Invasive aspergillosis occurs frequently in immunocompromised patients, primarily in patients with neutropenia or individuals receiving treatment with corticosteroids, antibiotics, or cytotoxic drugs,1 while it is uncommon in patients with preserved cell immunity. Several cases of fungal infection caused by Aspergillus have been described in recent years, and this is a complication that should be taken into account in patients who present a pneumonic process during the course of an influenza virus infection.2
We report the case of a patient with influenza virus infection who developed invasive aspergillosis as a complication that caused his death.
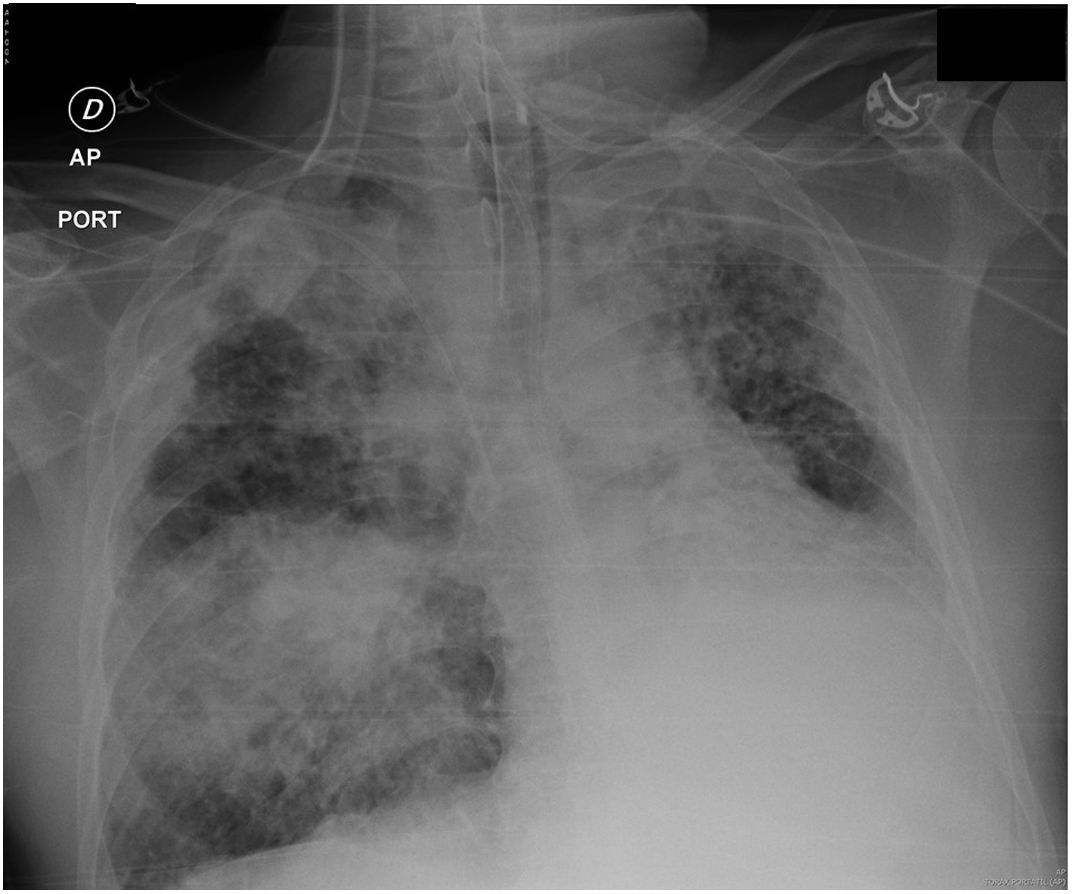
A 50-year-old patient diagnosed with common variable immunodeficiency receiving treatment with intravenous immunoglobulins every 3 weeks, clinically stable, with no significant infections in the last 3 years, consulted his primary care physician with irritative cough, high fever, and dyspnea. He was treated with levofloxacin without improvement, so he attended the emergency room. Physical examination showed BP 133/85, pulse 111beats per minute, 20breaths per minute, no fever. Immunoglobulin serum values: IgA: 0g/l; IgG: 7.05g/l; IgM: 0.73g/l. The chest X-ray showed loss of left volume and images of bilateral bronchiectasis without radiological changes. The patient was admitted for respiratory failure. PCR of pharyngeal exudate was positive for influenza virus (H3N2), so treatment began with systemic corticosteroids and oseltamivir, with the addition of piperacillin/tazobactam and intravenous amikacin. After an initial improvement, the patient deteriorated on day 5 of admission with tachypnea, tachycardia, and the appearance of a right basal pulmonary condensation on radiology (Fig. 1), so he was transferred to the intensive care unit, requiring intubation and invasive ventilation. Linezolid and intravenous colistin were added to his regimen. Bronchoscopy was performed, showing images of whitish membranes in the bronchial tree in both sides. Bronchial aspirate and bronchoalveolar lavage showed countless colonies of Aspergillus fumigatus and Aspergillus terreus sensitive to voriconazole and amphotericin B. Galactomannan testing in bronchoalveolar lavage and blood was negative. Treatment with voriconazole was added, with little improvement. Amphotericin B was then administered, and the patient developed refractory shock and acute respiratory distress syndrome, which caused his death.
The most frequently described complications in patients with influenza virus infection are acute respiratory distress, bacterial superinfection, the selection of oseltamivir-resistant strains, and pulmonary hemorrhage, which can lead to a poor outcome in immunocompromised patients.1 It is unusual to think of Aspergillus as a pathogen capable of causing invasive disease in patients with viral infection, yet since 2010 several cases of influenza virus infection complicated by post-onset invasive aspergillosis have been reported. Influenza virus infection, then, appears to be a new risk factor for invasive fungal infection.
Pathogenesis may be a result of the influenza virus (and the H1N1 virus more frequently) causing severe and diffuse damage to the respiratory mucosa, disrupting the respiratory mucosa, and altering normal ciliary clearance,3–5 thus permitting invasion by the fungus. The virus can also damage local defenses against Aspergillus, alter local phagocytosis produced by alveolar macrophages, and reduce the functionality of natural killer cells and other immune responses.6,7 A recent publication found that the virus also damages pulmonary and systemic levels of cytokines and the function of pulmonary phagocytes, producing a state of immune deficiency.8,9
When influenza virus infection is complicated by fungal co-infection, mortality is approximately 50%–60%, 5 times higher than in hospitalized patients with viral infection only.3,10 In the series published by Van de Veerdonk et al.,11 invasive aspergillosis mortality in influenza patients was 55%. Absence of suspicion, the interference of the underlying influenza virus infection, and the limited use of serological diagnostic methods prevent early diagnosis, delay treatment, and lead to increased mortality.
Despite high mortality rates, this association is not routinely reported.12 The isolation of Aspergillus spp. observed in cultures obtained from bronchoscopic samples of patients admitted to the ICU with influenza virus infection can thus be underestimated, and they may be considered contaminants despite their potential to cause invasive disease. The presence of structural lung disease, high doses of corticosteroids, and T cell deficiencies during influenza virus infection may be responsible for an emerging group of patients at high risk of invasive aspergillosis.
According to Wauters et al.,13 steroid use within 7 days prior to ICU admission was an independent risk factor for fungal coinfection. Patients with influenza treated with corticosteroids before or after admission to the ICU should be carefully evaluated for possible Aspergillus coinfection; the authors suggest that systemic steroids should be avoided in patients with influenza, even in those who develop acute respiratory distress associated with their influenza infection.
Our patient had common variable immunodeficiency treated with immunoglobulins, with normal immunoglobulin values except IgA, and no infections in recent years. The infections most frequently described in these patients are bacterial infections (otitis, sinusitis, pneumonia, diarrhea, etc.) associated with humoral immunity deficiencies, which play a lesser role in invasive aspergillosis than the more important cell immunity.14
The interest of this scientific letter is that it draws attention to the increased risk of invasive aspergillosis in patients with influenza virus infection (most often H1N1). In patients with worsening symptoms, a chest CT scan and bronchoscopy should be performed early to ensure early diagnosis and treatment of invasive aspergillosis if there are signs indicating its presence. Taking into account the results published in the literature, Aspergillus species in the respiratory cultures of critically ill patients, particularly those with influenza virus infection, should not necessarily be considered contaminants or colonizers. Early diagnosis and treatment strategies should be initiated in these patients and multicenter studies should be carried out to better define the incidence and outcome of this disease.12,15
Please cite this article as: García Clemente M, Martín Iglesias L, Enríquez Rodríguez AI, Iscar Urrutia M, Madrid Carbajal C, López González FJ. Aspergilosis invasora como complicación de infección por virus influenza H3N2. Arch Bronconeumol. 2020;56:406–408.