The Covid-19 pandemic has created a situation that is unprecedented in the history of medicine. Health systems have already changed all over the world, and the effects of the situation will continue to influence how we will manage respiratory diseases and, more specifically, how we will monitor patients with these diseases.
SARS-CoV-2, the virus that causes Covid-19, has a special predilection for the respiratory epithelium, triggering episodes of pneumonia and severe acute respiratory failure and often requiring admission to hospital and intensive care units.1 The radiologic picture usually shows bilateral, more or less severe involvement, with the appearance of peripheral ground glass opacities and/or consolidations in the alveolar space,2 while cavitation, pleural effusion, and fibrosis are very rare. These lesions are also observed in patients seen in primary care centers who have not required hospital admission. Although few descriptions of lung tissue samples have been published, the available reports depict a histopathological picture of acute alveolar damage and fibromyxoid cell exudate, with pulmonary edema, desquamation of pneumocytes, and hyaline membrane formation.3
This clinical-radiological-histopathological picture might suggest that more severe patients who overcome the infection will present residual lesions with fibrosis and destructuring of the pulmonary parenchyma. Therefore, after the acute phase, our efforts should focus on the clinical and functional follow-up of residual lesions.
Monitoring strategies in patients with other respiratory diseases will also have to be redesigned, given the difficulties they may face in attending visits for scheduled consultations or additional examinations. For example, patients with COPD, which is a risk factor for a more severe Covid-19 course,4 will continue to need follow-up of their disease to improve their symptoms and prevent exacerbations. The same applies to virtually all other chronic respiratory diseases, including asthma, bronchiectasis, idiopathic pulmonary fibrosis, and vascular lung disease.
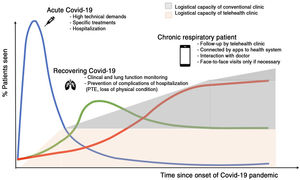
In the post-Covid-19 era (Fig. 1), we will have to reorganize our approach to respiratory disease outpatient care and how we assess which patients require lung function testing, imaging techniques or invasive techniques that need to be performed in a health center, which patients can be monitored by video consultation or telephone call, and which need to be seen at home by primary care personnel.5 In this setting, we will also have to learn which diagnostic or clinical follow-up tools can be used by patients in their home to provide us with sufficient information for decision-making. Some of them, such as the questionnaires we use in routine clinical practice (CAT©, ACT©), could be included in mobile applications that could help the clinician determine which patients are controlled and which are not. Others, such as pulse oximeters using smartphone flashes or built-in smartphone spirometers that do not require additional components, will need to be developed quickly so we can be prepared for the follow-up of patients with respiratory disease in the post-Covid-19 era.
Please cite this article as: Alcázar-Navarrete B, París JM, Sánchez FJM. Seguimiento del paciente con enfermedad respiratoria en la era post-COVID-19: ¿estamos preparados? Arch Bronconeumol. 2020;56:685–686.