baracaldo. Myriam Aburto Barrenechea, H. de Galdakano. Sophe García Fuika, Hospital Santiago Apostol, Vitoria. Patricia Sobradillo Ecenarro, Hospital Txagorritx, Basurto.
Please cite this article as: Rubio MC, Hermosa JL, Soler-Cataluña JJ, López-Campos JL, Navarrete BA, Soriano JB, et al. Atención médica según el nivel de riesgo y su adecuación a las recomendaciones de la guía española de la enfermedad pulmonar obstructiva crónica (EPOC) (GesEPOC): Estudio EPOCONSUL. Arch Bronconeumol. 2018;54:270–279.