In March 2010, a 60-year-old male non-smoker was referred to our Thoracic Surgery Unit with a history of dyspepsia during the previous three months and two episodes of syncope.
Past medical history included left hemicolectomy resection for pT1pN0 adenocarcinoma of the sigma more than 10 years previously. Colonoscopy was performed 6 months before our observation during a routine follow-up appointment and proved negative. Electrocardiogram (EKG) revealed sinus bradycardia; transthoracic echocardiography (TTE) showed normal left ventricular function with no segmental kinetic changes, no valvular stenosis or insufficiency and normal ejection fraction. Tilt test was negative. Neurologic examination and computed tomography (CT) scan of the head were also negative for expansive or ischemic/hemorrhagic lesions.
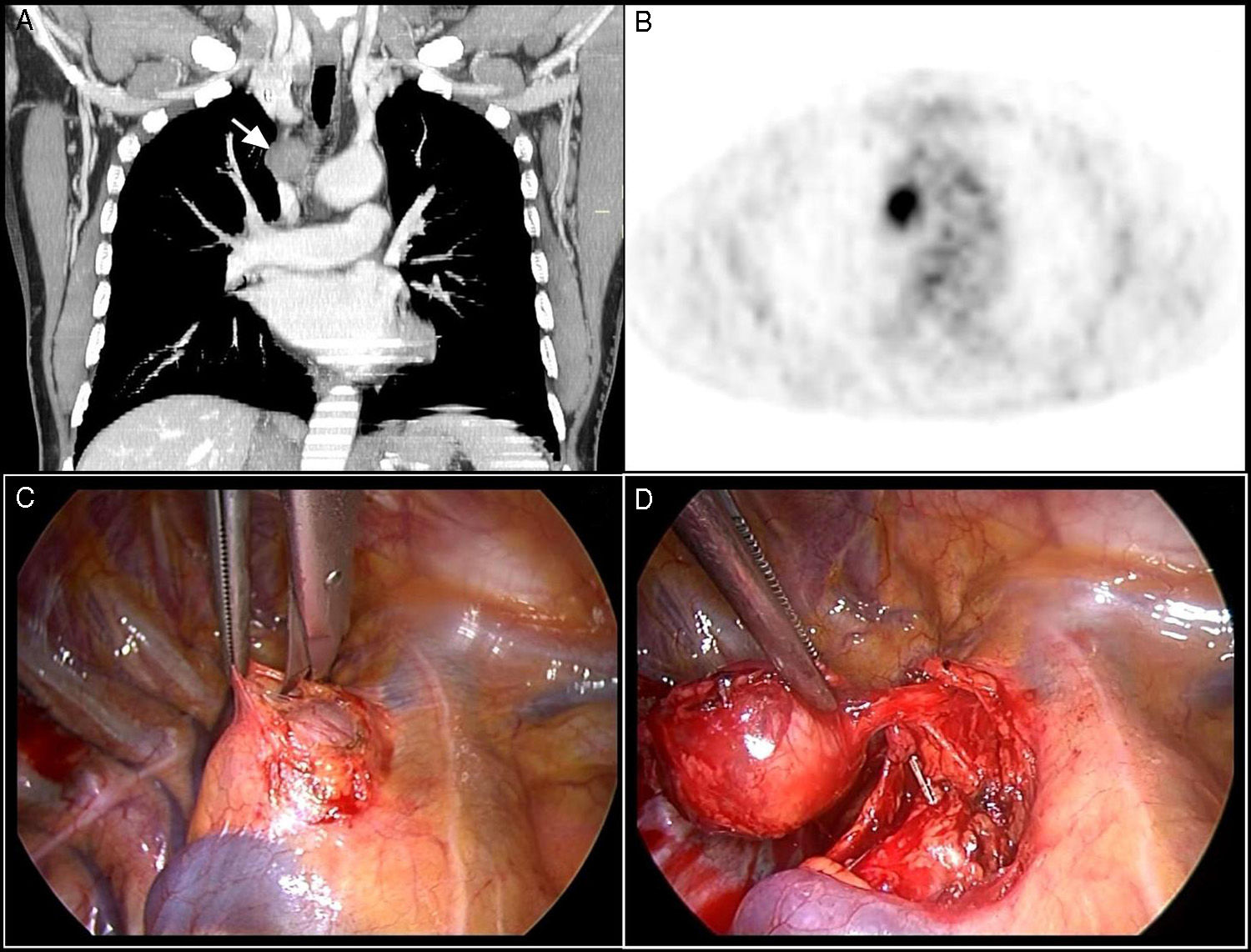
Chest X-ray revealed mild prominence of the right heart border. Subsequent chest CT scan with iodine contrast medium showed a soft, well-defined, encapsulated paratracheal and retrocaval lesion measuring 24mm×26mm (Fig. 1A), located in the proximity of the azygos vein arch. An 18F-FDG PET scan (Fig. 1B) revealed an increased uptake value corresponding with the lesion [standard uptake value (SUV)=5.91]. After the weekly discussion meeting, we decided to perform transbronchial needle aspiration (TBNA); biopsy revealed nerve cells, compatible with low-grade nerve tissue tumor.
(A) Chest CT-Scan showing a well-defined paratracheal and retrocaval soft lesion, 24mm×26mm, located in the proximity of the azygos vein arch, characterized by medium contrast uptake. (B) 18F FDG-PET scan showing increased spot uptake located in correspondence of the lesion (SUV=5.91). (C) Intraoperative thoracoscopic view; (D) intracapsular enucleation of the lesion after opening the mediastinal pleura.
The patient was scheduled for surgery and underwent successful enucleation of the mediastinal lesion using a biportal thoracoscopic approach. The patient was placed in left lateral decubitus. Single lung ventilation was achieved using a double-lumen endobronchial tube positioned under fiberoptic guidance. A 4-centimeter surgical access was made in the 4th intercostal space and a second thoracotomy for the camera was made under direct vision in the 8th intercostal space on the mid-axillary line.
The nodule was identified on the right vagus nerve just above the azygos vein arch and excised by intracapsular enucleation (Figs. 1C and D); the anatomical integrity of the right vagus nerve could not be preserved and it was sacrificed. Continuous EKG monitoring was performed during the post-operative period to monitor for bradycardia due to vagus nerve injury. No atropine administration was required.
At the end of the surgical procedures, a 24Ch chest tube was placed to guarantee lung re-expansion through the lower thoracotomy.
The post-operative period was uneventful and the patient was discharged after four days. Visual analog scale (VAS) for pain on day 1 post-surgery was 1 (range 0–10).
Histopathology of the specimen showed fascicles of spindle cells in a loose stroma. Strong positivity of the tumor cells for S-100 protein confirmed the diagnosis of schwannoma Antoni type A.1
The patient reported resolution of symptoms and EKG revealed sinus rhythm at 78bpm, probably linked to reduction of the parasympathetic effect on the heart rhythm caused by vagus nerve stimulation due to the mass. No recurrence was observed after a 4-year follow-up.
Schwannomas are uncommon, mainly benign, tumors that can arise from all myelinic nerve fibers. Vagus nerve schwannomas are rare mediastinal masses, accounting for 2% of all mediastinal neurological tumors, arising typically from the nerve sheath and extrinsically compressing the nerve fibers.2
Biportal VATS is a safe approach for excision of this kind of lesion and produces less post-operative pain and a shorter hospital stay.3
To conclude, this was a rare symptomatic mediastinal lesion, successfully treated by a minimally invasive surgical approach.
Please cite this article as: Roncon A, Davoli F, Casadio C, Baietto G, Rena O, Turello D. Schwannoma del nervio vago mediastínico tratado exitosamente con toracoscopia biportal videoasistida. Arch Bronconeumol. 2015;51:102–103.