Plastic bronchitis (PB) is a rare disease characterized by the formation of bronchial casts that partially or fully block the bronchial lumen.1,2 It occurs as a complication of respiratory diseases, lymphatic abnormalities, infections, and particularly after surgery for congenital heart diseases, especially the Fontan procedure,1,2 and is often confused with bronchoaspiration.2 We report a case series of patients with a diagnosis of plastic bronchitis.
Between 2001 and 2016, 13 patients were diagnosed with plastic bronchitis, and a total of 18 bronchoscopies were performed. All patients were diagnosed using flexible bronchoscopy (FB).
Mean patient age was 31 months (range: 1 month to 8 years); 7 boys and 6 girls. The most common underlying processes were recurrent wheezing and asthma, reported in 10 patients. The other 3 patients presented malignant pertussis (1), lymphocytic leukemia (1), and complex congenital heart disease with double outlet right ventricle for which the patient had undergone multiple surgical interventions, including the Fontan procedure (1).
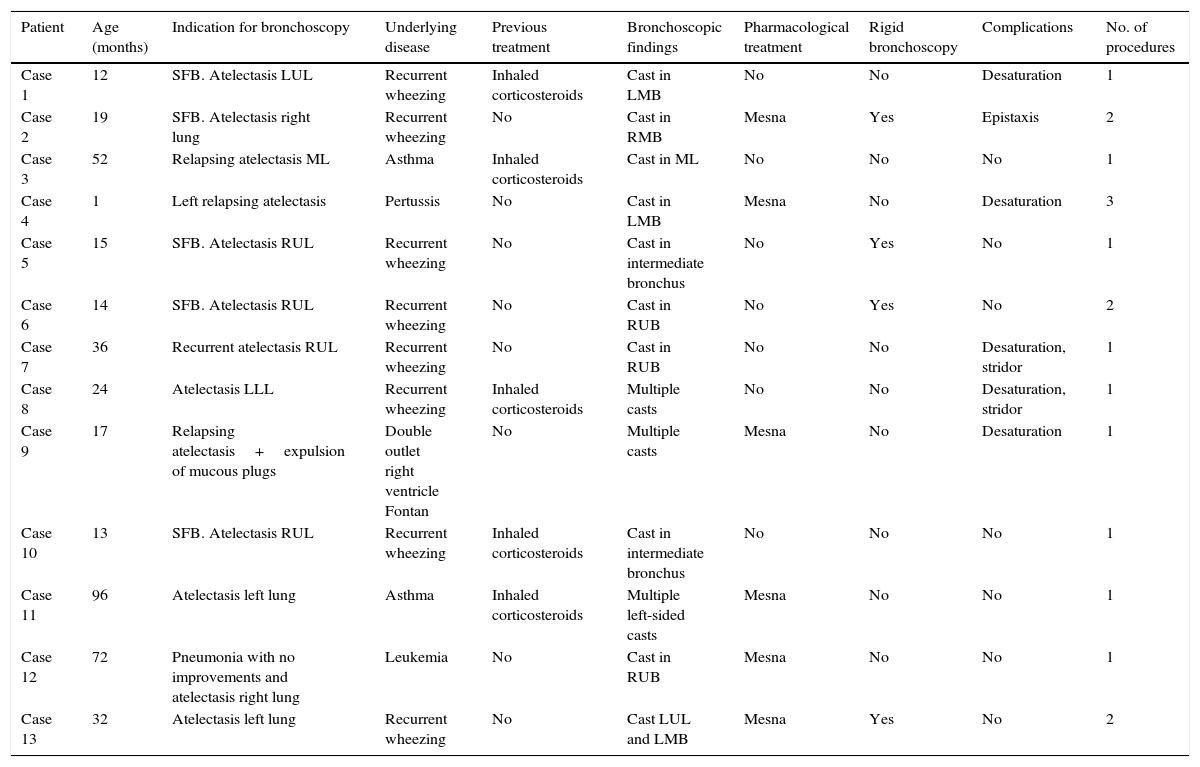
Symptoms on presentation included fever, breathing difficulties, and bronchorrhea. FB findings are shown in Table 1.
Clinical and Bronchoscopic Characteristics of Patients.
| Patient | Age (months) | Indication for bronchoscopy | Underlying disease | Previous treatment | Bronchoscopic findings | Pharmacological treatment | Rigid bronchoscopy | Complications | No. of procedures |
|---|---|---|---|---|---|---|---|---|---|
| Case 1 | 12 | SFB. Atelectasis LUL | Recurrent wheezing | Inhaled corticosteroids | Cast in LMB | No | No | Desaturation | 1 |
| Case 2 | 19 | SFB. Atelectasis right lung | Recurrent wheezing | No | Cast in RMB | Mesna | Yes | Epistaxis | 2 |
| Case 3 | 52 | Relapsing atelectasis ML | Asthma | Inhaled corticosteroids | Cast in ML | No | No | No | 1 |
| Case 4 | 1 | Left relapsing atelectasis | Pertussis | No | Cast in LMB | Mesna | No | Desaturation | 3 |
| Case 5 | 15 | SFB. Atelectasis RUL | Recurrent wheezing | No | Cast in intermediate bronchus | No | Yes | No | 1 |
| Case 6 | 14 | SFB. Atelectasis RUL | Recurrent wheezing | No | Cast in RUB | No | Yes | No | 2 |
| Case 7 | 36 | Recurrent atelectasis RUL | Recurrent wheezing | No | Cast in RUB | No | No | Desaturation, stridor | 1 |
| Case 8 | 24 | Atelectasis LLL | Recurrent wheezing | Inhaled corticosteroids | Multiple casts | No | No | Desaturation, stridor | 1 |
| Case 9 | 17 | Relapsing atelectasis+expulsion of mucous plugs | Double outlet right ventricle Fontan | No | Multiple casts | Mesna | No | Desaturation | 1 |
| Case 10 | 13 | SFB. Atelectasis RUL | Recurrent wheezing | Inhaled corticosteroids | Cast in intermediate bronchus | No | No | No | 1 |
| Case 11 | 96 | Atelectasis left lung | Asthma | Inhaled corticosteroids | Multiple left-sided casts | Mesna | No | No | 1 |
| Case 12 | 72 | Pneumonia with no improvements and atelectasis right lung | Leukemia | No | Cast in RUB | Mesna | No | No | 1 |
| Case 13 | 32 | Atelectasis left lung | Recurrent wheezing | No | Cast LUL and LMB | Mesna | Yes | No | 2 |
RMB: right main bronchus; LMB: left main bronchus; RUB: right upper bronchus; RLL: right lower lobe; LLL: left lower lobe; ML: middle lobe; RUL: right upper lobe; LUL: left upper lobe; Mesna: 2-mercaptoethane sulfonate; SFB: suspected foreign body.
With respect to treatment, bronchial casts were extracted from all patients. Four of the 13 patients required rigid bronchoscopy (RB) for complete removal of the cast. Four patients required repeated FBs due to persistent symptoms. No notable incidents occurred during the procedures, with the exception of self-limiting desaturations. A histological study of the material from the heart patient reported fibrinous material with scant cellularity.
Progress of 11 of the 13 patients was satisfactory with full recovery, while 2 patients died: the patient with congenital heart disease and the patient with leukemia. The congenital heart disease patient had a relapse of his PB one month later, and died due to this process in the referral hospital, while the leukemia patient died of her underlying disease.
PB is an uncommon disease,3 consisting of obstruction of the airway by casts. It is mainly associated with underlying congenital heart disease or lung diseases. Seear et al. categorized PB as type 1: casts made up of inflammatory cells, common in lung diseases; and type 2: hypocellular casts with mucin, common in heart disease.4 Although the etiology has not been fully clarified, the formation of the casts appears to be due to lymph fluid building up in the lung. Leakage of lymph fluid to the bronchial tree results in obstruction of the respiratory tract and loss of lymphatic cells and immunoglobulins, leading to increased susceptibility to infections.1,3 Madsen et al. propose a model in which the inflammatory processes activated in asthma would cause dysregulation of the formation of mucus that, together with reduced mucociliary clearance and infiltration of the airway by neutrophils and eosinophils, would explain the pathophysiology of PB.5 Atelectasis is commonly observed on imaging tests, providing a differential diagnosis with foreign-body bronchoaspiration.
Treatment consists of bronchoalveolar lavage and FB aspiration. In some cases RB is required for aspiration and extraction of the material with forceps.6
Other treatment options are available, such as the method recently described by Gibb et al., consisting of administration of a fibrinolytic agent (tissue-type plasminogen activator (t-PA))7 via FB, but we have no experience of this technique. Most studies, however, indicate inhaled t-PA for disrupting the bronchial cast.6,8 Other treatments include aerosolized fibrinolytics, such as urokinase, or inhaled mucolytics, such as acetylcysteine and dornase alfa.8–12 Mucolytics appear to be more useful in type 1 casts, which have a higher mucin content.4,11,12 In patients with congenital heart diseases, a good cardiac output must be achieved, while in those with lung diseases that involve bronchial hyperreactivity, treatment is based on the use of inhaled and systemic corticosteroids.12
Prognosis is generally good,1 except in cases associated with congenital heart diseases, in which mortality can be as high as 29%,13 and 41% of patients can present life-threatening events.13
In conclusion, while PB is an uncommon process, it must be taken into account in patients with recurrent atelectasis and in case of a suspected intrabronchial foreign body. Patients with underlying heart diseases are at greatest risk of death, while those with inflammatory processes present a less severe clinical picture.
We thank all the members of the Respiratory Medicine Section of the Hospital Materno-Infantil de Málaga.
Please cite this article as: Ruiz EP, Castillo MC, Aguilera PC, Frías JP. Bronquitis plástica en pediatría: manejo y tratamiento. Arch Bronconeumol. 2017;53:467–468.