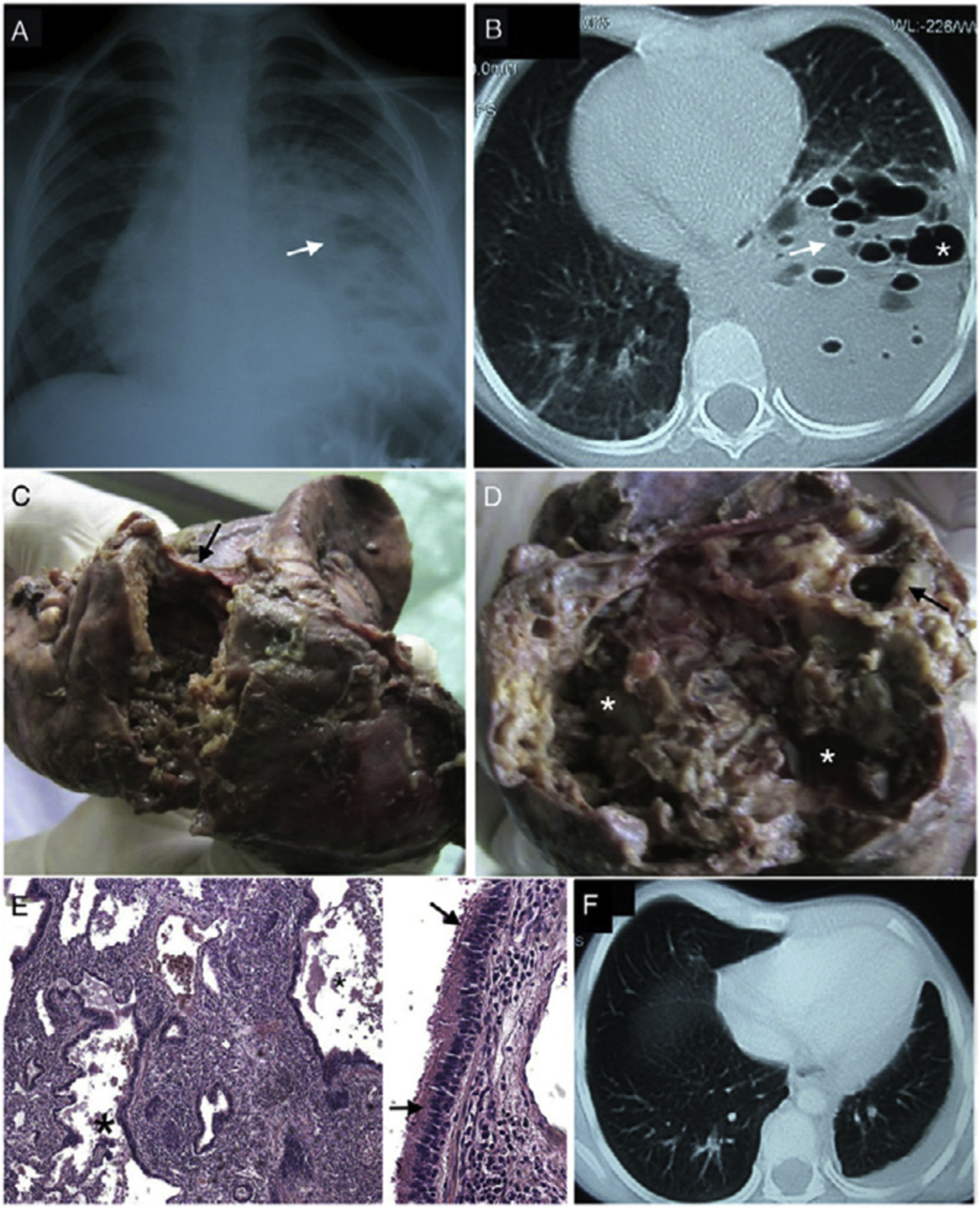
Our patient was a young girl, 6 years of age, with no prenatal check-ups or previous episodes of pneumonia. She was hospitalized for a 5-day history of signs and symptoms consistent with left basal pneumonia and mild respiratory distress. Chest X-ray showed pleural and parenchymal involvement of the left lower lobe (Fig. 1A). She was treated with broad-spectrum antibiotics. Serologies for echinococcus granulosus and tuberculous mycobacteria were negative. Clinical and radiological progress were unfavorable, so a chest computed tomography (CT) was performed (Fig. 1B), which suggested complicated pulmonary sequestration or congenital malformation. Surgical treatment (left lower lobectomy) was performed; the anatomical piece (Fig. 1C and D) had its own visceral pleura, with independent irrigation from a fine artery originating in the thoracic aorta, characteristic of extralobar pulmonary sequestration (EPS); the histopathological study (Fig. 1E) confirmed infected congenital cystic adenomatoid malformation (CCAM) type 2. Her subsequent progress was favorable, and a follow-up CT was performed at 6 months (Fig. 1F).
A) Anteroposterior chest X-ray shows right shift of the trachea and mediastinum, signs of air trapping, presence of a radiopaque image involving the left lower lobe, where multiple rounded radiolucent images (arrow), and left pleural effusion are seen. B) Chest CT shows solid-cystic lesion, without air bronchogram, with multiple cysts of variable size (arrow), from 5 to 15 mm, some converging to form larger cavities (asterisk). C and D) Gross examination found a specimen measuring 12 × 6 × 8 cm of friable tissue (arrow) with multiple cavities of varying size and purulent content (asterisk). E) Microscopy (H&E staining ×40) shows marked architectural alteration with multiple cystic formations (asterisks), the largest cystic formations (right, magnification ×100) being covered by a pseudostratified columnar epithelium (arrow) surrounded by thin fibromuscular walls and dense inflammatory infiltrate in the cystic and interstitial space, consistent with infected congenital cystic adenomatoid malformation type 2. F) Follow-up CT showing right and left upper lobe compensatory emphysema, and left posterior pleural and lateral thickening.
CCAM is a rare congenital abnormality with a prevalence of approximately 8–9/100,000.1,2 The association with EPS2 (hybrid form), as in the present case, is very rare, even more so in late presentation (older than 1 year of age). It is important for the clinician to be aware of the clinical and radiological course, and the differential diagnoses that include congenital (diaphragmatic hernia, pulmonary cysts, etc.) and infectious (necrotizing pneumonia, tuberculosis, abscess, and pulmonary hydatidosis) causes, in order to make an early diagnosis and provide timely treatment.2
Please cite this article as: Pumacayo-Cárdenas S, León-Bejarano E, Recabarren-Lozad A. Malformación pulmonar congénita compleja de diagnóstico tardío: de la clínica y radiología a la histopatología. Arch Bronconeumol. 2020;56:523.