There is some controversy about the effect of continuous positive airway pressure (CPAP) on the incidence of cardiovascular events (CVE). However, the incidence of CVE among patients with both obstructive sleep apnea (OSA) ans resistant hypertension (HR) has not been evaluated. Our objective was to analyze the long-term effect of CPAP treatment in patients with RH and OSA on the incidence of CVE.
MethodsMulti-center, observational and prospective study of patients with moderate-severe OSA and RH. All the patients were followed up every 3–6 months and the CVE incidence was measured. Patients adherent to CPAP (at least 4h/day) were compared with those with not adherent or those who had not been prescribed CPAP.
ResultsValid data were obtained from 163 patients with 64 CVE incidents. Treatment with CPAP was offered to 82%. After 58 months of follow-up, 58.3% of patients were adherent to CPAP. Patients not adherent to CPAP presented a non-significant increase in the total CVE incidence (HR:1.6; 95%CI: 0.96–2.7; p=0.07). A sensitivity analysis showed that patients not adherent to CPAP had a significant increase in the incidence of cerebrovascular events (HR: 3.1; CI95%: 1.07–15.1; p=0.041) and hypertensive crises (HR: 5.1; CI95%: 2.2–11.6; p=0.006), but the trend went in the opposite direction with respect to coronary events (HR: 0.22; CI95%: 0.05–1.02; p=0.053).
ConclusionsIn patients with RH and moderate-severe OSA, an uneffective treatment with CPAP showed a trend toward an increase in the incidence of CVE (particularly neurovascular events and hypertensive crises) without any changes with respect to coronary events.
Existe cierta controversia sobre el efecto de la presión positiva continua en las vías respiratorias (CPAP) sobre la incidencia de eventos cardiovasculares (ECV). Sin embargo, no se ha evaluado la incidencia de ECV en los pacientes con apnea obstructiva del sueño (AOS) e hipertensión resistente (HR). Nuestro objetivo fue analizar el efecto a largo plazo del tratamiento con CPAP en pacientes con HR y AOS en la incidencia de ECV.
MétodosEstudio multicéntrico, observacional y prospectivo de pacientes con AOS y HR. Cada paciente acudió a revisión cada 3-6 meses y se midió la incidencia de ECV. Se compararon los pacientes con buena adherencia a la CPAP (al menos 4h/día) con aquellos con mala adherencia o aquellos a quienes no se les había indicado la CPAP.
ResultadosSe obtuvieron datos válidos de 163 pacientes con 64 eventos de ECV. Se ofreció tratamiento con CPAP al 82%. Después de 58 meses de seguimiento, el 58,3% de los pacientes presentaron buena adherencia a la CPAP. Los pacientes con mala adherencia o sin prescripción de CPAP presentaron un aumento no significativo en la incidencia total de ECV (HR: 1,6; IC 95%: 0,96-2,7; p=0,07). Un análisis de sensibilidad mostró que los pacientes con mala adherencia a la CPAP tuvieron un aumento significativo en la incidencia de eventos cerebrovasculares (HR: 3,1; IC 95%: 1,07-15,1; p=0,041) y crisis hipertensivas (HR: 5,1; IC 95%: 2,2-11,6; p=0,006), pero la tendencia fue en la dirección opuesta con respecto a los eventos coronarios (HR: 0,22; IC 95%: 0,05-1,02; p=0,053).
ConclusionesEn pacientes con HR y AOS moderada o grave, un tratamiento ineficaz con CPAP mostró una tendencia hacia un aumento en la incidencia de ECV (particularmente eventos neurovasculares y crisis hipertensivas), sin ningún cambio con respecto a los eventos coronarios.
Obstructive sleep apnea (OSA) has demonstrated a negative impact on blood pressure (BP) readings1 and the incidence cardiovascular events (CVE).2 Various pathophysiological explanations have been offered for this association.3
Although it would be logical to suppose that the elimination of these respiratory events by treatment with continuous positive airway pressure (CPAP) would lead to a reduction in the incidence of CVE, the results in the literature are uneven. These results basically depend on the type of methodology used, the type of CVE studied, and the type of population included in the study.4–16
Patients with resistant hypertension (RH) – defined as the hypertension that remains uncontrolled despite the administration of three antihypertensive drugs, including a diuretic at optimal doses or those that requires at least four drugs to be controlled – present a high cardiovascular risk,17–21 as well as a high prevalence of OSA.22 CPAP treatment in these patients has proved capable of bring down BP readings to a clinically significant degree,23,24 but no study to date has demonstrated whether long-term CPAP treatment results in a reduction in CVE in these patients.
The objective of our study was to assess whether long-term CPAP treatment in patients with RH alters the incidence of CVE (both fatal and non-fatal).
Material and methodsStudy designThis was an observational, multicenter (24 centers) and prospective study of a series of patients diagnosed with RH who presented moderate-to-severe OSA (apnea–hypopnea index [AHI] ≥15events/h). All the patients signed their informed consent to participate. This study was approved by the ethics committee of the main research center (number 48/2008. Hospital General Universitario de Valencia).
The HIPARCO randomized control trial study23Throughout 2012–2013, 194 patients with a diagnosis of RH and moderate-to-severe OSA were randomized to receive CPAP or conservative treatment over three months. Patients with antecedents of cardiovascular risk factors were not excluded from the study (Appendix 1).
Selection of the patientsAll those patients who took part in the previously published HIPARCO study (clinicaltrials.gov Identifier: NCT00616265) were included in the present study (n=194).23 Those patients with no follow-up data on the incidence or otherwise of fatal or non-fatal CVE were excluded.
Follow-up after the HIPARCO studyOnce the HIPARCO study finished, the randomization of CPAP treatment also came to an end; each individual sleep and hypertension unit decided whether or not the patients were suited to CPAP treatment or any changes in medical treatment. All the patients eventually selected for CPAP treatment were subjected to a titration of CPAP pressure (Appendix 2).
In any case, all the patients were followed up in their respective sleep and hypertension units every 3–6 months, depending on the severity of their condition. Data on adherence to CPAP and antihypertensive treatment were collected in the same way as in the HIPARCO study, along with data on clinical changes and incidence of new CVE. The exclusion criteria and possible changes in treatment (including antihypertensive treatment) were also reevaluated.
The diagnoses and dates of the various fatal or non-fatal CVE reviewed on an individual basis at every medical consultation. They were taken into consideration only when objective proof of their occurrence was supplied by the corresponding specialists, either at the time of their occurrence or after a review of electronic hospital or out-patient records.
Main outcome measuresThe main outcome was the incidence of new fatal or non-fatal CVE, including transient ischemic attack (TIA), stroke, acute myocardial infarction (AMI), coronary revascularization, angina, atrial fibrillation, hypertensive crises, heart failure, and cardiovascular death.
Secondary outcomes included a separate analysis of other composite and individual outcomes: 1. Neurological outcomes (stroke+TIA+neurological death); 2. Heart outcomes (AMI+angina/revascularization+coronary death); 3 heart failure; 4. Hypertensive crisis (defined as the elevation of systolic BP>179mmHg or diastolic BP>109mmHg25; 5. Atrial fibrillation.
Statistical analysisContinuous variables were expressed as mean (SD), while categorical variables were reported as absolute numbers and percentages. The normality of the distribution of variables was tested by means of the Kolmogorov–Smirnov test.
As no data are available on the incidence of CVE in RH patients, any difference in the incidence of CVE of at least 10% between the CPAP branches with and without adherence during the follow-up was used to calculate the sample size. Calculating a 10% loss of patients, a total incidence of 60 CVE was required to achieve a statistical power of 80% and an alpha error of 5%.
The characteristics of the groups that tolerated CPAP and those that did not (or were not prescribed it) were compared by means of a Student T, U Mann–Whitney or Chi squared test, depending on the type of variable and its distribution.
For each of the composite or individual CVE, the point of initial inclusion in the HIPARCO study, after confirmation of RH and OSA (in the case of non-prescription of CPAP), or the start of CPAP therapy (in the case of the treatment group) were considered the entry point into the study. It was decided to end the follow-up in June 2018, once the sample size required for total CVE (main outcome) was achieved. The follow-up period for composite outcomes ended with the first appearance of one of the CVE on the list of those defined by the composite, while the analysis of each individual CVE ended at the point at which the first CVE of this specific type occurred.
In order to compare the incidence of CVE, in both composite and individual forms, between the group adherent to CPAP and non-adherent (or non-prescription) group, the corresponding Kaplan Meier curves were constructed with a log-rank test for between-group comparison. Finally, a multivariate Cox analysis was used for each endpoint to adjust for the variables that the researchers considered clinically justified for the corresponding endpoint. A two-sided p value of less than 0.05 was considered significant. Data management and statistical analyses were performed using Stata, version 11, and SPSS predictive analytics software (IBM), version 21.
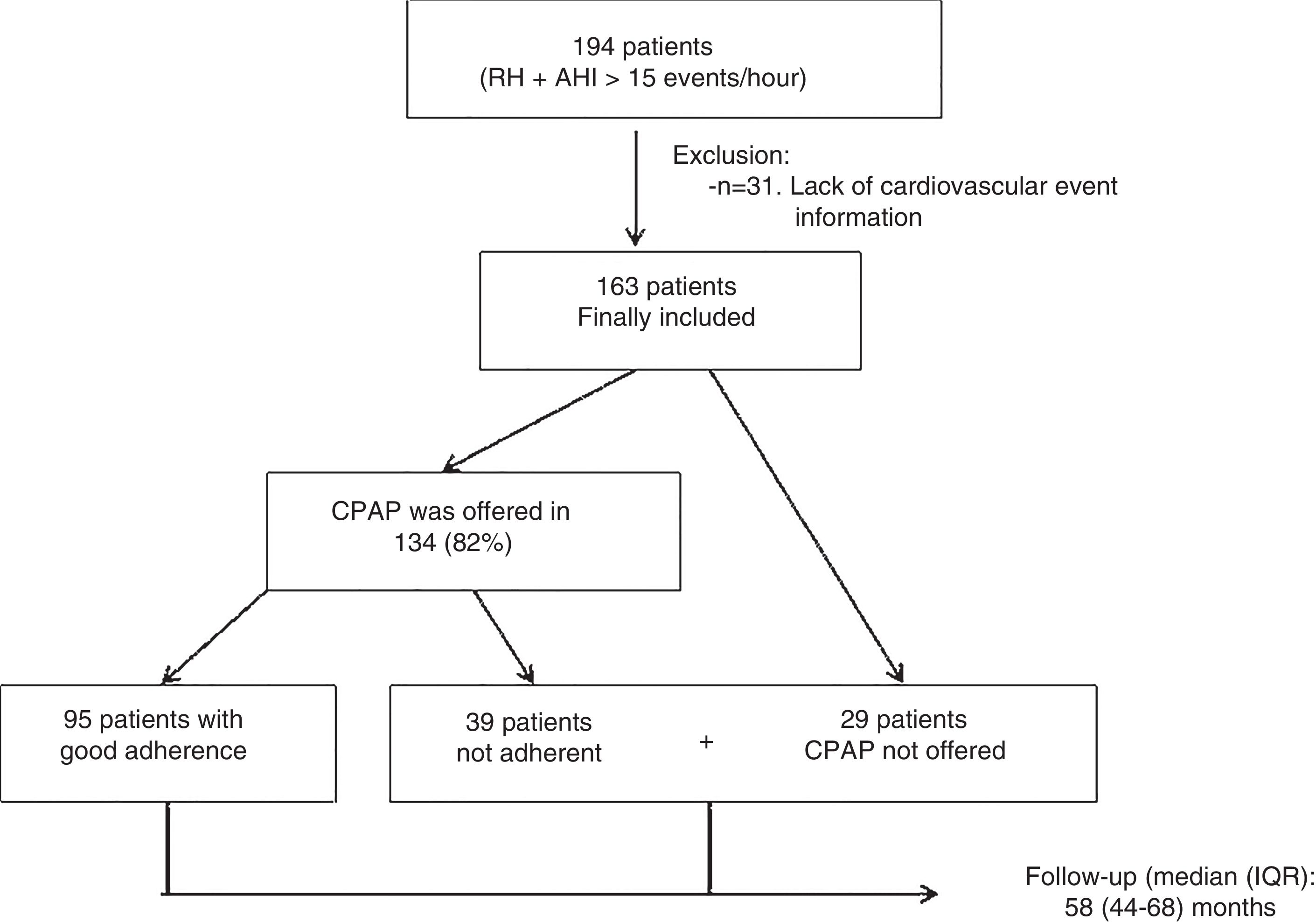
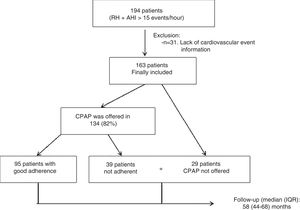
ResultsOf the 194 initial patients, 31 patients lacked information about their follow-up and so they were ruled out for the analysis, which finally covered 163 patients (Fig. 1). CPAP was offered to 82% of the patients. The average use of CPAP treatment during the follow-up (objectively measured by the internal counter of every device) was 5.1 (1.8)h per night, with 95 patients (58.3%) using it at least 4h per night during the follow-up and 38% using it at least 6h per night. The mean CPAP pressure used was 9.1 (1.8) mmHg. The residual AHI following the application of CPAP during the titration study was 3.9 (3.4) mmHg. The patients were followed up for a median of 58 months (interquartile range of 44–68 months). There were 12 deaths (7.4%; 10 of cardiovascular origin). There were no differences in terms of age, gender, clinical picture, cardiovascular risk factors, number of antihypertensive drugs or polygraphic variables between those patients who were offered CPAP (n=134; 82%) and those without prescription of this treatment (n=29; 18%).
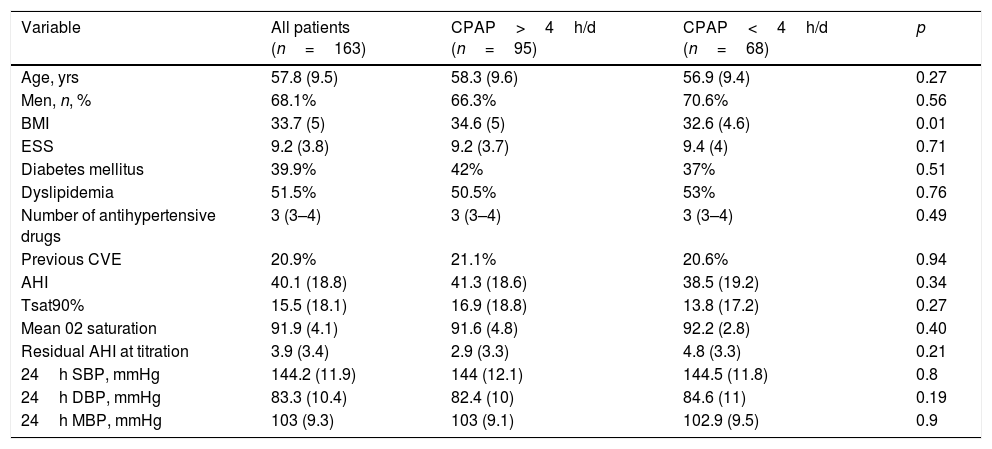
Table 1 shows the patients’ general characteristics, along with the comparison between those who tolerated CPAP and those who did not (or were not prescribed it). The mean age was 57.8 (9.5) years and 68.1% of the patients were male. BMI was 33.7 (5), AHI 40.1 (18.8) (96.6% obstructive), and the mean Epworth score was 9.2 (3.8). The median (IQR) of antihypertensive drugs taken was 3 (3–4). No significant changes were observed in the BMI over the course of the follow-up (33.6 [5] vs 33.5 [5], p=0.2]). Those patients who tolerated CPAP treatment presented a significantly higher BMI than the group that did not tolerate (or were not offered) CPAP. There were no differences in any of the other variables that were analyzed.
Characteristics of the patients included and comparisons between those adherent to CPAP treatment and those who were not adherent to (or were not offered) CPAP.
| Variable | All patients (n=163) | CPAP>4h/d (n=95) | CPAP<4h/d (n=68) | p |
|---|---|---|---|---|
| Age, yrs | 57.8 (9.5) | 58.3 (9.6) | 56.9 (9.4) | 0.27 |
| Men, n, % | 68.1% | 66.3% | 70.6% | 0.56 |
| BMI | 33.7 (5) | 34.6 (5) | 32.6 (4.6) | 0.01 |
| ESS | 9.2 (3.8) | 9.2 (3.7) | 9.4 (4) | 0.71 |
| Diabetes mellitus | 39.9% | 42% | 37% | 0.51 |
| Dyslipidemia | 51.5% | 50.5% | 53% | 0.76 |
| Number of antihypertensive drugs | 3 (3–4) | 3 (3–4) | 3 (3–4) | 0.49 |
| Previous CVE | 20.9% | 21.1% | 20.6% | 0.94 |
| AHI | 40.1 (18.8) | 41.3 (18.6) | 38.5 (19.2) | 0.34 |
| Tsat90% | 15.5 (18.1) | 16.9 (18.8) | 13.8 (17.2) | 0.27 |
| Mean 02 saturation | 91.9 (4.1) | 91.6 (4.8) | 92.2 (2.8) | 0.40 |
| Residual AHI at titration | 3.9 (3.4) | 2.9 (3.3) | 4.8 (3.3) | 0.21 |
| 24h SBP, mmHg | 144.2 (11.9) | 144 (12.1) | 144.5 (11.8) | 0.8 |
| 24h DBP, mmHg | 83.3 (10.4) | 82.4 (10) | 84.6 (11) | 0.19 |
| 24h MBP, mmHg | 103 (9.3) | 103 (9.1) | 102.9 (9.5) | 0.9 |
BMI: Body mass index; ESS: Epworth Sleepiness Scale; CVE: Cardiovascular events; AHI: Apnea–hypopnea index; Tsat90%: Night-time with oxygen saturation below 90%; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; MBP: Mean Blood Pressure.
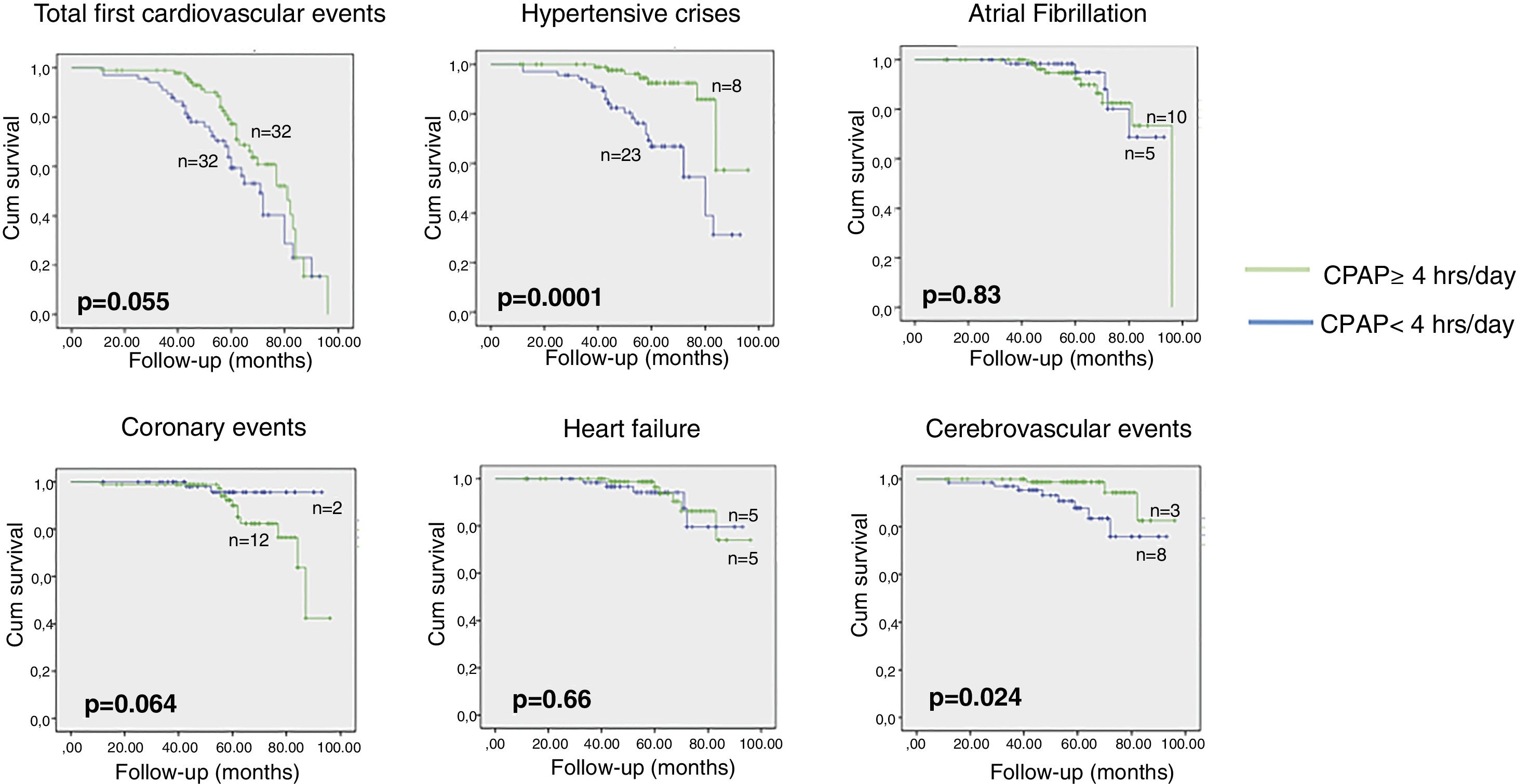
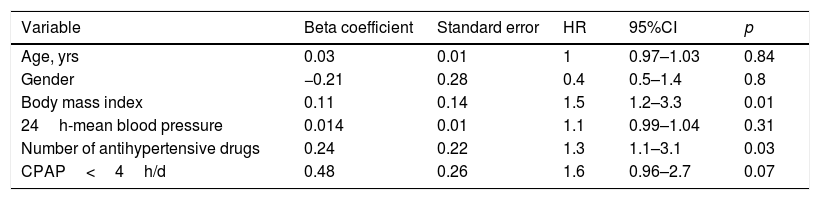
A total of 64 first CVE were observed, 32 CVE in each of the group studied in terms of adherence to CPAP. Those patients adherent to CPAP tended to present a lower total incidence of CVE (Fig. 2), and this remained the case after adjustment for clinically relevant confounders such as age, gender, and BMI (HR 1.6 [IC95%: 0.96–2.7; p=0.07) (Table 2). Both a higher BMI and a need for a greater number of antihypertensive drugs were significantly related to a higher total incidence of CVE. The results did not significantly change when 5 or 6h were used as cut-off points to define adherence to CPAP.
Cox regression. Factors associated with the presence of a new cardiovascular event (total number).
| Variable | Beta coefficient | Standard error | HR | 95%CI | p |
|---|---|---|---|---|---|
| Age, yrs | 0.03 | 0.01 | 1 | 0.97–1.03 | 0.84 |
| Gender | −0.21 | 0.28 | 0.4 | 0.5–1.4 | 0.8 |
| Body mass index | 0.11 | 0.14 | 1.5 | 1.2–3.3 | 0.01 |
| 24h-mean blood pressure | 0.014 | 0.01 | 1.1 | 0.99–1.04 | 0.31 |
| Number of antihypertensive drugs | 0.24 | 0.22 | 1.3 | 1.1–3.1 | 0.03 |
| CPAP<4h/d | 0.48 | 0.26 | 1.6 | 0.96–2.7 | 0.07 |
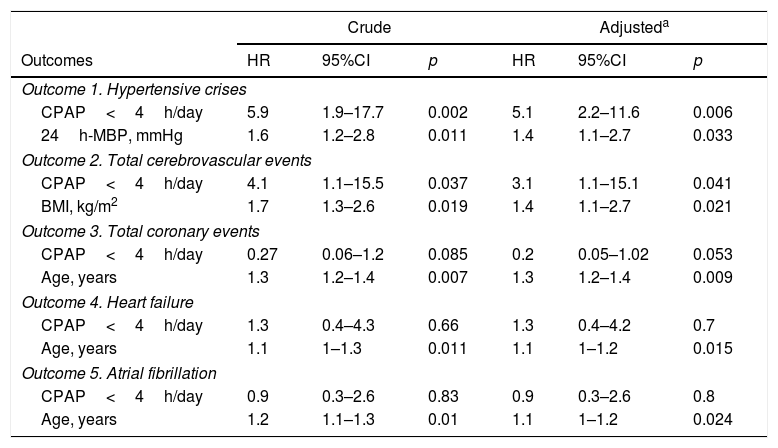
There were 11 new cerebrovascular events, 8 in the group not adherent to CPAP and 3 in the group adherent to CPAP. The latter patients presented a significant reduction in the incidence of these events, even after adjustment for age, gender, and BMI (HR 3.1 [1.07–15.1; p=0.041) (Fig. 2, Table 3).
Cox regression. Factors associated with the presence of a new cardiovascular event (composite or individual).
| Crude | Adjusteda | |||||
|---|---|---|---|---|---|---|
| Outcomes | HR | 95%CI | p | HR | 95%CI | p |
| Outcome 1. Hypertensive crises | ||||||
| CPAP<4h/day | 5.9 | 1.9–17.7 | 0.002 | 5.1 | 2.2–11.6 | 0.006 |
| 24h-MBP, mmHg | 1.6 | 1.2–2.8 | 0.011 | 1.4 | 1.1–2.7 | 0.033 |
| Outcome 2. Total cerebrovascular events | ||||||
| CPAP<4h/day | 4.1 | 1.1–15.5 | 0.037 | 3.1 | 1.1–15.1 | 0.041 |
| BMI, kg/m2 | 1.7 | 1.3–2.6 | 0.019 | 1.4 | 1.1–2.7 | 0.021 |
| Outcome 3. Total coronary events | ||||||
| CPAP<4h/day | 0.27 | 0.06–1.2 | 0.085 | 0.2 | 0.05–1.02 | 0.053 |
| Age, years | 1.3 | 1.2–1.4 | 0.007 | 1.3 | 1.2–1.4 | 0.009 |
| Outcome 4. Heart failure | ||||||
| CPAP<4h/day | 1.3 | 0.4–4.3 | 0.66 | 1.3 | 0.4–4.2 | 0.7 |
| Age, years | 1.1 | 1–1.3 | 0.011 | 1.1 | 1–1.2 | 0.015 |
| Outcome 5. Atrial fibrillation | ||||||
| CPAP<4h/day | 0.9 | 0.3–2.6 | 0.83 | 0.9 | 0.3–2.6 | 0.8 |
| Age, years | 1.2 | 1.1–1.3 | 0.01 | 1.1 | 1–1.2 | 0.024 |
MBP: Mean blood pressure; BMI: Body mass index.
Similarly, a total of 31 hypertensive crises were observed (23 in the non-adherent group), which represented a significant drop in the group adherent to CPAP, even after adjusting for the initial values of MBP (mean BP), number of antihypertensive drugs required, age, gender, and BMI (HR 5.1 (2.2–11.6; 0.006) (Fig. 2, Table 3).
Long-term effect of CPAP on ischemic heart disease eventsNo significant differences were observed between the two groups, however, in the total number of coronary events (12 in the group adherent to CPAP and 2 in the non-adherent group) (HR 0.22 [0.05–1.02]; p=0.053) (Fig. 2, Table 3).
Long-term effect of CPAP on other cardiovascular endpointsFinally, no significant differences were observed between the two groups in the incidence of cardiac arrhythmias along the lines of atrial fibrillation (5 in the group not adherent and 10 in the group adherent to CPAP; HR 0.9) or in new diagnoses of heart failure (5 in the group not adherent to CPAP and 5 in the adherent group; HR 1.3) (Fig. 2, Table 3).
DiscussionThis the first study to analyze the long-term effect of CPAP treatment on the incidence of CVE in patients with RH and OSA. According to our results, no reduction was observed, after a follow-up of approximately 5 years, in the overall incidence of CVE, even after adjusting the results for clinically significant confounders. Other notable findings were obtained, however: a significant drop in the number of hypertensive crises and cerebrovascular events (both fatal and not-fatal), and no changes in the incidence of coronary events in the group adherent to CPAP.
The effect of CPAP treatment on the incidence of CVE is an issue that continues to arouse great controversy.4–16 In the studies that we have analyzed, the results are dependent on various factors, such as the type of study (clinical trials are more negative); the adherence to CPAP; the type of event (a positive effect of CPAP is more usually found in cerebrovascular, as opposed to coronary events); and the type of population studied (CPAP tends to demonstrate a more positive effect in studies that include patients who have suffered an stroke, or who have a high risk of doing so, than in those that include patients who have had a coronary ischemic event, or have a high risk of doing so).16
Our study, the first to be undertaken on the long-term effect of CPAP on patients with RH and a high risk of both cerebrovascular and cardiovascular events, seems to follow similar lines. Thus, whereas no changes were observed in the overall incidence of CVE between the compared groups according to their adherence to CPAP, there was a difference between the overall incidence of coronary events and cerebrovascular events. These results could have various explanations. Firstly, the mechanisms regulating cerebral and coronary circulation in response to intermittent hypoxemia and its elimination could also be different in RH patients.26–32 Moreover, the effects of the different responses from the brain and heart to a significant drop in BP after CPAP are not inconsiderable. Sanchez de la Torre et al.33 found a significant variability in the BP decrease experienced by RH patients with moderate-to-severe OSA after CPAP treatment. A significant number of patients experience a drop in BP of more than 10mmHg, and it is possible to identify these subjects via the use of biomarkers. Therefore, an additional hypothesis that might contribute to explaining the results is that in those subjects with RH and OSA in whom CPAP treatment might lead to a significant decrease in BP (especially if the antihypertensive medications are not subsequently optimized), there is a possibility of an increased incidence of coronary events. This would occur because patients might experience an excessive BP drop at some point during the 24h (a BP drop under coronary perfusion pressure). This might be similar to the effect of the increase in coronary events that has been reported when an excessive BP drop occurs with drug treatment in subjects with high cardiovascular risk, known as the “J-curve phenomenon”.34,35 However, the latter hypothesis is purely speculative. Finally, there is a possibility that patients with RH and untreated OSA may achieve a status of protection from coronary events because they have developed an ischemic preconditioning state which means that their myocardium has adapted to continue functioning with a low level of oxygen. In contrast, this preconditioning state is lost with the CPAP treatment.
On the other, the reduction in the incidence of hypertensive crises – a known risk factor for a cerebrovascular event36 – observed in patients adherent to CPAP suggests that CPAP could play a protective role. It is therefore possible that the collation of all CVE (both coronary and cerebrovascular) for the composite that was our primary outcome (combined with the fact that coronary events were more frequent) meant that our results did not ultimately favor the group adherent to CPAP.16
The main strength of the present study is that it is the first to examine the long-term effect of CPAP on a group with a high cardiovascular risk, in this case RH, in a very well characterized series of patients coming from a recognized clinical study.
As regards the limitations of our study, it obviously should be stressed that it is not a clinical trial. Once the randomized HIPARCO clinical trial had come to an end,23 the randomization had to be terminated for ethical reasons, as a clinically significant improvement had been found in the BP readings. Therefore, although the patients were closely followed up, the study became observational and prospective, and it compared the group that tolerated CPAP with the one that did not, with all the well-known limitations of this methodology. Furthermore, although the total number of CVE corresponded with the calculation of the sample size, this was not true of the number of individual CVE of each type; this could trigger a type II error, and significant differences could go undetected when they are in fact present. This situation does, however, strengthen the conclusion that well-tolerated CPAP in RH patients can provide protection against cerebrovascular events and hypertensive crises, but this conclusion cannot be reached with regards to those associations that did not prove significant. Moreover we have no analyzed the impact of the changes in the antihypertensive treatment or the adherence to this treatment during follow-up and we have not performed 24h-ABPM or heart function measures at the end of follow-up in all patients. Finally, the adherence of CPAP was measured at the end of the study, so there was no continuous monitoring that allowed us to observe different patterns of adherence that could have an impact on the results of the study.
In conclusion, in our series of patients with RH and OSA, well-tolerated long-term treatment with CPAP did not modify the total incidence of CVE, although we did observe different patterns in the incidence of cerebrovascular events and hypertensive crises (which were significantly reduced) and that of coronary events (which were unchanged).
AuthorshipCNS, MAMG, FCR, GT and FB participated in the study's conception and design, supervised the study and wrote the manuscript.
MAMG and AM participated in the statistical analysis.
CNS, MST, CCE, PLL, TDC, MS, JFM, MG, EM, MP, FGR, JM, GO, AGO, TP, and FCR participated in the data collection.
All the other authors contributed to data acquisition and interpretation, critically revised the manuscript and approved the final version for publication.
MAMG is the guarantor of the paper.
Conflict of interestThe authors declare no conflict of interest.