The aim of this article is to highlight some concerns regarding lung cancer screening with computed tomography (CT) through an analysis of scientific literature. The publication of the National Lung Screening Trial in 2011 has revealed that CT screening of smokers and ex-smokers in three annual rounds reduces lung cancer mortality a 20% when compared with thorax X-ray screening. The first limitation of this screening modality is its lack of downstaging in successive screening rounds compared with the initial round. Also, lung cancer screening with CT has a low positive predictive value, similar to the percentage of unnecessary surgeries performed in false positives. Another problem is that, at present, the burden of lung cancer overdiagnosis is not known. It is to be expected that if overdiagnosis occurs when thorax X-ray screening is used it will be greater when using CT. CT, even at low doses, exposes patients to high levels of radiation. Dealing with positive nodules entails an even higher radiation dose and the number of cancer cases induced by radiation in patients screened with CT is not known. Lastly, published studies on lung cancer CT screening are vastly heterogeneous. They include different age groups, different types of smokers and ex-smokers and different tomogram thickness, making the results hardly comparable. In this context we do not recommend lung cancer screening with CT for smokers or ex-smokers outside of the context of individual counseling.
El objetivo de este artículo es destacar la problemática que afecta al cribado del cáncer de pulmón con tomografía computarizada (TC) mediante un análisis exhaustivo de la literatura científica. La publicación del National Lung Screening Trial en 2011ha indicado que el cribado con TC de fumadores y exfumadores en 3 rondas anuales reduce la mortalidad por cáncer de pulmón en un 20% cuando se compara con el cribado con radiografía de tórax. La primera limitación de esta modalidad de cribado es la falta de descenso en la estadificación en rondas sucesivas de cribado cuando se compara con la ronda inicial. El cribado de cáncer de pulmón con TC también tiene un bajo valor predictivo positivo, similar al porcentaje de cirugías innecesarias realizadas en los falsos positivos. Otro problema es que, actualmente, el sobrediagnóstico del cáncer de pulmón es desconocido. Podemos suponer que si existe sobrediagnóstico cuando la técnica de cribado es la radiografía de tórax, este será mayor cuando se utilice TC. La TC, incluso a dosis bajas, expone a los pacientes a niveles elevados de radiación. La detección de nódulos positivos implica una mayor exposición a radiación, y el número de casos de cáncer inducidos por radiación en los pacientes cribados con TC es desconocido. Por último, los estudios publicados sobre el cribado de cáncer de pulmón con TC son tremendamente heterogéneos. Incluyen diferentes grupos de edad, diferentes categorías de fumadores y exfumadores y diferentes grosores en los cortes de la TC, lo que convierte los resultados en difícilmente comparables. Con estos datos no recomendamos el cribado de cáncer de pulmón con TC de baja dosis para fumadores o exfumadores fuera del contexto de la recomendación individual.
Lung cancer is an important healthcare problem. In developed countries, it is the cancer with the highest mortality in males, while in women it is the fourth most frequent cancer and the second in terms of mortality. In 2008, lung cancer was responsible for 13% of all cancer cases and 18% of all cancer deaths.1
Lung cancer is also a lethal disease. According to the EUROCARE IV study, five-year survival in Europe is 12%.2 This datum has hardly varied in the last 30 years, and approximately 85% of subjects with lung cancer will die due to this disease.3 This poor prognosis is fundamentally due to the fact that, at the time of diagnosis, only 15% of tumors are located4 and are able to be surgically resected. A screening test that could detect the disease in an early phase could prevent dissemination of the disease, providing for early treatment and prolonging the life of the patient.
Lung cancer has multiple risk factors, although 85%–90% of all cases are attributed to smoking.5 If tobacco consumption were eliminated, lung cancer would be far from the top spots in the cancer incidence ranking. Thus, any early diagnosis screening should be directed at smokers. Many aspects of smoking influence the risk for lung cancer: smoking duration and intensity, inhalation depth or type of tobacco consumed.6 It is known that the duration of tobacco habit has greater influence than its intensity7 and, therefore, a person who has smoked a pack a day for 20 years has a lower risk for lung cancer than a person who has smoked half pack for 40 years, even though both have an accumulated tobacco consumption of 20 pack-years.
An exhaustive search has been going on for a diagnostic test to be used in the early detection of lung cancer. Numerous studies have been published, to different degrees of quality, in order to establish the suitability of different diagnostic tests. Low-dose computed tomography (LDCT), chest radiography and sputum analyses have been the most widely used. Although these studies indicate a greater effectiveness of CT for early detection,8,9 none has been able to demonstrate greater survival of the patients screened with LDCT compared with a control group. The results of the National Lung Screening Trial have been the first to show longer survival of patients screened with LDCT versus chest radiographs.10 The results from the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial,11 published in November 2011, show that annual screening with chest radiography (4 annual rounds) did not lower mortality due to lung cancer, which ruled out chest X-rays as a screening test for lung cancer. A recent publication, however, has shown several limitations of LDCT for lung cancer screening.12 This present article enumerates even more limitations than the mentioned publication, with the aim to generate debate among medical professionals through an analysis based on scientific evidence before this technology becomes established in clinical practice.
The National Lung Screening TrialThe National Lung Screening Trial (NLST) is a randomized clinical trial financed by the U.S. National Cancer Institute10 that included 53454 asymptomatic smokers and ex-smokers, with accumulated smoking histories of at least 30 pack-years, between the ages of 55 and 74. Its objective was to compare two screening methods, LDCT and chest radiography, in order to observe possible differences in mortality. The participants were randomized to receive LDCT or chest X-ray and approximately half of the subjects in each group were ex-smokers. They were screened at the start of the study and after one and two years of follow-up, with a total of three consecutive screening tests. The participants were followed another five years, with a program compliance of about 93% in both groups. The population included was highly motivated, urban and screened at hospitals with extensive experience in the analysis of imaging tests and the management of suspicious lung nodules. Mean follow-up was 6 and one-half years.
The following is a description of the most relevant results. The positive screening percentages in the LDCT group were 27.3%, 27.9% and 16.8%, versus 9.2%, 6.2% and 5.0% in the chest X-ray group for each round. During screening, 39.1% and 16% of the participants in the LDCT and chest radiography groups, respectively, had a minimum of at least one positive result. In the three rounds, 96.4% in the LDCT group and 94.5% in the radiography group were false positives. A total of 1060 cases of lung cancer were diagnosed in the LDCT arm: 649 after a positive screening, 44 after a negative screening and 367 cases among participants who had missed a screening test or after the end of the screening. There was a total of 18146 positive CT screenings, and cancer was confirmed in 649 cases, with a positive predictive value of 3.6%. The staging of the tumors detected in each CT screening round is included in the supplemental material of the original article and has been summarized in Table 1 of this present article. In the CT screening group, lung cancer deaths were 20% lower than those of the chest radiography screening group. This difference was 6.7% when the total number of deaths was considered. As for adverse effects, 16 participants in the CT group died after an invasive diagnostic procedure, six of whom did not have lung cancer.
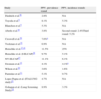
Lung Cancer Stages Detected With CT According to Screening Round.
| Stage | First round, % | Second round, % | Third round, % |
| IA or IB | 54.6 | 59.01 | 63.9 |
| IIIA, IIIB or IV | 37.8 | 31.2 | 30.4 |
One of the aims of a screening program is to detect the disease in an early phase, requiring less aggressive treatment and resulting in faster recovery. When a screening program is begun, it is expected that the first round will detect prevalent cases, with no dominating stages. Successive rounds will detect cases in which early stages predominate when compared with the first round.13 The time period between two consecutive screening tests should be short enough so that cancers detected after the screening do not have time to progress to advanced stages. However, studies published about lung cancer screening trials with CT do not present these characteristics. Table 2 shows the lung cancer stages detected in the initial and successive screenings for several studies.10,14–23 Some articles do not differentiate between the staging from initial and successive rounds, and analyzing a possible decrease in stages is therefore not possible.24
Lung Cancer Stages Detected With CT According to Prevalence or Incidence.
| Study | Stage in the prevalence screening | Stage in the incidence screenings | |
| Second round | Third round | ||
| NLST10 | IA: 45.9%IB: 9.2%IIA: 3.4%IIB: 4.1%IIIA: 11.6%IIIB: 10.2%IV: 16.0% | 47.5%11.5%6.0%3.8%7.7%10.4%13.1% | 50.4%13.5%3.5%2.2%6.5%8.7%15.2% |
| Fujikawa et al.14a | IA: 100% | Undetected cancers | |
| Bach et al.15,16 | The advanced cancers detected (stages III and IV) surpass those predicted by the model. It is not specified which were detected in an initial screening and which are from successive screening rounds (3.9 years of follow-up on average). | NA | |
| Henschke et al.17,18 | I: 85%II: 3.7%III: 11.3%IV: 0% | IA: 85.7%II: 0%IIIA: 14.3%IV: 0% | |
| Swensen et al.19b | I: 71.0%II: 12.9%III: 6.4%IV: 3.2%Limited small-cell lung cancer: 6.5% | I: 50.0%II: 11.8%III: 17.7%IV: 0%Limited small-cell lung cancer: 17.7%Unknown: 2.9% | |
| Wilson et al.20 | I: 58.4%II: 3.8%III: 28.3%IV: 7.5%Small-cell lung cancer: 1.9% | I: 37.5%II: 4.2%III: 25.0%IV: 4.2%Small-cell lung cancer: 33.3% | |
| Pastorino et al.21 | I: 54.5%II: 9.1%III: 27.2%IV: 9.1% | I: 100%II: 0%III: 0%IV: 0% | |
| ITALUNG study22 | I: 52.4%II: 9.5%III: 9.5%IV: 19%Limited small-cell lung cancer: 9.5% | NA | |
| Lung screening study23 | I: 53.3%II: 10.0%III: 20.0%IV: 10.0%Unknown: 6.7% | I: 25.0%II: 0%III: 62.5%IV: 12.5%Unknown: 0% | |
As shown in Table 2, most studies do not indicate a decrease in stages in rounds after the initial round. The frequency of advanced cancers either remains stable or even increases after the first round. The NLST detects a slight increase in stages IA and IB in the second and third rounds and a slight decrease in stages III and IV in the third round compared with the first round (37.8% vs 30.4%).10 The study by Pastorino et al. has observed a significant increase in the percentage of cancer cases in an initial phase detected in the incidence rounds.21 Contrarily, the study by Wilson et al. indicates a significant decrease in the cases detected in stage I in the second round versus the first round, together with a slight increase in the number of stage III and IV cases detected in the second round.20 The remaining studies indicate an increase in the percentage of cancer cases in advanced stages detected in the rounds of incidence compared with the cancers detected in the initial screening (prevalence screening).17–19,23
These results indicate that the expected decline in cancer stages does not occur in patients who participate in consecutive screening rounds. This observation is compatible with Bach's hypothesis of a bipartite model for lung cancer, which affirms that some lung cancers grow rapidly and are very aggressive, while others grow at a slower pace. In the latter type, a screening program could modify their clinical course.16 These findings also imply that one of the requirements for a screening program would not be met, since the clinical course of the disease would not be modified. If the stages detected are not lower and there is an increase in the percentage of advanced-stage cancer detected in the screening rounds, then lung cancer screening would be demonstrated to be useless.
The Positive Predictive Value of Lung Cancer Screening With CT is Low and is Similar to the Percentage of Surgeries Done in Patients Without Lung CancerSmall non-calcified lesions detected with LDCT are classified as positive, and LDCT has much greater resolution when compared with other screening techniques. Table 3 reflects a positive predictive value for CT that ranges between 2.8% and 11.5% in the initial screening.8–10,17–23,25–29 Only three studies reveal a positive predictive value above 9%,17,27,29 with a range from 1.6% to 25% in the incidence screening rounds. In most studies, positive predictive value is around 5% in the incidence screening rounds. The NLST obtained a positive predictive value of 3.8% in the initial round and 5.2% in the last round. Many published studies, such as DANTE, do not differentiate between the positive results in the first round from the remaining rounds; therefore, the positive predictive value for each screening round cannot be calculated.24
Positive Predictive Value (PPV) of CT for Screening Lung Cancer in the Prevalence and Incidence Rounds.
| Study | PPV, prevalence round | PPV, incidence rounds |
| Diedrich et al.26 | 2.8% | NA |
| Toyoda et al.8 | 8.1% | 5.3% |
| Blanchon et al.9 | 5.3% | NA |
| Aberle et al.10 | 3.8% | Second round: 2.4%Third round: 5.2% |
| Croswell et al.28 | 7.0%a | NA |
| Tockman et al.25 | 6.9% | NA |
| Henschke et al.17,18 | 11.5% | 25% |
| Henschke et al. (I-ELCAP)29 | 9.7% | 5.1% |
| NY-ELCAP27 | 11.1% | 6.1% |
| Swensen et al.19 | 4.1% | 4.1%a |
| Wilson et al.20 | 3.6% | 1.6% |
| Pastorino et al.21 | 5.1% | 9.7% |
| Lopez Pegna et al. (ITALUNG study)22 | 4.7% | NA |
| Gohagan et al. (Lung Screening Study)23 | 8.9% | 3.3% |
Another result that is expected in a screening program is that the positive predictive value should increase in the incidence rounds when compared with the initial screening. Many of the positive lesions found in the first round will persist in the second round without showing any growth and, therefore, should not be classified as positive findings in successive screenings. In only two studies17,21 does the positive predictive value increase in the incidence rounds when compared with the prevalence round (Table 3). One of these studies is the I-ELCAP, where the positive predictive value increased from 11.5% in the first round to 25% in the incidence rounds. This study has the highest positive predictive value in both rounds.29
When there is a positive finding, the lesion should be examined to determine if it is malignant, requiring treatment. More than 90% of positive findings do not correspond with lung cancer. From the total number of nodules detected, around 98% are benign.30 Thus, in the NLST, about 90% of positive screenings required diagnostic evaluation.10 The majority of the lesions detected in the screening are less than one centimeter in diameter.31 Given that the risk for a lesion being cancerous depends directly on its diameter, there is controversy regarding the management of subcentimeter nodules, and different studies propose different protocols. For small nodules, CT may be done in 3 to 6 months, and, if there is an increase in size, an invasive test should be used to confirm the existence of malignant cells. The guidelines of the American College of Chest Physicians (ACCP) has specific criteria about the management of lung nodules in smokers.31 It recommends periodic CT depending on the size of the nodule, and for those nodules smaller than 4mm, annual CT is recommended. When positive findings are detected, the pretest probability of a positive lesion is crucial. The lesion diameter, patient smoking history, being a current or ex-smoker and patient age are all factors that influence this probability. None of the studies analyzed has applied these criteria with positive findings, and all the lesions have been treated in the same manner within each study, regardless of the individual characteristics of the participants.
The invasive analysis of a positive nodule has side effects that range from minimal to death. In a certain percentage of positive cases, it will be necessary to carry out a surgical procedure like mediastinoscopy (when lymphadenopathies are found on computed tomography), thoracoscopy or thoracotomy. In NLST, surgery was done in 4.2% of positive cases in the first round, 2.9% of the positive cases in the second round and in 5.6% in the third round.10 Of all the surgical procedures (mediastinoscopy or mediastinotomy, thoracoscopy and thoracotomy), thoracotomy was used in almost half of the cases in all the screening rounds. For positive patients, the percentage of surgical procedures surpasses the percentage of individuals with confirmed lung cancer by 0.4%–0.5%, indicating that approximately this percentage of positive patients receive unnecessary surgical interventions. In the NLST, 164 patients underwent unnecessary surgical interventions, showing that 0.9% of all the positive patients were subjected to surgery in which no lung cancer was detected (164/total number of positive results in the three rounds=18146). These percentages are significant when we take into account their morbidity and mortality, even though in the NLST only 0.06% of the positive patients had relevant complications after invasive surgery.10 The mortality rate associated with surgical resections of lung cancer is situated between 1% and 4%, which also depends on the number of surgeries performed at each hospital.32 When the tumor is in its initial phases, postsurgical mortality descends to 1%–2%.33
Table 4 shows the surgical interventions on benign lesions in those studies that indicate this result.9,10,19–21,24,28 The percentage of unnecessary surgeries ranged from 0.9% (NLST)10 to 13% (DANTE),24 while in most studies it was around 2%. This datum was not reported for the International Early Lung Cancer Action Project (I-ELCAP) study.29
Surgical Interventions in Individuals With Positive Screening that have a Later Benign Result.
| Study | Surgical interventions in positive lesions that are not lung cancer |
| Blanchon et al.9 | 2% (3 thoracotomies in a total of 152 non-calcified nodules) |
| Croswell et al.28 | 2% |
| Infante et al.24 | 13% (6 thoracotomies out of a total of 46 demonstrated a benign lesions) |
| Wilson et al.20 | 1.6% (video-assisted thoracoscopy or thoracotomy) |
| Swensen et al.19 | 2% (approximately) |
| Pastorino et al.21 | 2.3% received unnecessary surgery in the first screening vs 0.9% in the second round |
| Aberle et al.10 | 0.9% of unnecessary surgeries (164 in 18146 positive subjects) |
The aforementioned results indicate how false positives can have a direct effect on screened subjects. Moreover, a positive result carries a severe psychological burden for patients. Most patients are aware of the fact that lung cancer is a potentially lethal disease, so a positive result affects the entire family. During the time that transpires between a positive screening result and the moment when the disease is ruled out, the patients and their families live under a great amount of anxiety.34 Even when the patients are properly informed about the high number of false positives involved in screening tests, it is unavoidable that they will be worried. In addition to the psychological burden itself, the direct and indirect costs of false positives can be high, including the transportation costs to and from the hospital and a potential loss in productivity at the workplace due to absenteeism or poor work performance.
Overdiagnosis in Lung Cancer Screening is Probably HighOverdiagnosis can be defined as: (1) the cancer did not evolve or even diminish; (2) the cancer progresses so slowly that the patient dies from other causes without ever having developed cancer symptoms. The latter depends on three factors: (a) size of the lesion at the time of detection; (b) rate of growth; and (c) competing risks of death. Because, at the time of the detection, it cannot be known which cancers are overdiagnosed and which are not, a diagnostic approach is necessary in all of them. One of the main causes of overdiagnosis is screening35,36 and, in the case of lung cancer screening, overdiagnosis is not just a possibility, it is a fact. This was seen in the Mayo Lung Project, which observed that the screening arm with chest radiography still had an excess of cancer cases detected after 16 years of additional follow-up.37 If the overdiagnosis occurs using chest X-ray, it would be expected to be even greater when CT is used, given its higher resolution. In fact, CT detects two or three times more positive nodules than chest radiography. Population screenings with CT can detect a substantial number of indolent tumors and benign lesions as well as potentially lethal nodules.38 Overdiagnosis, by definition, is classified as an unnecessary case and, likewise, all the procedures ordered due to an overdiagnosed positive nodule are also unnecessary. Studies that analyze lung cancer screening with CT mention the possibility of overdiagnosis, although it has not been formally analyzed in any of these studies. It is practically impossible to classify a malignant positive nodule as overdiagnosis after it has been detected. The logical step is to analyze the nodules and verify the presence of cancer cells. The NLST observes overdiagnosis in the CT screening arm. This screening systematically detects more cancer cases than screening with X-ray in all the screening rounds (similar to other studies). Nevertheless, to confirm this, a lengthy follow-up of both groups would be necessary.10,35 Moreover, the fact that the number of positives only declines between the second and third rounds and remains the same between the initial round and the second round suggests the possibility of overdiagnosis. In the NLST, it is not possible to quantify the presence of overdiagnosis compared with standard care since the comparison group had been studied with chest radiography.
The management of overdiagnosis is extremely difficult in cancer screening programs and the perspective is even more difficult in lung cancer screening with CT. Adopting a conservative approach to suspicious lesions detected with screening entails the use of imaging techniques,31 which expose the patients to high levels of radiation. Nevertheless, this would seem to be the least harmful way to distinguish between two lesions measuring 0.8cm in diameter, one of which is aggressive and potentially lethal, while the other is indolent, slow-progressing or even recessive. This hypothesis is supported by results that indicate that subjects in stage I detected by cancer screening who do not receive treatment die from this disease in the end.39
Using Low-Dose Computed Tomography as a Screening Test for Lung Cancer Increases the Risk for Radiation-Induced CancerMost recent studies about lung cancer screening have used low-dose CT as a screening test. This screening method has many advantages, like being able to detect subcentimeter nodules, but it also has disadvantages because it exposes subjects to much higher radiation doses than chest radiography. One low-dose CT is equal to approximately the natural radiation that a person receives in 3 years, or 400 chest X-rays. Other screening tests are much less harmful, such as mammography, which is equivalent to the natural radiation a person receives over the course of 3 months.40 Simulation studies have indicated that around 1.5%–2% of all cancers diagnosed in the United States are caused by radiation received from computed tomographies.41 In the United States, the exposure to medical radiation has surpassed the exposure to natural radiation due to the increased use of diagnostic imaging tests.42,43 Furthermore, lung cancer is one of the most frequent cancer types induced by radiation,44 as demonstrated by recent modeling studies. It has been estimated that there is one cancer death induced by radiation for every 2000 computed tomographies (assuming an effective dosage of 10 per tomography and a 5% risk per sievert).45 The individuals screened with a normal result should be screened annually. This situation would mean a lower risk for a screened individual due to the radiation received. When a suspicious lesion is detected, there should be a follow-up to check its growth every 3–6 months, exposing the subjects to high accumulated doses of radiation (using diagnostic CT involves more radiation). Furthermore, it has been suggested that there is a sub-multiplicative relationship between radiation and tobacco,46 and individuals screened for lung cancer are all either smokers or ex-smokers. It has been observed that the risk for cancer due to radiation descends with age, but this is not true for lung cancer. The doses of radiation used with LDCT are situated in the range of radiation for which there is direct evidence of an increase in the risk for cancer in atomic bomb survivors. In lung cancer, the dose of radiation with this type of tomography is 2.5–9mGy. The excess risk for lung cancer for a dose of 5.2mGy in smokers over the age of 50 who have received an annual screening test until the age of 75 is 0.85% for women and 0.23% for men. Thus, annual screening could therefore increase lung cancer deaths by 1.8% in the United States. Delaying the age for the initial screening from 50 to 60 would considerably reduce the risk for radiation-induced cancer, and changing the frequency of screening from annual to biannual would cut radiation doses in half.10 The study that provided these results, however, did not take into account other potential tests for diagnosing lung cancer, such as positron-emission tomography (PET), and the risks could be underestimated.
Lung Cancer Screening With Computed Tomography has an Important Economic and Organizational ImpactA lung cancer screening program with CT for smokers would have a significant economic impact. There is a large number of subjects to be screened in a program of these characteristics, all of whom would need to be located and contacted. This would not be easy, and patient medical files would need to be used to locate them.47 There are no databases of active smokers or ex-smokers and the reliability of the medical files to locate them is arguable. Given the high number of subjects at risk, it would be necessary for tomographs to be dedicated exclusively to the screening program, with radiologists, technicians and auxiliary staff assigned to each screening unit. These units should work double shifts to increase their effectiveness, and therefore the staff per tomograph would be double. Each CT currently costs some 366.32€,48 to which we should add the cost of complementary tests when there is a positive result (adding the cost of the tomography, the personnel and preparatory requirements of the tests and the loss of work productivity incurred by medical appointments).47
For a hypothetical population of one million people over the age of 18 in which only those subjects aged 50–75 were screened (35% of the population, for example), with a prevalence of smoking of 25% and around 90% of the smokers had consumed more than 20 pack-years, the number of subjects screened would be 1000000×0.35×0.25×0.9=78750 (7.8% of the entire population over the age of 18). The cost of the screening tests alone, at 300€ per test, would be a total of 23625000€. By applying the results of the NLST study, in the first round there would be 21499 (27.3%) positive results that would need later testing. From these positive results, 3.6% would be confirmed as lung cancer and the rest would be false positives. Therefore, 774 cases would be detected. The cost of a false-positive in a male is estimated to be $1171 for one year.49 In a second screening round, the number of cancers detected would probably decrease since prevalent cancers have been ruled out, but the cost of the screening program continues (with a possible drop in false positives). Some cost-effectiveness studies favor lung cancer screening,50 but their estimations are based on the ELCAP study, which has obtained the best results of all the studies published, although it presents many limitations.51,52
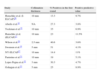
Other AspectsThere is great variability in the characteristics of lung cancer screening studies (Table 5). Regarding the periodicity of the screening, there is consensus that the ideal interval is one year, but there is much variability about at what age screening should start and end. Another factor that influences the number of positive lesions is the prevalence of smoking in the different studies. Some studies include never-smokers,8,14 in whom the probability for positive results is low and, even more important, the characteristics of the smokers vary between the populations screened (Table 5). Many studies simply use pack-years to include smokers, without considering that the time transpired since quitting smoking reduces the possibility for developing lung cancer. There are large differences in the age of the screened subjects; while some studies start screening at age 40,29 others start at age 60.17,24 Many studies do not specify an age limit for screening, even though the remaining life expectancy of a person who is going to be screened with computed tomography should be at least 10 years.39
Smokers’ Ages and Characteristics as well as Screening Intervals of the Reviewed Studies.
| Study | Age (range) | Smokers’ characteristics | Screening interval |
| Aberle et al.10 | 55–74 | ≥30 pack-years; subjects had quit smoking in the previous 15 years | 1 year |
| Henschke et al. (I-ELCAP)29 | ≥40 | Smokers, ex-smokers or never-smokers exposed to passive smoke or exposed to occupational lung carcinogens | 7–18 months |
| Henschke et al. (ELCAP)17,18 | ≥60 | Smoking ≥10 pack-years; fit for thoracic surgery | 6–18 months |
| Tockman et al.25 | ≥45 | Smokers and ex-smokers ≥30 pack-years with moderate obstruction on spirometry (FEV1/FVC<70%) | NA |
| Infante et al.24 | 60–74 | Smokers or ex-smokers of at least 20 pack-years | 1 year |
| Wilson et al.20 | 50–79 | Smokers or ex-smokers of at least 37.5 pack-years; <10 years since quitting | 1 year |
| Swensen et al.19 | 50–85 | Smokers or ex-smokers; <10 years since quitting | 1 year |
| NY-ELCAP27 | ≥60 | Smoking history ≥10 pack-years; fit for thoracic surgery | 7–18 months |
| Pastorino et al.21 | ≥50 | Smokers or ex-smokers of at least 20 pack-years | 1 year |
| Lopes Pegna et al.22 | 55–69 | At least 20 pack-years in the last 10 years | 1 year |
| Gohagan et al.23 | 55–74 | Smokers or ex-smokers of 30 pack-years; ex-smokers who had quit smoking in the last 10 years | 1 year |
Computed tomography slice thickness is especially important. The thinner the collimation, the greater the number of nodules located. Most studies include 10mm-slices,10,17,21,27 and those nodules with smaller diameters are less likely to be detected. Studies using thinner slices detect more nodules, involving additional explorations afterwards and greater doses of radiation. It seems reasonable that the screening interval should be extended when thinner slices are used, and shortened when poorer resolution is used. It can be observed in Table 6 that the studies with thinner cuts have a greater prevalence of positive nodules20,22 and lower positive predictive value in the first round. Lastly, the probability for positive results will also depend on the underlying characteristics of the population. Thus, in areas where there is a higher prevalence of tuberculosis or respiratory diseases, the probability for positive findings is elevated.
Collimation Thickness, Positives in the First Round and Positive Predictive Value.
| Study | Collimation thickness | % Positives in the first round | Positive predictive value |
| Henschke et al. (I-ELCAP)56 | 10mm | 13.3 | 9.7% |
| Aberle et al.10 | NA | 27.3 | 3.8% |
| Tockman et al.25 | 10mm | 35 | 6.9% |
| Hanschke et al. (ELCAP)17 | 10mm | 23 | 11.5% |
| Wilson et al.20 | 2.5mm | 40.6 | 3.6% |
| Swensen et al.19 | 5mm | 51 | 4.1% |
| NY-ELCAP27 | 10mm | 14.4 | 11% |
| Pastorino et al.21 | 10mm | 19 | 5.1% |
| Lopes Pegna et al.22 | 3mm | 30.3 | 4.7% |
| Gohagan et al.23 | 5mm | 25 | 8.9% |
Finally, many studies have detected a relatively high frequency of interval cancer. As for the total number of cancers found in the incidence rounds, the cases of interval cancer are 6.8%,29 5.9%19 and 6.8%.10 These findings support Bach's hypothesis of a bipartite model for lung cancer.16
Contextualizing the Results and Proposed Steps for ActionThe results observed for lung cancer screening with CT show many limitations. The main limitation is an extremely low positive predictive value, which means a very high number of false positives. False positives expose the individuals to unnecessary and damaging treatments and even death. Although it is expected for a population screening program to have a low positive predictive value since the negative predictive value is the key parameter, the results for lung cancer seem unacceptable. Moreover, the diagnostic approach to a positive nodule involves a certain risk of morbidity. Some nodules are located in anatomic areas that are not accessible through bronchoscopy or percutaneous transthoracic needle aspiration (biopsy or cytology) and the only way to determine the nature of the nodule is by means of a surgical procedure. New diagnostic procedures provide easier access to these nodules53 but there are still inaccessible areas. There may be metastasis even when the primary tumor is small. Centrally located tumors or those in the respiratory tract are not easily detected with a screening tomography.54 The estimated positive predictive value of 5% should be weighed against the 2% possibility of having unnecessary surgery. The deaths avoided should be weighed against the effects of radiation, plus anxiety, plus unnecessary surgery, plus direct and indirect costs.
Despite the results of the NLST and other studies with promising results like I-ELCAP, the reasonable option is not to recommend lung cancer screening with CT. It is better to unite our efforts to make sure that health-care professionals are alerted to lung cancer symptoms, while improving their training and making smokers aware of the risk they have for developing lung cancer. More resources should be dedicated to anti-smoking advice and education as well as public health-care policies with the aim to avoid the onset of tobacco consumption among teens. These steps should be accompanied by the development of new studies that define in which population subgroups tomography screening would be cost-effective. These subgroups could be outlined by the quantity of tobacco smoked in a lifetime (high), age group, coexistence of risk factors (risk of occupational lung cancer, exposure to high concentrations of radon) and the presence of other respiratory diseases or, alternatively, with timely screenings of individuals selected in accordance with their individual characteristics. As has been recently published, a change is needed in screening policies55 and this is particularly important in lung cancer, where deep reflection is currently necessary. The American College of Chest Physicians and the American Thoracic Society are going to put into practice guidelines for clinical practice suggesting annual screening with LDCT for smokers aged between 50 and 74 with an accumulated tobacco consumption of more than 30 pack-years,12 although with clear warnings. Perhaps the most important is that LDCT should not be offered outside an organized program. It is necessary to promote a thought-provoking debate amongst the health-care professional involved (pulmonologists, oncologists, radiologists, thoracic surgeons, epidemiologists, administrators and patients) before starting up an unorganized population screening program, which would benefit only a few individuals while possibly being harmful for many more, including health-care organizations.
Conflict of InterestNone to declare.
Please cite this article as: Ruano-Ravina A, et al. Cribado de cáncer de pulmón con tomografía computarizada de baja dosis después del National Lung Screening Trial. El debate continúa abierto. Arch Bronconeumol. 2013;49:158–65.