We have carried out a review of the literature after the presentation of a case of Niemann-Pick (N-P) disease type B reporting the radiological findings with special emphasis on lung affectation. The patient is 40 years old and was diagnosed at the age of 6 with possible N-P disease suspected due to the presentation of hepatosplenomegaly and reticular pattern on chest radiography, with initially normal lung function tests. Said diagnosis was confirmed by measuring the activity of acid sphingomyelinase (ASM) enzyme in skin fibroblast cultures and by demonstrating the presence of mutations in the ASM gene. In cases of storage disease, lung affectation should always be considered, and the most reliable radiological technique is high-resolution computed tomography. Although the “crazy-paving” pattern is not the most specific for this pathology, N-P disease should be included in the differential diagnosis.
Tras la presentación de un caso de enfermedad de Niemann-Pick (N-P) tipo B se realiza una revisión de la literatura en la que se describen los hallazgos radiológicos, con especial hincapié en la afectación pulmonar. Se trata de un paciente de 40 años diagnosticado a los 6 años de posible enfermedad de N-P sospechada por presentar hepatoesplenomegalia y patrón reticular en radiografía de tórax, con pruebas de función respiratoria inicialmente normales. Dicho diagnóstico se confirmó mediante medición de la actividad de la enzima esfingomielinasa ácida (ASM) en cultivo de fibroblastos de piel y demostración de la presencia de mutaciones en el gen de la ASM. Ante una enfermedad de depósito habría que tener siempre en cuenta la afectación pulmonar, y la técnica radiológica más fiable es la tomografía computarizada de alta resolución. Aunque el patrón encrazy-paving no es el más específico de esta patología, la enfermedad de N-P debería estar en el diagnóstico diferencial.
Niemann-Pick disease (N-P) is a lysosomal storage disease in which there is an accumulation of sphingomyelin1 in different tissues. It affects multiple organs and has been classically divided into two subtypes according to phenotype: types A and B.1 A third subtype (type C) has also been described, but it is caused by a different genetic alteration. In type A, there is a neurodegenerative disorder with premature death. Type B causes chronic visceral affectation,2 frequently with later lung affectation. Radiographically, the lung affectation is characterized by an interstitial pattern associated with ground glass opacities. There is a week correlation between lung function and interstitial disease.3 We present a case of N-P disease type B with pulmonary and hepatic affectation. The objective is to describe the pathologic findings of this disease in the lungs, as seen on both simple chest radiography and high-resolution computed tomography (HRCT), and their correlation with lung function testing. We also include a review of the literature.
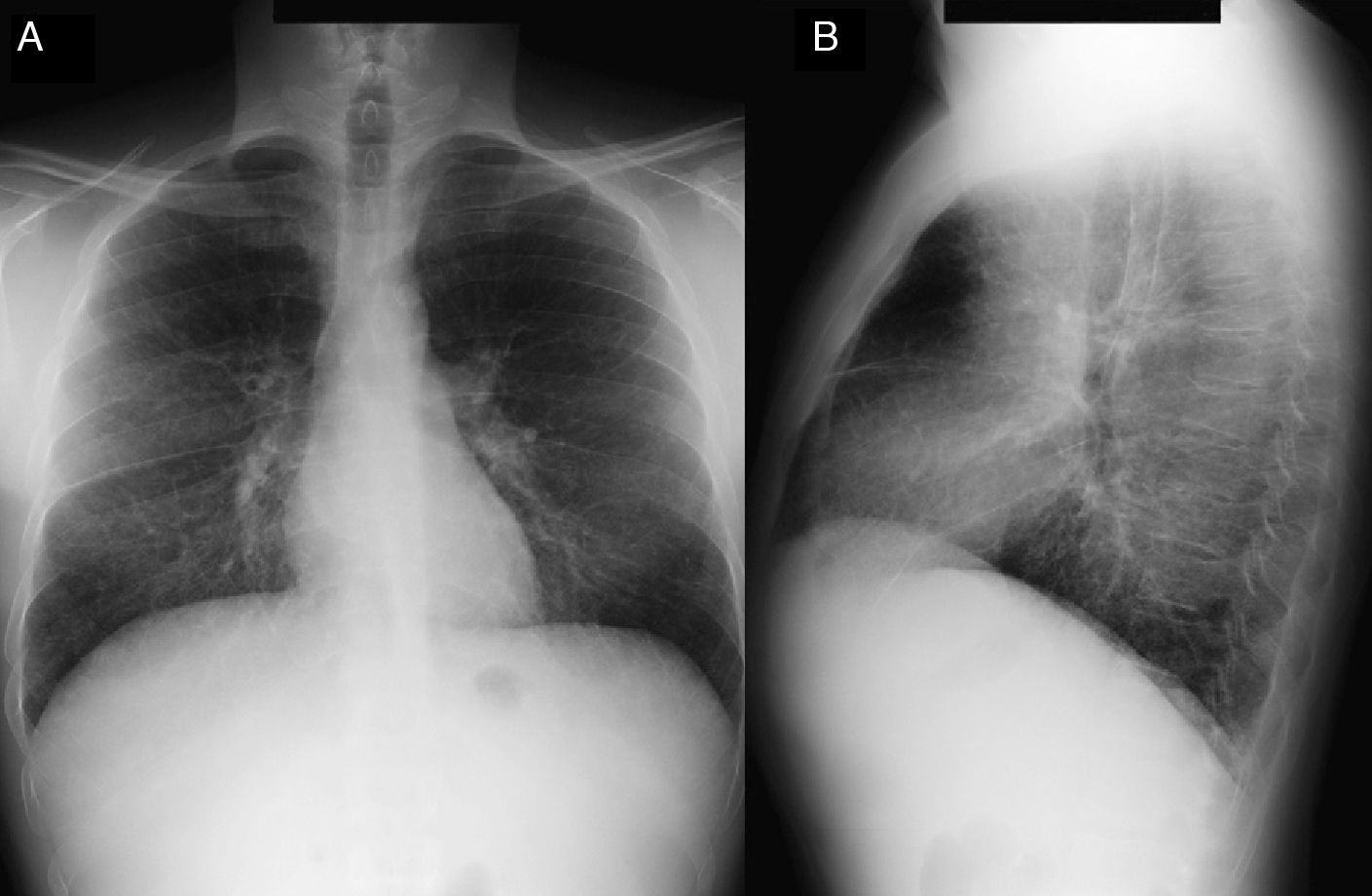
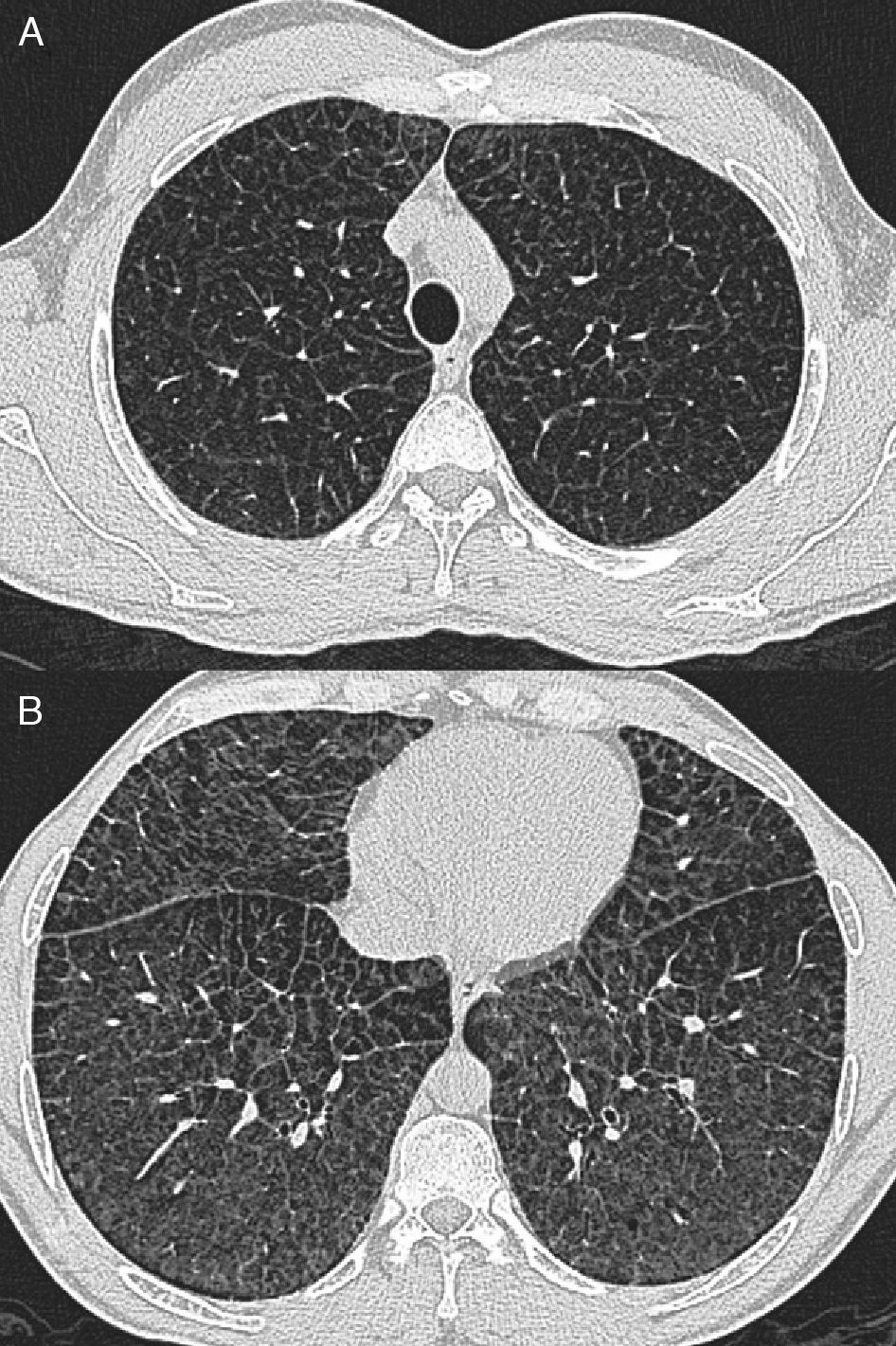
Case ReportA 40-year-old male diagnosed with N-P disease with hepatic and pulmonary affectation. Personal history included hepatosplenomegaly diagnosed at the age of 6–7 months. The patient was hospitalized at the age of 6 due to symptoms of asthenia, anorexia, deterioration and fever. Posteroanterior and lateral (PA-L) chest X-rays revealed diffuse reticular pattern. Given the radiographic findings and presence of hepatosplenomegaly, deposition disease was suspected. Rectal mucus and hepatic biopsies were suggestive of N-P disease (lipid-laden macrophages were observed). Neurological examination and respiratory function tests were normal. The diagnosis was confirmed when the patient was 20 using skin biopsy with fibroblast cultures, which confirmed a marked acid sphingomyelinase (ASM) deficiency characteristic of N-P disease that, supporting the clinical diagnosis, would be type B. At the age of 38, a molecular diagnosis revealed two mutations in the SMPD gene (heterozygosis in mutation p.R608del). The patient currently continues to be seen at the pulmonology and hepatology outpatient consultations, and he presents intermittent jaundice and maximal exertion dyspnea (MRC scale 0). On physical examination, minimal bibasilar crackles, subconjunctival jaundice and hepatosplenomegaly are observed. Neurological examination is normal. In the work-up, the most noteworthy results are: total bilirubin 4.17mg/dl; GOT 38IU/l; GPT 45IU/l; total cholesterol 221mg/dl. Lung function tests show a normal ventilatory pattern (FVC 3.84 [87.7%]; FEV1 3.13 [86%]; FEV1/FVC 81.58%; TLC 5.26 [81.8%]) and a mild alteration in the gas exchange (DLCO 57.5%). Radiographic findings on PA-L chest X-ray (Fig. 1A and B) include diffuse reticular interstitial affectation observed in the pulmonary parenchyma, predominantly in the middle and lower fields. HRCT (Aquilion Toshiba, 64-detector) (Fig. 2A and B) demonstrated diffuse ground-glass affectation, although predominantly in the lower lobes with subpleural septal thickening in the peripheral and mediastinal pleura and scissurae. No mediastinal or hilar lymphadenopathies are observed. The patient currently follows no type of treatment and only presents pulmonary and hepatic affectation with no central nervous system affectation.
Niemann-Pick disease was first described by Albert Niemann in 1914.4 It is an autosomal recessive lysosomal storage disorder.1 Its incidence in newborns is from 0.4 to 0.6/100,000.3 It is the result of an ASM deficiency and the accumulation of sphingomyelin,1 mainly in the central nervous system and the reticuloendothelial system5 in the form of lipid-laden macrophages known as “Niemann-Pick cells”.6 N-P disease entails two different entities in terms of metabolism and clinical symptoms, known as types A and B, with inherited deficiency of ASM activity and characterized by the accumulation of lipids in different tissues, especially the liver and spleen.6 Type C is a lipid storage disorder that is more complex due to the defect in intracellular cholesterol traffic,6 which is produced by a different genetic alteration.
Type A is a severe pediatric neurodegenerative disease with progressive psychomotor delay, failure to grow, hepatosplenomegaly and strawberry stains.2 Life expectancy is very short at 3–4 years for most.4
Type B does not seem to favor either of the sexes and it can become evident at any age, although it is most frequently seen before the age of 20.7 There is a chronic visceral affectation that develops slowly2 and presents a wide variability in the severity of the symptoms and the clinical findings.3 Hepatosplenomegaly is rather common, with splenic growth above all.1 Liver function is affected, with an increase in transaminases and bilirubin. Thrombocytopenia may appear, which could be secondary to infiltration of the bone marrow by N-P cells,8 and leucopenia may also be caused. Lung disease is frequent and in most patients alterations appear on chest radiographs or HRCT.1 The exact incidence of the lung affectation is difficult to determine, but it is rare in adults and more common in pediatric forms.9 N-P cells accumulate in the alveolar septa, bronchial walls and pleura, and they cause a restrictive pattern that progressively worsens, which may lead to respiratory failure1 with oxygen dependence and/or reduced tolerance to physical exercise.10 Respiratory function tests show the said restrictive pattern with an incapacity for gas exchange, and cycle ergometry is abnormal in half of the patients.3 The radiological findings are determined by the existence of reticulonodular pattern with thickening of the interlobular septa, ground glass opacities and sometimes millimetric nodules that may be calcified.2,8,10 Occasionally, the combination of these findings produces an HRCT image known as “crazy paving”, although these findings are not specific. The differential diagnosis of this pattern includes: pulmonary edema, pulmonary hemorrhage, lymphangitis, alveolar proteinosis, amyloidosis3 and non-specific interstitial pneumonia. Nevertheless, the association with hepatosplenomegaly should suggest deposition disease.2 There is a poor correlation between lung function tests and morphologic findings on HRCT, which implies that the interstitial changes do not always affect the gas exchange to a significant degree.3,10 Therefore, the presence of interstitial lung disease on the simple X-ray or HRCT is not necessarily a reliable indicator of the appearance of clinical symptoms or of the alteration in the respiratory function tests. For the study of the lung alterations in this disease, chest radiography as well as HRCT should be used.1 In our case, the lung affectation was demonstrated when the patient was 6 years old with the detection of a reticular pattern on simple chest radiograph, but to date the patient has not presented significant respiratory symptoms.
The diagnosis is done by the identification of N-P cells in bone marrow aspiration11 or instead by the demonstration of reduced ASM activity in isolated leucocytes and/or skin fibroblast culture. The molecular diagnosis is based on the identification of two ASM mutations causing the disease.10
There is currently no specific treatment available for ASM deficiency. Enzyme substitution therapy and gene therapy could be useful for patients with type B disease.3,4
Our case presents the majority of the radiological lung findings described in the literature with the presence of crazy paving with apical-basal gradient. The respiratory function tests did not correlate with the morphological alterations observed on HRCT as the respiratory tests were practically normal. Therefore, we believe that although N-P disease is a rare disease that presents non-specific radiological alterations, these can support the initial diagnosis and its confirmation. When confronted with a lipid storage disorder or a deposition disease, lung affectation must always be contemplated, and the most reliable radiological technique is HRCT.5 Although the crazy paving pattern is not the most specific for this type of disease, it should be included in the differential diagnosis, in accordance with what has been previously stated in the literature.5,10
Please cite this article as: Castañón Martínez R, et al. Afectación pulmonar en paciente adulto con enfermedad de Niemann-Pick tipo B. Arch Bronconeumol. 2012; 48:213-5.