To the editor:
Analysis of the mediastinal lymph nodes is a determining factor for lung cancer staging and, until recently, cervical mediastinoscopy was considered the gold standard for mediastinal staging. However, with the advent of endobronchial ultrasound guided transbronchial needle aspiration (EBUS-TBNA), sensitivity of diagnosing mediastinal ganglia using less invasive techniques seems to have increased. We report the case of a 53-year-old woman diagnosed with a carcinoid tumour in the lower left lobe, in which positron emission tomography showed a maximum standardised uptake value (PET SUVmax) of 4 in a high left paratracheal adenopathy (space 2L). Using real-time EBUS (BF-UC180F with Aloka ProSound alpha 5) a swollen lymph node was found in the 2L space and the aspiration needle inserted 3 times. The patient tolerated the procedure well and was discharged the same day. After 48 h, she reported to the general hospital emergency department with erythema over the sternal notch, neck pain and fever. Laboratory tests showed high blood inflammatory markers: C-reactive protein (CRP) 219.2 and a white blood count (WBC) of 12,280/mm3. The chest radiograph showed no alterations, but a CT scan showed acute mediastinitis in the left superior mediastinum, with prevascular fatty infiltration and left pretracheal affection (Figs. 1a and b). Empirical treatment was initiated with piperacillintazobactam, 4/0.5g iv every 8 hours, and clinical improvement was seen after 5 days, with less erythema and pain. The inflammatory parameters also normalised a week after starting the treatment (PCR 67.7 and leukocyte count 7960).
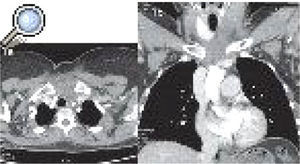
Thoracic CT mediastinal window. a) Axial section in superior mediastinum with thickening of the skin and subcutaneous tissue at the cervical midline. b) Coronal section with cloudiness to the left paratracheal fatty tissue extending to the retrosternal and prevascular fatty tissue in superior mediastinum.
In 2009, Varela Lema et al. published a systematic review examining the efficacy and safety of EBUS-TBNA,1 with more than 1627 patients in 20 series where no serious complications were found. More recently, 4 cases of infectious complications after EBUSTBNA were published: pericarditis after a the subcarinal adenopathy had been punctured,2 tumour bed contamination after pulmonary squamous tumour had been punctured,3 infection after biopsy of a thyroid cystic lesion,3 and, more recently, mediastinitis produced by biopsy of an adenopathy.4 This is the first time that an acute mediastinitis after EBUS-TBNA has been reported in Spain. There is also another case of mediastinitis after puncturing an adenopathy following endoscopic aspiration (EUS-FNA).5 The hypothesis for the relationship between bronchoscopy and mediastinitis is that, when the bronchoscope goes through the nasopharyngeal region, the working channel is contaminated. As a result, when the transbronchial needle passes through the working channel, it gets contaminated and can infect the tissue sample. The American Society for Brochology published a bronchoscope handling guide6 which concluded that it was not necessary to use prophylactic antibiotics when puncturing the mediastinal lymph nodes due to the low rate of complications.
We agree with this, but we believe that the appearance and size of lymph nodes are variables to keep in mind when performing the puncture, as larger lesions or those with a necrotic appearance could have compromised blood flow, and therefore may reduce the capacity to clear the bacterial inoculation. We conclude that EBUS-TBNA is a safe procedure. This was our first complication after performing more than 750 EBUS-TBNA operations, however, we must be alert in order to detect and report any complications in this new technique, as these infectious complications require early diagnosis and treatment.